Chest Tube Removal (Perform)
Chest Tube Removal (Perform)
PREREQUISITE NURSING KNOWLEDGE
• Chest tubes are placed in the pleural or mediastinal space to evacuate an abnormal collection of air or fluid or both.
• Indications for removal are based on the reason for insertion and include the following:
 Drainage has decreased to 50 to 200 mL in prior 24 hours if tube was placed for hemothorax, empyema, or pleural effusion.
Drainage has decreased to 50 to 200 mL in prior 24 hours if tube was placed for hemothorax, empyema, or pleural effusion.
 Research has shown that, depending on the reason for the chest tube, volumes of 200 to 450 mL/day do not adversely affect length of stay or overall costs when compared with lower threshold volumes, nor does the risk of pleural fluid reaccumulation increase.5,21
Research has shown that, depending on the reason for the chest tube, volumes of 200 to 450 mL/day do not adversely affect length of stay or overall costs when compared with lower threshold volumes, nor does the risk of pleural fluid reaccumulation increase.5,21
 Drainage has changed from bloody to serosanguineous, no air leak is present, and amount is less than 100 mL in the past 8 hours (if tube was placed after cardiac surgery).1,9
Drainage has changed from bloody to serosanguineous, no air leak is present, and amount is less than 100 mL in the past 8 hours (if tube was placed after cardiac surgery).1,9
 Lungs are reexpanded (as shown on chest radiographic results).
Lungs are reexpanded (as shown on chest radiographic results).
 Respiratory status has improved (i.e., nonlabored respirations, equal bilateral breath sounds, absence of shortness of breath, decreased use of accessory muscles, symmetrical respiratory excursion, and respiratory rate less than 24 breaths/min).
Respiratory status has improved (i.e., nonlabored respirations, equal bilateral breath sounds, absence of shortness of breath, decreased use of accessory muscles, symmetrical respiratory excursion, and respiratory rate less than 24 breaths/min).
 Fluctuations are minimal or absent in the water-seal chamber of the collection device, and the level of solution rises in the chamber.
Fluctuations are minimal or absent in the water-seal chamber of the collection device, and the level of solution rises in the chamber.
• Air leaks have resolved for at least 24 hours (the absence of continuous bubbling in the water-seal chamber or absence of air bubbles from right to left in the air leak detector), and lung is fully reinflated on chest radiographic results.
• The air leak detector should bubble gently immediately on insertion of the chest tube during expiration and with coughing. Continuous bubbling in the air leak detector indicates a leak in the patient or the chest drainage system. Fluctuations in the water level (also known as tidaling) in the water-seal chamber of 5 to 10 cm, rising during inhalation and falling during expiration, should be observed with spontaneous respirations. If the patient is on mechanical ventilation, the pattern of fluctuation is just the opposite. Any suction applied must be disconnected temporarily to assess correctly for fluctuations in the water-seal chamber.
• Pleural tubes are placed after cardiac surgery if the pleural cavity has been entered. They typically are removed within 24 to 48 hours after surgery.1,9
• Mediastinal chest tubes most often are removed 24 to 36 hours after cardiac surgery.1
• Flexible Silastic (Blake) (Ethicon, Inc, Somerville, NJ) drains may be used in place of large-bore chest tubes in the mediastinal and pleural spaces after cardiac surgery. These tubes provide more efficient drainage and improved patient mobility with minimized tissue trauma and pain with removal.3,7,17 Pleural tubes placed for reasons other than postcardiac surgery necessity remain until the patient no longer needs them (i.e., no persistent air leak, stoppage of ongoing fluid leak or bleeding, or reexpansion of lung on chest radiograph).
• Chest radiographs are done periodically to determine whether the lung has reexpanded. Daily chest radiographs are not necessary while the tube is in place.10 Reexpanded lungs, along with respiratory assessments that show improvement in the patient’s respiratory status, are the basis for the decision to remove the chest tube.
• While the tubes are in place, patients may have related discomfort. Prompt removal of chest tubes encourages patients to increase ambulation and respiratory measures to improve lung expansion after surgery (e.g., coughing, deep breathing). However, removal of the chest tube may also be a painful procedure for the patient.4,8,15,16
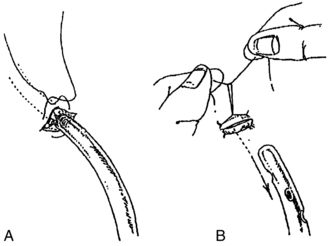
• The types of sutures used to secure chest tubes vary according to the preference of the physician, the physician assistant, or the advanced practice nurse. One common type is the horizontal mattress or purse-string suture, which is threaded around and through the wound edges in a U-shape with the ends left unknotted until the chest tube is removed. Usually, one or two anchor stitches accompany the purse-string suture (Fig. 22-1).
• A primary goal of chest tube removal is removal of tubes without introduction of air or contaminants into the pleural space.
EQUIPMENT
• Antiseptic swabs (povidone-iodine, chlorhexidine gluconate with alcohol, etc)6
• Petrolatum gauze, as per hospital protocol
• Rubber-tipped Kelly clamps (two per chest tube) or disposable umbilical clamps
• Wide occlusive tape (2-inch)
• Elastic closure device, such as Steri-Strips (3M, St. Paul, MN)
• Dry 4 × 4 gauze sponges (two to four)
• Personal protective equipment (goggles, sterile and nonsterile gloves, mask, gown)
Additional equipment (to have available depending on patient need) includes the following:
PATIENT AND FAMILY EDUCATION
• Assess patient and family understanding of the procedure.  Rationale: This assessment identifies patient and family knowledge deficits concerning patient condition, procedure, expected benefits, and potential risks and allows time for questions to clarify information.
Rationale: This assessment identifies patient and family knowledge deficits concerning patient condition, procedure, expected benefits, and potential risks and allows time for questions to clarify information.
• Explain the procedure, reason for removal, and sensations to be expected.15,19,20 The most commonly reported sensations are pulling, pain or hurting, and burning.14  Rationale: This explanation decreases patient anxiety and enhances cooperation.
Rationale: This explanation decreases patient anxiety and enhances cooperation.
• Explain the patient’s role in assisting with removal. Explain that the patient should perform the Valsalva maneuver on the count of “3”. Have the patient practice the maneuver before the procedure.  Rationale: This explanation elicits patient cooperation and facilitates removal.
Rationale: This explanation elicits patient cooperation and facilitates removal.
• Instruct the patient to turn and reposition every 2 hours after the chest tube has been removed.  Rationale: This action prevents complications related to immobility and retained secretions.
Rationale: This action prevents complications related to immobility and retained secretions.
• Instruct the patient to cough and deep breathe after the chest tube has been removed, with splinting of the affected side or sternum (with mediastinal tubes).  Rationale: This action prevents respiratory complications associated with retained secretions. The application of firm pressure over the insertion site (i.e., splinting) decreases pain and discomfort.
Rationale: This action prevents respiratory complications associated with retained secretions. The application of firm pressure over the insertion site (i.e., splinting) decreases pain and discomfort.
• Instruct the patient about the availability of prescribed analgesic medication.  Rationale: Analgesics alleviate pain and facilitate coughing, deep breathing, and repositioning.8,16,20
Rationale: Analgesics alleviate pain and facilitate coughing, deep breathing, and repositioning.8,16,20
• Instruct the patient and family to report signs and symptoms of respiratory distress or infection immediately.  Rationale: Immediate reporting facilitates prompt intervention to relieve a recurrent pneumothorax or to treat an infection.
Rationale: Immediate reporting facilitates prompt intervention to relieve a recurrent pneumothorax or to treat an infection.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
 Oxygen saturation within normal limits
Oxygen saturation within normal limits
 Absence of shortness of breath
Absence of shortness of breath
 Decreased use of accessory muscles
Decreased use of accessory muscles
 Rationale: Assessment of respiratory status verifies the patient’s readiness for chest tube removal.
Rationale: Assessment of respiratory status verifies the patient’s readiness for chest tube removal.
• Assess chest tube drainage (less than 200 mL in 24 hours or less than 100 mL in 8 hours after cardiac surgery).1,5,9,21  Rationale: Assessment of drainage verifies patient readiness for chest tube removal.
Rationale: Assessment of drainage verifies patient readiness for chest tube removal.
• Assess for minimal or absence of air leak in the air leak detector zone or indicator.  Rationale: This assessment indicates whether the lung is reexpanded and whether or not air leak is present.
Rationale: This assessment indicates whether the lung is reexpanded and whether or not air leak is present.
• Evaluate chest radiographic results.  Rationale: Lung reexpansion indicates that need for chest tube is resolved.
Rationale: Lung reexpansion indicates that need for chest tube is resolved.
• Assess vital signs and (optional) arterial blood gases.  Rationale: Vital sign assessment indicates whether the patient can tolerate chest tube removal.
Rationale: Vital sign assessment indicates whether the patient can tolerate chest tube removal.
• Assess laboratory results for clotting capability and medications that may impact clotting.  Rationale: Low platelet levels or thrombolytic medications may precipitate excessive bleeding.18
Rationale: Low platelet levels or thrombolytic medications may precipitate excessive bleeding.18
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information. Anticipatory preparation may prepare patients for a better experience.15,19,20
Rationale: This communication evaluates and reinforces understanding of previously taught information. Anticipatory preparation may prepare patients for a better experience.15,19,20
• Administer premedication of adequate analgesics at least 20 minutes before the procedure. Alternatively, subfascial lidocaine may be injected into the chest tube tract. Slow deep-breathing relaxation exercises in addition to opioids have also been shown to further diminish pain sensation.8  Rationale: Intravenous morphine 4 mg 20 minutes before or ketorolac 30 mg 60 minutes before the procedure have been shown to have substantial relief of pain without excessive analgesia.16 Pain medication and relaxation exercises reduce the discomfort and anxiety experienced, which facilitates patient cooperation.8,15,16
Rationale: Intravenous morphine 4 mg 20 minutes before or ketorolac 30 mg 60 minutes before the procedure have been shown to have substantial relief of pain without excessive analgesia.16 Pain medication and relaxation exercises reduce the discomfort and anxiety experienced, which facilitates patient cooperation.8,15,16
• Time the removal procedure to occur at peak analgesic effect.  Rationale: This timing increases patient cooperation and decreases anxiety.16
Rationale: This timing increases patient cooperation and decreases anxiety.16
• Place the patient in the semi-Fowler’s position. Alternatively, place the patient on the unaffected side with the waterproof pad underneath the site.  Rationale: This position enhances accessibility to the insertion site of the chest tube and protects the bed from drainage.
Rationale: This position enhances accessibility to the insertion site of the chest tube and protects the bed from drainage.
References
1. Abramov, D, et al. Timing of chest tube removal after coronary artery bypass surgery. J Card Surg. 2005; 20:142–146.
![]() 2. Bell, RL, et al, Chest tube removal. end-inspiration or end-expiration. J Trauma 2001; 50:674–677.
2. Bell, RL, et al, Chest tube removal. end-inspiration or end-expiration. J Trauma 2001; 50:674–677.
3. Bjessmo, S, et al, Comparison of three different chest drainages after coronary artery bypass surgery. a randomised trial in 150 patients. Eur J Cardiothorac Surg 2007; 31:372–375.
4. Bruce, EA, Howard, RF, Franck, LS, Chest drain removal pain and its management. a literature review. J Clin Nurs 2008; 15:145–154.
5. Cerfolio, RJ, Bryant, AS. Results of a prospective algorithm to remove chest tubes after pulmonary resection with high output. J Thorac Cardiovasc Surg. 2008; 135(2):269–273.
6. Digison, MB. A review of anti-septic agents for pre-operative skin preparation. Plast Surg Nurs. 2007; 27(4):185–189.
![]() 7. Frankel, TL, et al. Silastic drains vs conventional chest tubes after coronary artery bypass. Chest. 2003; 124:108–113.
7. Frankel, TL, et al. Silastic drains vs conventional chest tubes after coronary artery bypass. Chest. 2003; 124:108–113.
8. Friesner, SA, Curry, DM, Moddeman, GR, Comparison of two pain-management strategies during chest tube removal. relaxation exercise with opioids and opioids alone. Heart Lung. 2006; 35(4):269–276.
![]() 9. Gercekoglu, H, et al. Effect of timing of chest tube removal on development of pericardial effusion following cardiac surgery. J Card Surg. 2003; 18(3):217–224.
9. Gercekoglu, H, et al. Effect of timing of chest tube removal on development of pericardial effusion following cardiac surgery. J Card Surg. 2003; 18(3):217–224.
10. Hendrikse, KA, et al. Low value of routine chest radiographs in a mixed medical surgical ICU. Chest. 2007; 132(3):823–828.
11. Khan, T, et al. Is routine chest radiograph following mediastinal drain removal after cardiac surgery useful. Eur J Cardiothorac Surg. 2008; 34(3):542–544.
![]() 12. Laws, D, Neville, E, Duffy, J. British Thoracic Society guidelines for the insertion of a chest drain. Thorax. 2003; 58(Suppl II):ii53–ii59.
12. Laws, D, Neville, E, Duffy, J. British Thoracic Society guidelines for the insertion of a chest drain. Thorax. 2003; 58(Suppl II):ii53–ii59.
![]() 13. Martino, K, et al. Prospective randomized trial of thoracostomy removal algorithms. J Trauma. 1999; 46:369–371.
13. Martino, K, et al. Prospective randomized trial of thoracostomy removal algorithms. J Trauma. 1999; 46:369–371.
![]() 14. Mimnaugh, L, et al. Sensations experienced during removal of tubes in acute postoperative patients. Appl Nurs Res. 1999; 12:78–85.
14. Mimnaugh, L, et al. Sensations experienced during removal of tubes in acute postoperative patients. Appl Nurs Res. 1999; 12:78–85.
![]() 15. Puntillo, K, et al, Patients’ perceptions and responses to procedural pain. results from Thunder Project II. Am J Crit Care 2001; 10:238–251.
15. Puntillo, K, et al, Patients’ perceptions and responses to procedural pain. results from Thunder Project II. Am J Crit Care 2001; 10:238–251.
![]() 16. Puntillo, K, Ley, SJ. Appropriately timed analgesics control pain due to chest tube removal. Am J Crit Care. 2004; 13:292–304.
16. Puntillo, K, Ley, SJ. Appropriately timed analgesics control pain due to chest tube removal. Am J Crit Care. 2004; 13:292–304.
17. Sakopoulos, AG, et al. Efficacy of Blake drains for mediastinal and pleural drainage following cardiac operations. J Card Surg. 2005; 20(6):574–577.
18. Sullivan, B. Nursing management of patients with a chest drain. Br J Nurs. 2008; 17(6):388–393.
![]() 19. Suls, J, Wan, CK, Effects of sensory and procedural information on coping with stressful medical procedures and pain. a meta-analysis. J Consult Clin Psychol 1989; 57:372–379.
19. Suls, J, Wan, CK, Effects of sensory and procedural information on coping with stressful medical procedures and pain. a meta-analysis. J Consult Clin Psychol 1989; 57:372–379.
![]() 20. Summer, GH, Puntillo, K. Management of surgical and procedural pain in a critical care setting. Crit Care Nurs Clin North Am. 2001; 13:233–242.
20. Summer, GH, Puntillo, K. Management of surgical and procedural pain in a critical care setting. Crit Care Nurs Clin North Am. 2001; 13:233–242.
![]() 21. Younes, RN, et al. When to remove a chest tube? A randomized study with subsequent prospective consecutive validation. J Am Coll Surg. 2002; 195(5):658–662.
21. Younes, RN, et al. When to remove a chest tube? A randomized study with subsequent prospective consecutive validation. J Am Coll Surg. 2002; 195(5):658–662.