History
Current Medications
Comments
Current Symptoms
Physical Examination
Comments
Laboratory Data
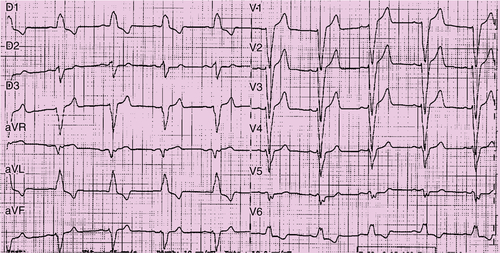
FIGURE 23-1 Baseline electrocardiogram with sinus rhythm and left bundle branch block.
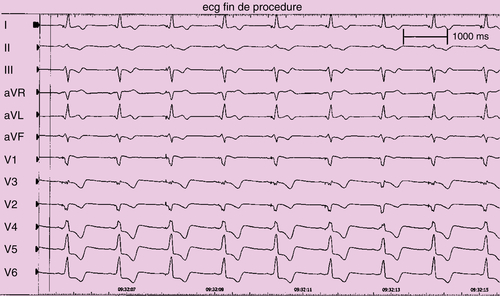
FIGURE 23-2 Surface electrocardiogram with biventricular pacing, with the bipolar lead positioned at the proximal portion of the lateral vein (see Figure 23-1).
Comments
Electrocardiogram
Findings
Chest Radiograph
Findings
Comments
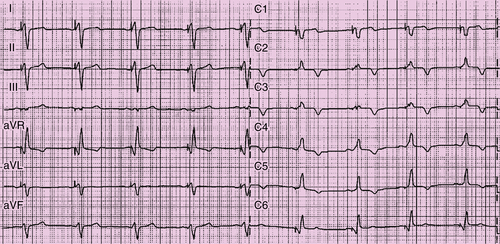
FIGURE 23-3 Final surface electrocardiogram with biventricular pacing with left ventricular pacing configuration M4 (proximal pole) to right ventricular coil.
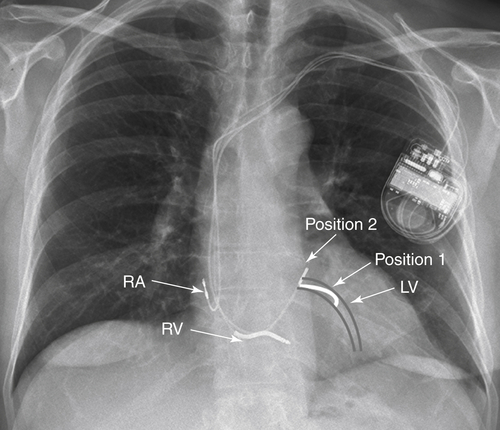
FIGURE 23-4 Left ventricular (LV) projection of the lateral vein. Position 1: Position of the LV lead at the end of the implantation. Position 2: Position of the LV lead the day after into the body of the coronary sinus. RA, Right atrial; RV, right ventricular.
Focused Clinical Questions and Discussion Points
Question
Discussion
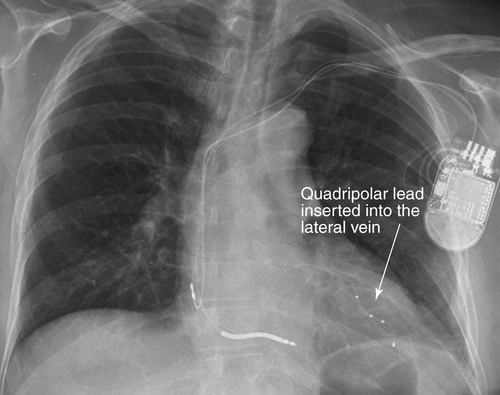
FIGURE 23-5
Question
Discussion
Question
Discussion
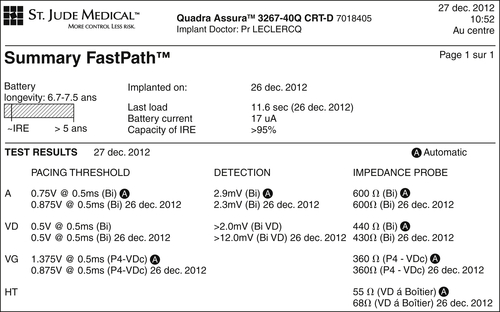
FIGURE 23-6 Summary of the pacing threshold, sensing, and impedances.
Final Diagnosis
Plan of Action
Intervention
Outcome
Selected References
1. Forleo G.B., Della Rocca D.G., Papavasileiou L.P. et al. Left ventricular pacing with a new quadripolar transvenous lead for CRT: early results of a prospective comparison with conventional implant outcomes. Heart Rhythm. 2011;8:31–37.
2. Landolina M., Gasparini M., Lunati M. et al. Long-term complications related to biventricular defibrillator implantation: rate of surgical revisions and impact on survival: insights from the Italian Clinical Service Database. Circulation. 2011;123:2526–2535.
3. Thibault B. et al. Posters PO 04-117 to 04-183. Heart Rhythm. 2011;8 S291.






