Procedure 2 Halo Placement in the Pediatric and Adult Patient
Indications
 Odontoid fracture: type III or specific type II
Odontoid fracture: type III or specific type II
 One-column bony cervical spine fracture
One-column bony cervical spine fracture
 Fracture in ankylosing spondylitis
Fracture in ankylosing spondylitis
 Preoperative traction or stabilization
Preoperative traction or stabilization
 Postoperative stabilization of arthrodesis, infection, tumor resection
Postoperative stabilization of arthrodesis, infection, tumor resection
Treatment Options
• Consider rigid collar immobilization in a compliant, young, healthy patient with a minimally displaced, stable fracture.
• Consider surgical intervention in an elderly or noncompliant patient with an unstable or displaced fracture, a fracture of high nonunion potential, ligamentous injury, or associated injury.
• Move to surgical intervention for failure of halo fixation: loss of fracture alignment, symptomatic nonunion, neurologic deterioration.
Examination/Imaging
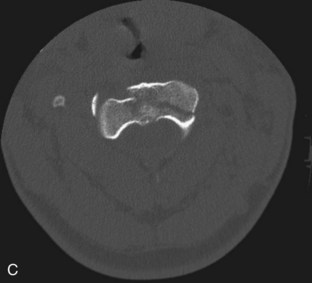
 Computed tomography (CT) is required to define fracture morphology and stability and rule out adjacent or noncontiguous injuries (Como et al, 2009) (Figure 2-1, A–C).
Computed tomography (CT) is required to define fracture morphology and stability and rule out adjacent or noncontiguous injuries (Como et al, 2009) (Figure 2-1, A–C).
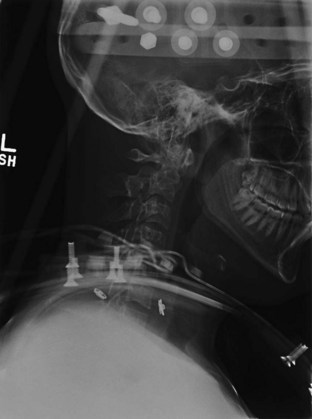
 Radiographs confirm fracture reduction and cervical alignment following halo application, and maintenance of these parameters during treatment (Figure 2-2).
Radiographs confirm fracture reduction and cervical alignment following halo application, and maintenance of these parameters during treatment (Figure 2-2).
Surgical Anatomy
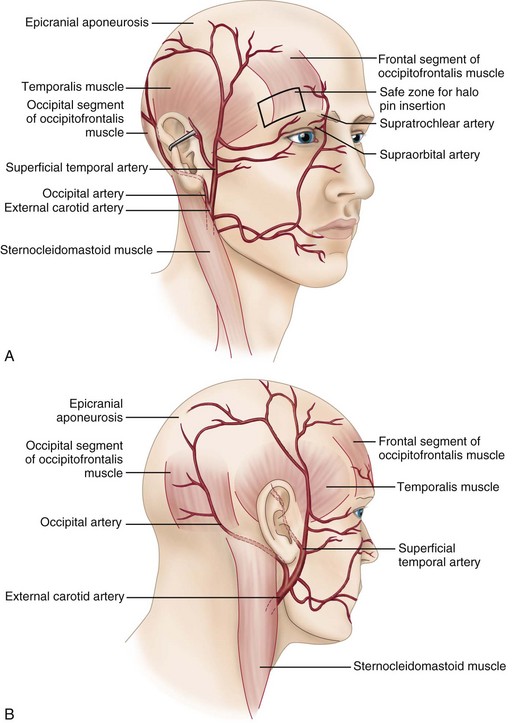
 Relevant anatomy pertains to pin placement. Correct placement prevents direct neural or vascular injury, inner calvarial plate penetration, and pin migration, while providing adequate strength of fixation.
Relevant anatomy pertains to pin placement. Correct placement prevents direct neural or vascular injury, inner calvarial plate penetration, and pin migration, while providing adequate strength of fixation.
Positioning
 Typical halo application is performed in the supine position utilizing in-line cervical stabilization by a knowledgeable care provider while two providers apply the apparatus.
Typical halo application is performed in the supine position utilizing in-line cervical stabilization by a knowledgeable care provider while two providers apply the apparatus.
 For stable fractures or nonfracture treatment, halo application in the upright position is preferred to optimize cranial-cervical-thoracic alignment and patient comfort.
For stable fractures or nonfracture treatment, halo application in the upright position is preferred to optimize cranial-cervical-thoracic alignment and patient comfort.
 A cervical collar can provide additional stability until the halo construct is completed.
A cervical collar can provide additional stability until the halo construct is completed.
Procedure: Halo Application
Step 1: Crown and Pin Placement
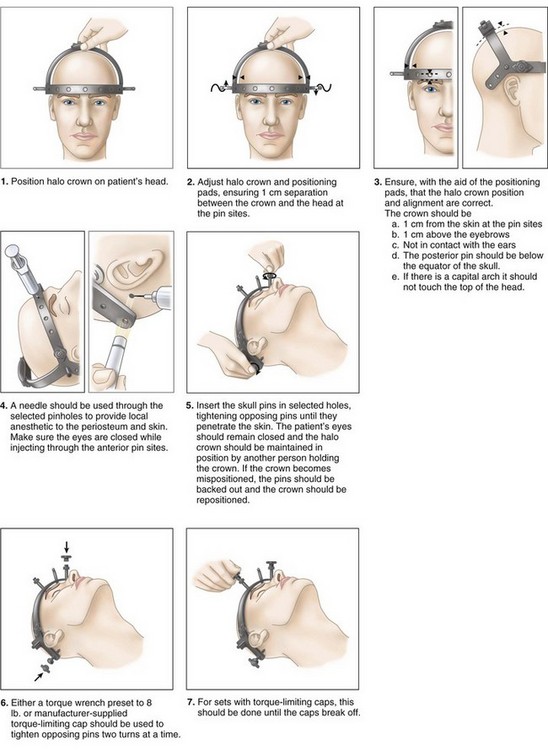
 Identify proper crown size: small for 48- to 58-cm head circumference, large for 58- to 66-cm head circumference. Choose the smallest crown size that allows at least 1 cm of space between head and crown.
Identify proper crown size: small for 48- to 58-cm head circumference, large for 58- to 66-cm head circumference. Choose the smallest crown size that allows at least 1 cm of space between head and crown.
 Identify proper pin sites as previously described in the “Surgical Anatomy” section of this chapter.
Identify proper pin sites as previously described in the “Surgical Anatomy” section of this chapter.
 Shave hair at posterior sites and cleanse skin at all sites with Betadine or alcohol preparation.
Shave hair at posterior sites and cleanse skin at all sites with Betadine or alcohol preparation.
 Instruct patient to keep eyes closed and face musculature relaxed.
Instruct patient to keep eyes closed and face musculature relaxed.
 Utilize positioning pins to align and maintain halo position: 1 cm above eyebrow and top of ear and below largest circumference of the head.
Utilize positioning pins to align and maintain halo position: 1 cm above eyebrow and top of ear and below largest circumference of the head.
 Inject 1% lidocaine with epinephrine at the intended pin sites. Pass the needle through the pin holes of the halo ring to optimize anesthetic positioning. Inject from skin though to periosteum for patient comfort during pin placement.
Inject 1% lidocaine with epinephrine at the intended pin sites. Pass the needle through the pin holes of the halo ring to optimize anesthetic positioning. Inject from skin though to periosteum for patient comfort during pin placement.
 Traditionally, four pins provide halo fixation.
Traditionally, four pins provide halo fixation.
 Initial skin incision at the pin sites is not necessary and does not influence scar formation.
Initial skin incision at the pin sites is not necessary and does not influence scar formation.
 Placement of all pins should occur simultaneously to maintain halo position and balance pin forces. Simultaneous advancement to the skin, through the soft tissue, and to the skull should occur, with final security achieved with release of the breakaway torque-limiting caps (Figure 2-4) (Depuy Spine Bremer Halo Systems technical monograph).
Placement of all pins should occur simultaneously to maintain halo position and balance pin forces. Simultaneous advancement to the skin, through the soft tissue, and to the skull should occur, with final security achieved with release of the breakaway torque-limiting caps (Figure 2-4) (Depuy Spine Bremer Halo Systems technical monograph).
 Confirm torque to 8 inch-pounds utilizing a torque wrench.
Confirm torque to 8 inch-pounds utilizing a torque wrench.
 With pins secure to the skull, tighten the locking nuts to secure the pins to the halo ring.
With pins secure to the skull, tighten the locking nuts to secure the pins to the halo ring.
 Areas of tethered or tented skin surrounding the pins can be released using a scalpel as needed.
Areas of tethered or tented skin surrounding the pins can be released using a scalpel as needed.
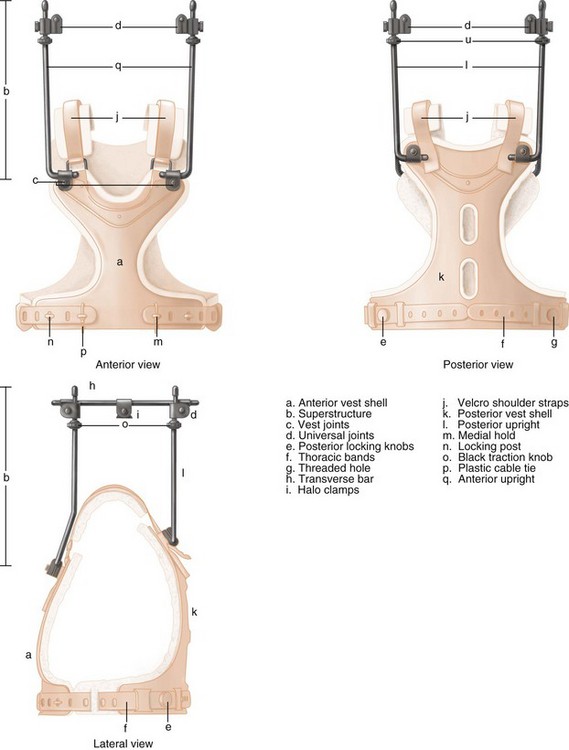
Step 2: Vest Application
 Identify proper vest size based on chest circumference 5 cm below the xiphoid process and patient height: short vest for circumference of 70 to 97 cm and height less than 170 cm, large vest for circumference up to 112 cm and height greater than 170 cm.
Identify proper vest size based on chest circumference 5 cm below the xiphoid process and patient height: short vest for circumference of 70 to 97 cm and height less than 170 cm, large vest for circumference up to 112 cm and height greater than 170 cm.
 In-line cervical stabilization is maintained as required.
In-line cervical stabilization is maintained as required.
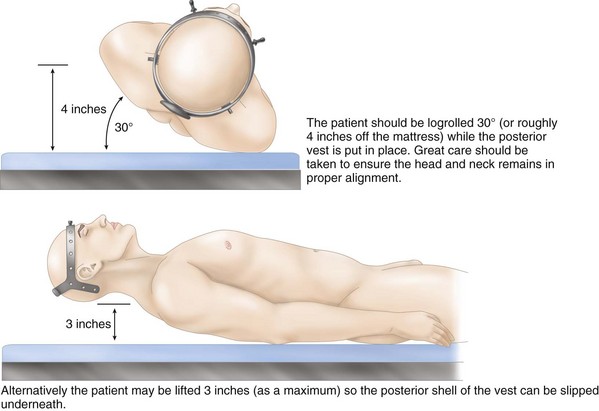
 Logrolling or trunk elevation allows placement of the posterior shell of the vest (Magnum and Sunderland, 1993) (Figure 2-5).
Logrolling or trunk elevation allows placement of the posterior shell of the vest (Magnum and Sunderland, 1993) (Figure 2-5).
 The anterior shell is positioned and secured to the posterior shell.
The anterior shell is positioned and secured to the posterior shell.
 The vertical bars are secured on the vest and positioned for fixation to the crown.
The vertical bars are secured on the vest and positioned for fixation to the crown.
Step 3: Construct Alignment
 Each posterior vertical bar is attached to its ipsilateral anterior bar by the horizontal crown connector. Loosen all joints within the construct to allow appropriate alignment of the bars relative to the crown.
Each posterior vertical bar is attached to its ipsilateral anterior bar by the horizontal crown connector. Loosen all joints within the construct to allow appropriate alignment of the bars relative to the crown.
 Time spent in optimizing bar position before attachment to the crown will minimize patient discomfort and risk of loss of cervical alignment, which can occur when adjustments are made with the construct secured to the crown (Magnum and Sunderland, 1993) (Figure 2-6).
Time spent in optimizing bar position before attachment to the crown will minimize patient discomfort and risk of loss of cervical alignment, which can occur when adjustments are made with the construct secured to the crown (Magnum and Sunderland, 1993) (Figure 2-6).
 Ensure symmetry between left and right bar constructs.
Ensure symmetry between left and right bar constructs.
 Final tightening of all joints of the crown and vest construct should provide security with no concern for loosening.
Final tightening of all joints of the crown and vest construct should provide security with no concern for loosening.
 Only when final stability is obtained may the rigid collar be removed and in-line stabilization released.
Only when final stability is obtained may the rigid collar be removed and in-line stabilization released.
 Final cranial-cervical-thoracic alignment is crucial to: (1) maintain fracture alignment, (2) provide patient comfort, and (3) optimize patient function, specifically concerning normal vision and swallowing ability.
Final cranial-cervical-thoracic alignment is crucial to: (1) maintain fracture alignment, (2) provide patient comfort, and (3) optimize patient function, specifically concerning normal vision and swallowing ability.
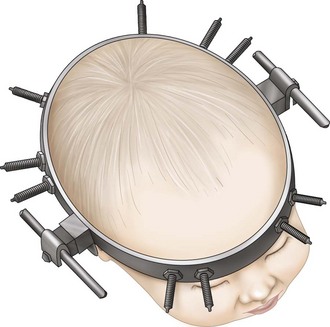
Procedure: Halo Application in the Child or Infant
 Relevant differences in halo application in the pediatric population pertain to skull thickness, skull hardness, and the presence of open cranial sutures. Cranial penetration must be avoided.
Relevant differences in halo application in the pediatric population pertain to skull thickness, skull hardness, and the presence of open cranial sutures. Cranial penetration must be avoided.
 Consider general anesthesia depending on age and diagnosis. Although an anesthetized patient cannot provide feedback regarding neurologic status, this may be irrelevant in the very young child or infant.
Consider general anesthesia depending on age and diagnosis. Although an anesthetized patient cannot provide feedback regarding neurologic status, this may be irrelevant in the very young child or infant.
 A custom crown and vest may be necessary, although pediatric sizes are available.
A custom crown and vest may be necessary, although pediatric sizes are available.
 Consider preapplication computed tomography to identify cranial sutures and plan pin placement (Mubarak et al, 1989) (Figure 2-7).
Consider preapplication computed tomography to identify cranial sutures and plan pin placement (Mubarak et al, 1989) (Figure 2-7).
 Eight to 10 pins are utilized to provide stable fixation at lower torque forces.
Eight to 10 pins are utilized to provide stable fixation at lower torque forces.
 Torque to 2 inch-pounds utilizing a torque wrench. Consider torquing to finger tightness only in the very young child or infant.
Torque to 2 inch-pounds utilizing a torque wrench. Consider torquing to finger tightness only in the very young child or infant.
Pitfalls
• Beware of halo use in the extremes of ages. In the very young, skull thickness and frequent falls during typical pediatric ambulation increase complications. In the elderly, cardiopulmonary dysfunction leads to significantly increased morbidity and mortality. Some clinicians question the safety of this tool in the elderly (Majercik et al, 2005).
Postoperative Care and Expected Outcomes
Botte MJ, Byrne TP, Abrams RA, Garfin SR. The halo skeletal fixator: current concepts of application and maintenance. Orthopedics. 1995;18:463-471.
Como JJ, Diaz JJ, Dunham CM, et al. Practice management guidelines for identification of cervical spine injuries following trauma: update from the eastern association for the surgery of trauma practice management guidelines committee. J Trauma. 2009;67:651-659.
Kang M, Vives MJ, Vaccaro AR. The halo vest: principles of application and management of complications. J Spinal Cord Med. 2003;26:186-192.
Letts M, Girouard L, Yeadon A. Mechanical evaluation of four versus eight-pin halo fixation. J Pediatr Orthop. 1997;17:121-124.
Magnum S, Sunderland PM. A comprehensive guide to the halo brace. AORN J. 1993;58:534-546.
Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Coiffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59:350-357.
Manthey DE. Halo traction device. Emerg Med Clin North Am. 1994;12:771-778.
Morishima N, Ohota K, Miura Y. The influence of halo-vest fixation and cervical hyperextension on swallowing in healthy volunteers. Spine. 2005;30:e179-e182.
Mubarak SJ, Camp JF, Vuletich W, Wenger DR, Garfin SR. Halo application in the infant. J Pediatr Orthop. 1989;9:612-614.
Nemeth JA, Mattingly LG. Six-pin halo fixation and the resulting prevalence of pin-site complications. J Bone Joint Surg Am. 2001;83:377-382.
Polin RS, Szabo T, Bogaev CA, Replogle RE, Jane JA. Nonoperative management of types II and III odontoid fractures: the Philadelphia collar versus the halo vest. Neurosurgery. 1996;38:450-457.
Product monograph. Bremer Halo Crown Traction Set. Bremer Halo Systems, Raynham, Mass., 2003.