Procedure 20 Endoscopic Thoracic Diskectomy
Indications
 The indications for thoracoscopic diskectomy are similar to the indications for other procedures to treat central thoracic disk herniations.
The indications for thoracoscopic diskectomy are similar to the indications for other procedures to treat central thoracic disk herniations.
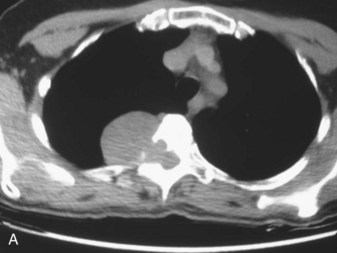
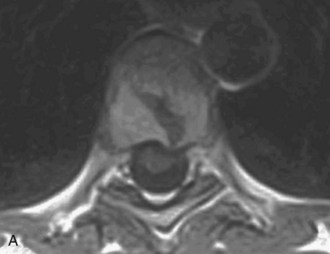
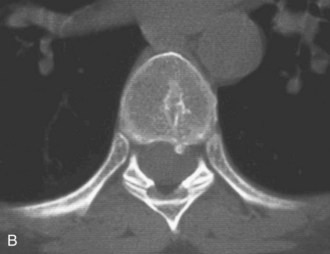
 Thoracoscopic spinal surgery may also be performed for nerve sheath tumor resection, anterior release for scoliosis, sympathectomy for hyperhidrosis, or vertebral corpectomy. Figure 20-1 shows a 55-year-old female patient with an incidental finding of a mediastinal mass on a chest radiograph. An axial computed tomography (CT) scan (see Figure 20-1, A), as well as axial (see Figure 20-1, B) and sagittal (see Figure 20-1, C) magnetic resonance imaging (MRI), showed a dumbbell-shaped tumor (peripheral nerve sheath tumor) of a nerve root with expansion of the neuroforamen. The tumor was successfully removed with simultaneous posterior and thoracoscopic excision.
Thoracoscopic spinal surgery may also be performed for nerve sheath tumor resection, anterior release for scoliosis, sympathectomy for hyperhidrosis, or vertebral corpectomy. Figure 20-1 shows a 55-year-old female patient with an incidental finding of a mediastinal mass on a chest radiograph. An axial computed tomography (CT) scan (see Figure 20-1, A), as well as axial (see Figure 20-1, B) and sagittal (see Figure 20-1, C) magnetic resonance imaging (MRI), showed a dumbbell-shaped tumor (peripheral nerve sheath tumor) of a nerve root with expansion of the neuroforamen. The tumor was successfully removed with simultaneous posterior and thoracoscopic excision.
Controversies
• The use of navigation systems has been shown to facilitate operation (Holly et al, 2001).
• Posterolateral approaches, such as a transpedicular or costotransversectomy approach, could address a ventral herniation; however, these approaches are ideal for paracentral lesions (Johnson et al, 2000).
• A multilevel procedure may be better undertaken with thoracotomy because of longer operative time with thoracoscopy.
• A preoperative angiogram has been recommended to determine location of the artery of Adamkiewicz (Di Chiro et al, 1970). However, for a thoracic diskectomy, ligation of a segmental artery is rarely necessary.
• Fusion may be necessary when excessive disk material is removed or the spine is otherwise destabilized.
Examination/Imaging
 Symptoms of a thoracic herniated disk correlate with thoracic radiculopathy, thoracic back pain, myelopathy, or vague nondermatomal leg pain (Anand and Regan, 2002).
Symptoms of a thoracic herniated disk correlate with thoracic radiculopathy, thoracic back pain, myelopathy, or vague nondermatomal leg pain (Anand and Regan, 2002).
 Selective thoracic nerve root blocks can be performed for therapeutic and diagnostic purposes, although no long-term pain relief has been shown in the literature. MRI has superior soft tissue detail and can show cord compression in multiple planes. The authors recommend obtaining an MRI of the lumbar spine with sagittal views of the thoracolumbar junction to compare with the thoracic MRI. This facilitates intraoperative localization.
Selective thoracic nerve root blocks can be performed for therapeutic and diagnostic purposes, although no long-term pain relief has been shown in the literature. MRI has superior soft tissue detail and can show cord compression in multiple planes. The authors recommend obtaining an MRI of the lumbar spine with sagittal views of the thoracolumbar junction to compare with the thoracic MRI. This facilitates intraoperative localization.
 In very challenging patients with poor anatomic localization, midthoracic lesions with little anatomic cues, or obvious vertebral body deformation, percutaneous placement of a radiopaque marker (Guglielmi detachable coil) in the pedicle adjacent to the disk in question can be performed preoperatively using CT guidance from a dorsal approach (Binning and Schmidt, 2010).
In very challenging patients with poor anatomic localization, midthoracic lesions with little anatomic cues, or obvious vertebral body deformation, percutaneous placement of a radiopaque marker (Guglielmi detachable coil) in the pedicle adjacent to the disk in question can be performed preoperatively using CT guidance from a dorsal approach (Binning and Schmidt, 2010).
 CT scans define the bony detail and a calcified disk better than MRI.
CT scans define the bony detail and a calcified disk better than MRI.
 High-quality plain radiographs of the lumbar spine and thoracic spine with overlapping views of the thoracolumbar junction are needed to confirm level. This can be important in patients with anomalous thoracic vertebrae (e.g., 13 thoracic vertebrae).
High-quality plain radiographs of the lumbar spine and thoracic spine with overlapping views of the thoracolumbar junction are needed to confirm level. This can be important in patients with anomalous thoracic vertebrae (e.g., 13 thoracic vertebrae).
Treatment Options
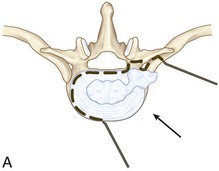
• Open thoracotomy and excision of central disk herniation through transthoracic approach (Figure 20-6, A)
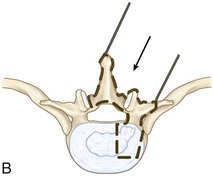
• Posterolateral approach for lateral calcified disk herniation or central soft disk herniation: transpedicular or transfacet pedicle-sparing approaches (Figure 20-6, B)
• Other methods of treatment for ventral disk herniation include lateral extracavitary and costotransversectomy approaches (Bohlman and Zdeblick, 1988) (Figure 20-6, C).
Surgical Anatomy
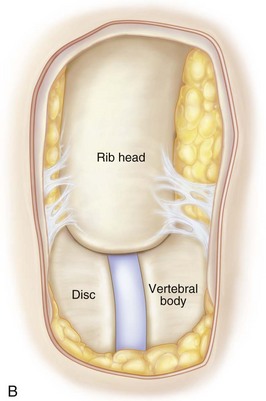
 The neurovascular bundle runs on the inferior border of the rib. The rib heads are more cephalad (i.e., closer to the disk space) in the cephalad levels. Above T10, a complete rib head resection may be needed to expose the disk space (Johnson et al, 2000; Moro et al, 2004).
The neurovascular bundle runs on the inferior border of the rib. The rib heads are more cephalad (i.e., closer to the disk space) in the cephalad levels. Above T10, a complete rib head resection may be needed to expose the disk space (Johnson et al, 2000; Moro et al, 2004).
 For a T7-8 diskectomy, the T8 rib head should be resected.
For a T7-8 diskectomy, the T8 rib head should be resected.
 The disk space is cephalad to the pedicle.
The disk space is cephalad to the pedicle.
 The artery of Adamkiewicz is usually on the left and between T9 and L3.
The artery of Adamkiewicz is usually on the left and between T9 and L3.
 Segmental vessels are located in the midportion of the vertebral body. For a diskectomy, these can be moved aside or coagulated, if necessary.
Segmental vessels are located in the midportion of the vertebral body. For a diskectomy, these can be moved aside or coagulated, if necessary.
Anatomy Pearls
• Use a bed with a break to allow lateral bending of the patient, to open the rib interspaces in small patients.
• Position the patient parallel to the room architecture.
• Check fluoroscopy before making the incision to ensure adequate imaging of appropriate level.
• Many radiologists will localize a thoracic lesion using the cervical spine and counting caudad. This can lead to wrong-level surgery, because intraoperative confirmation of the level is usually performed using the lumbar spine and thoracolumbar junction and the ribs. Therefore the authors suggest obtaining high-quality radiographs and MR images of the lumbar spine, with visualization of the thoracolumbar junction, and relating the anatomic nuances (osteophyte, disk collapse, short rib, etc.) to the thoracic imaging.
• Prepare the ipsilateral iliac crest, in case a fusion procedure is necessary.
• Ensure that the table can easily tilt anteriorly, to aid in lung retraction.
• The Trendelenburg position can facilitate hemostasis.
• Poor positioning of monitors can hinder vision and flow of the operation.
• If there is a history of previous thoracic surgery, strongly consider entering the chest from the contralateral side to avoid adhesions and scar tissue.
• Vacuum sand bag, intraoperative monitoring wires, and bed attachments in line with the fluoroscope may hinder high-quality intraoperative images.
Positioning
 Give prophylactic antibiotics for gram-positive organism coverage.
Give prophylactic antibiotics for gram-positive organism coverage.
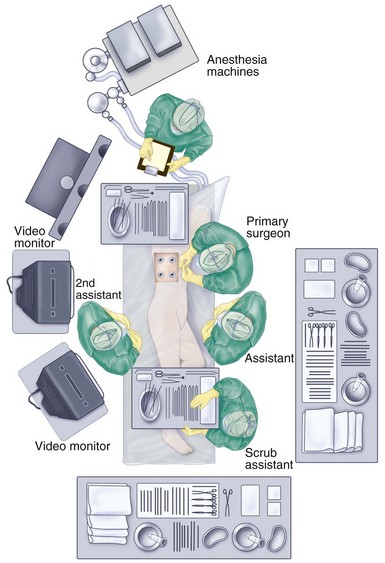
 The proper surgical team, anesthesiologist, and monitoring setup are crucial.
The proper surgical team, anesthesiologist, and monitoring setup are crucial.
 Apply antithromboembolic stockings and sequential pneumatic compression.
Apply antithromboembolic stockings and sequential pneumatic compression.
 A double-lumen endotracheal tube is placed for single-lung ventilation.
A double-lumen endotracheal tube is placed for single-lung ventilation.
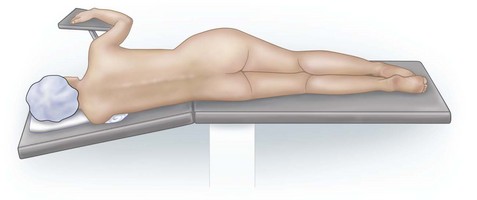
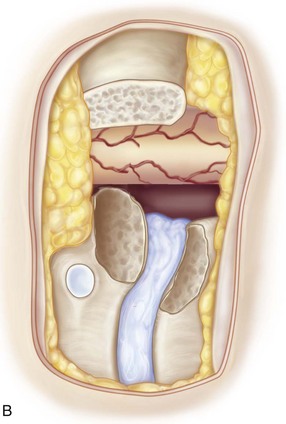
 The patient is placed in the lateral decubitus position, with the ventilated lung down (Figure 20-7). The arm is held in an “airplane”-type holder to expose the chest wall.
The patient is placed in the lateral decubitus position, with the ventilated lung down (Figure 20-7). The arm is held in an “airplane”-type holder to expose the chest wall.
 Pad all bony prominences and superficial nerves (e.g., peroneal and ulnar nerves).
Pad all bony prominences and superficial nerves (e.g., peroneal and ulnar nerves).
 Prepare the patient for possible thoracotomy. Also, prepare the patient’s back for a possible simultaneous posterior approach.
Prepare the patient for possible thoracotomy. Also, prepare the patient’s back for a possible simultaneous posterior approach.
 The surgeon and assistant should stand on the abdominal side of the patient. A second assistant can stand on the back side of the patient, in case extra instruments are necessary (Figure 20-8).
The surgeon and assistant should stand on the abdominal side of the patient. A second assistant can stand on the back side of the patient, in case extra instruments are necessary (Figure 20-8).
 The monitors should be on both sides of the patient, directly facing the surgeon, assistants, and operating room technician.
The monitors should be on both sides of the patient, directly facing the surgeon, assistants, and operating room technician.
Endoscopic Equipment
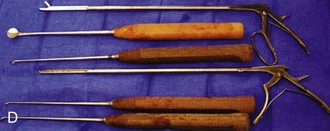
• Endoscope with conventional 5- or 10-mm lenses with 0-, 30-, or 45-degree angles (Figure 20-9, A); angled scopes prevent “fencing” within the chest (30 degree angled scope is ideal)
• Standard illumination source, camera attachment, and video monitor
• Pneumatic drill with a long shaft (25 cm) and pistol grip for rotational control (Figure 20-9, B)
• Coarse diamond burr or large round burr (5 mm) (Figure 20-9, C)
• Long-shaft Kerrison rongeurs, Cobb elevators, pituitaries, and curettes (Figure 20-9, D)
• Endoscopic cotton-tipped applicators
Portals/Exposures
 Three to four portals are usually sufficient to insert the endoscope, retractor, and suction-irrigation instrument and to perform the diskectomy.
Three to four portals are usually sufficient to insert the endoscope, retractor, and suction-irrigation instrument and to perform the diskectomy.
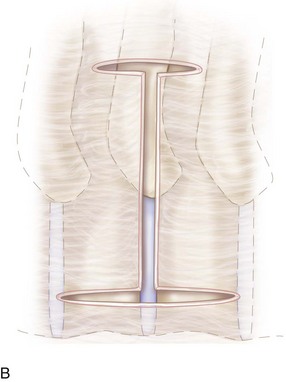
 Portal placement should proceed with an incision centered on the rib and blunt dissection over the superior border (Figure 20-10).
Portal placement should proceed with an incision centered on the rib and blunt dissection over the superior border (Figure 20-10).
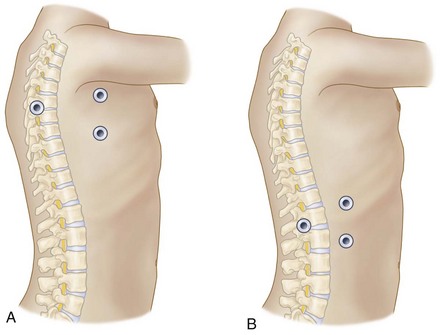
 The main working portal should be placed in the posterior axillary line, perpendicular to the pathologic location (Figure 20-11, A and B). However, the first portal should be above the sixth or seventh rib to avoid the diaphragm. Insert the other portals under direct visualization.
The main working portal should be placed in the posterior axillary line, perpendicular to the pathologic location (Figure 20-11, A and B). However, the first portal should be above the sixth or seventh rib to avoid the diaphragm. Insert the other portals under direct visualization.
 Two to three other accessory portals can be placed in the anterior axillary line, cephalad and caudad to the main working portal, to triangulate within the chest (see Figure 20-11).
Two to three other accessory portals can be placed in the anterior axillary line, cephalad and caudad to the main working portal, to triangulate within the chest (see Figure 20-11).
 The perpendicular portal is usually where the drill and rongeurs are inserted, but all the portals can be used for passing various instruments to proceed with the diskectomy safely.
The perpendicular portal is usually where the drill and rongeurs are inserted, but all the portals can be used for passing various instruments to proceed with the diskectomy safely.
Portals/Exposures Pearls
• The disk space and proximal rib head are colinear and can keep the surgeon oriented.
• The neural foramen contains epidural fat that can be used to indicate proximity of the nerve root.
• To ensure the appropriate operative level, intraoperative fluoroscopy or radiograph of a metallic instrument overlying the disk space should be compared with preoperative radiographs and MRI scans.
Procedure
Step 1
 Once portals are made and the lung retracted anteriorly with a fan retractor, the disk space is located by tracing the rib to the spine.
Once portals are made and the lung retracted anteriorly with a fan retractor, the disk space is located by tracing the rib to the spine.
 Fluoroscopy or an anteroposterior thoracic spine radiograph can be taken with a metallic instrument on the disk space to confirm the appropriate level (Figure 20-12, A and B).
Fluoroscopy or an anteroposterior thoracic spine radiograph can be taken with a metallic instrument on the disk space to confirm the appropriate level (Figure 20-12, A and B).
 Adjacent segmental vessels can be retracted or cauterized, depending on the extent of bony decompression.
Adjacent segmental vessels can be retracted or cauterized, depending on the extent of bony decompression.
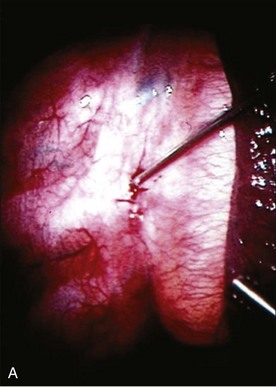
 The parietal pleura is widely dissected off the rib head and disk space using a Harmonic scalpel (Ethicon Endo-Surgery) (Figure 20-13, A and B).
The parietal pleura is widely dissected off the rib head and disk space using a Harmonic scalpel (Ethicon Endo-Surgery) (Figure 20-13, A and B).
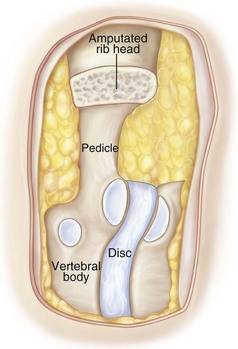
 The proximal 2 cm of the rib are removed with a pneumatic drill to expose the lateral wall of the pedicle and neural foramen (Figure 20-14).
The proximal 2 cm of the rib are removed with a pneumatic drill to expose the lateral wall of the pedicle and neural foramen (Figure 20-14).
 The pedicle is then drilled away to expose the dura of the spinal cord.
The pedicle is then drilled away to expose the dura of the spinal cord.
Step 2
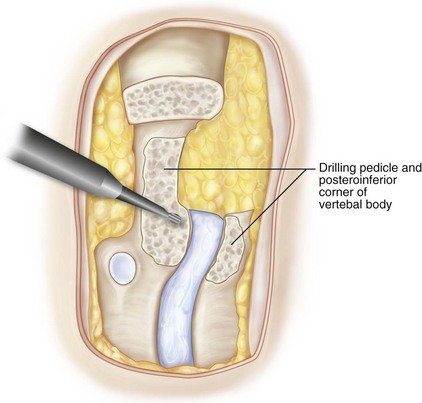
 Subsequent to removal of the pedicle and exposure of the neural foramen and epidural fat, the posterior margin of the vertebral body is palpated, and the superior and inferior end plates are drilled away (Figure 20-15).
Subsequent to removal of the pedicle and exposure of the neural foramen and epidural fat, the posterior margin of the vertebral body is palpated, and the superior and inferior end plates are drilled away (Figure 20-15).
 Begin drilling from the posterior margin of the vertebral body to approximately one third of the sagittal distance, leaving a cortical shell posteriorly to protect the ventral aspect of the spinal cord.
Begin drilling from the posterior margin of the vertebral body to approximately one third of the sagittal distance, leaving a cortical shell posteriorly to protect the ventral aspect of the spinal cord.
 The anterior two thirds of the vertebral body should be left intact.
The anterior two thirds of the vertebral body should be left intact.
 The cephalad and caudad extension of the vertebral body decompression depends on the size and migration of the herniated disk fragment.
The cephalad and caudad extension of the vertebral body decompression depends on the size and migration of the herniated disk fragment.
Step 3
 Burr the tunnel to the opposite pedicle depending on the size of the disk herniation.
Burr the tunnel to the opposite pedicle depending on the size of the disk herniation.
 Confirm the location of the burr with anteroposterior fluoroscopy.
Confirm the location of the burr with anteroposterior fluoroscopy.
 Once burring is completed, the floor of the canal that is left as a cortical shell can be removed with fine curettes or Kerrison rongeurs.
Once burring is completed, the floor of the canal that is left as a cortical shell can be removed with fine curettes or Kerrison rongeurs.
 The portion of the disk that is not herniated and is between the vertebral bodies is removed.
The portion of the disk that is not herniated and is between the vertebral bodies is removed.
 A rent is made in the posterior longitudinal ligament with a blunt probe or nerve hook, and the ligament is subsequently resected with Kerrison rongeurs.
A rent is made in the posterior longitudinal ligament with a blunt probe or nerve hook, and the ligament is subsequently resected with Kerrison rongeurs.
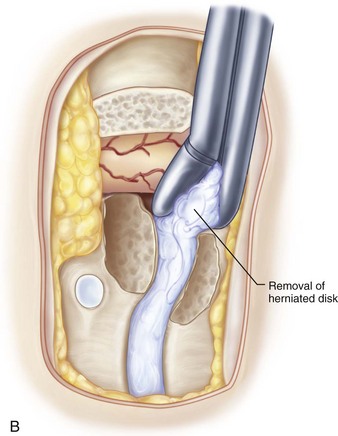
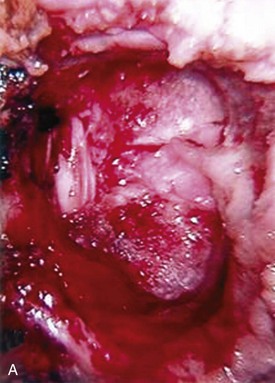
 The remaining herniated portion of the disk is subsequently pulled into the defect created by the bony decompression (Figure 20-16, A and B).
The remaining herniated portion of the disk is subsequently pulled into the defect created by the bony decompression (Figure 20-16, A and B).
 A calcified disk can be thinned with a burr to form a thin shell, which can be cracked and pulled into the decompressed space. This allows complete decompression of the spinal cord without any manipulation (Figure 20-17, A and B).
A calcified disk can be thinned with a burr to form a thin shell, which can be cracked and pulled into the decompressed space. This allows complete decompression of the spinal cord without any manipulation (Figure 20-17, A and B).
Step 4
 A chest tube is placed through one of the portals or through a separate incision, tunneled through the subcutaneous tissue, and guided endoscopically to the apex of the chest cavity.
A chest tube is placed through one of the portals or through a separate incision, tunneled through the subcutaneous tissue, and guided endoscopically to the apex of the chest cavity.
 Suction is applied at 20 cm H2O, and the lung is reinflated.
Suction is applied at 20 cm H2O, and the lung is reinflated.
 A chest radiograph is obtained after extubation to ensure that the lung is inflated.
A chest radiograph is obtained after extubation to ensure that the lung is inflated.
 The fascia is sutured with 2-0 Vicryl and the skin with 3-0 Vicryl subcuticular interrupted sutures, followed by Steri-Strips over the incision.
The fascia is sutured with 2-0 Vicryl and the skin with 3-0 Vicryl subcuticular interrupted sutures, followed by Steri-Strips over the incision.
Step 4 Controversies
• Extensive decompression could lead to increased mobility of the spinal segment. Potentially, this could lead to increased axial back pain and disability. Certain patients could benefit from a fusion after decompression (Anand and Regan, 2002). According to Broc and associates (1997), a cadaveric study showed slightly increased instability after endoscopic thoracic diskectomy without gross instability.
Postoperative Care and Expected Outcomes
 The chest tube is removed when drainage is less than 100 mL/day; usually by postoperative day 2.
The chest tube is removed when drainage is less than 100 mL/day; usually by postoperative day 2.
 The patient is ambulated on postoperative day 1.
The patient is ambulated on postoperative day 1.
 Oral analgesic medications are usually sufficient for adequate pain control.
Oral analgesic medications are usually sufficient for adequate pain control.
Surgical Outcomes
 Patients with severe myelopathy or dense neurologic loss usually stabilize or slightly improve (Anand and Regan, 2002; Johnson et al, 2000; Oskouian and Johnson, 2005).
Patients with severe myelopathy or dense neurologic loss usually stabilize or slightly improve (Anand and Regan, 2002; Johnson et al, 2000; Oskouian and Johnson, 2005).
 Patients with milder forms of myelopathy generally have significant improvement (Johnson et al, 2000; Oskouian and Johnson, 2005). Figure 20-18, A shows a preoperative T2-weighted MRI in a patient with acute ventral herniated nucleus pulposus causing myelopathy. The T1-weighted MRI in Figure 20-18, B was taken after thoracoscopic decompression with complete resolution of symptoms. Note that the extent of the bony decompression should be large enough to reduce the herniated disk without manipulation of the spinal cord.
Patients with milder forms of myelopathy generally have significant improvement (Johnson et al, 2000; Oskouian and Johnson, 2005). Figure 20-18, A shows a preoperative T2-weighted MRI in a patient with acute ventral herniated nucleus pulposus causing myelopathy. The T1-weighted MRI in Figure 20-18, B was taken after thoracoscopic decompression with complete resolution of symptoms. Note that the extent of the bony decompression should be large enough to reduce the herniated disk without manipulation of the spinal cord.
 Axial back pain or thoracic radiculopathy also improves after thoracoscopic diskectomy, albeit the results are more modest, paralleling treatment for mechanical lumbar back pain (Anand and Regan, 2002; Rosenthal and Dickman, 1998).
Axial back pain or thoracic radiculopathy also improves after thoracoscopic diskectomy, albeit the results are more modest, paralleling treatment for mechanical lumbar back pain (Anand and Regan, 2002; Rosenthal and Dickman, 1998).
Complications and Avoidance
 Pneumonia: generally not as common in endoscopic cases compared with thoracotomy (Rosenthal and Dickman, 1998)
Pneumonia: generally not as common in endoscopic cases compared with thoracotomy (Rosenthal and Dickman, 1998)
 Persistent chest tube drainage: can be avoided with meticulous hemostasis during decompression with application of bone wax to bleeding surface of bone.
Persistent chest tube drainage: can be avoided with meticulous hemostasis during decompression with application of bone wax to bleeding surface of bone.
Anand N, Regan JJ. Video-assisted thoracoscopic surgery for thoracic disc disease: classification and outcome study of 100 consecutive cases with a 2-year minimum follow-up. Spine. 2002;27:871-879.
Binning MJ, Schmidt MH. Percutaneous placement of radiopaque markers at the pedicle of interest for preoperative localization of thoracic spine level. Spine. 2010;35:1821-1825.
Bohlman HH, Zdeblick TA. Anterior excision of herniated thoracic discs. J Bone Joint Surg Am. 1988;70:1038-1047.
Broc GG, Crawford NR, Sonntag VKH, Dickman CA. Biomechanical effects of transthoracic microdiscectomy. Spine. 1997;22:605-612.
Di Chiro G, Fried LC, Doppman JL. Experimental spinal cord angiography. Br J Radiol. 1970;43:19-30.
Holly LT, Bloch O, Obasi C, Johnson JP. Frameless stereotaxy for anterior spinal procedures. J Neurosurg Spine. 2001;95:196-201.
Johnson JP, Filler AG, McBride DQ. Endoscopic thoracic discectomy. Neurosurg Focus. 2000;9:e11.
Le Huec JC, Lesprite E, Touagliaro F, et al. Complications of thoracoscopic spinal surgery: analysis of a series of patients. J Bone Joint Surg Br. 2002;84:44.
Moro T, Kikuchi S, Konno S. Necessity of rib head resection for anterior discectomy in the thoracic spine. Spine. 2004;29:1703-1705.
This study involves a Grade B recommendation for complete rib head removal above T9 (cadaver study).
Oskouian RJ, Johnson JP. Endoscopic thoracic microdiscectomy. J Neurosurg Spine. 2005;99:459-464.
Rosenthal D, Dickman CA. Thoracoscopic microsurgical excision of herniated thoracic discs. J Neurosurg. 1998;89:224-235.