Procedure 19 Resection of Intradural Intramedullary or Extramedullary Spinal Tumors
Indications
Examination/Imaging
 Plain films/computed tomography (CT) scan
Plain films/computed tomography (CT) scan
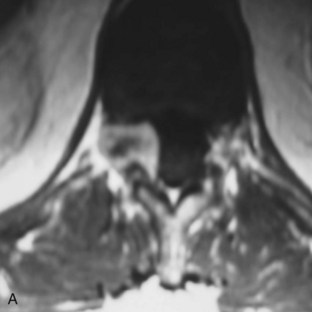
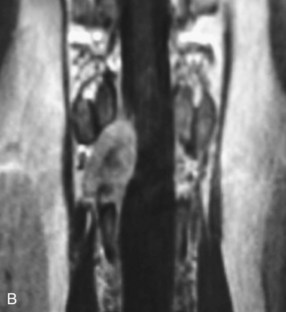
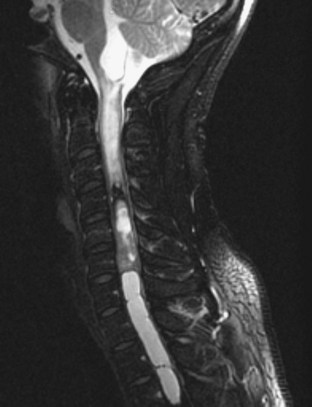
 Magnetic resonance imaging (MRI) with gadolinium
Magnetic resonance imaging (MRI) with gadolinium
Treatment Options
• Maximal tumor resection: Favorable outcomes postoperatively on intramedullary tumors are based on the histopathology of the tumor, total resection, and neurologic status preoperatively. In extramedullary tumors, postoperative neurologic recovery is very favorable in the vast majority of cases.
• Serial observation with imaging and clinical assessment is an option for intradural spinal cord tumor management in neurologically intact patients.
• Radiation therapy is a secondary treatment option or an adjuvant therapy in malignant or rapidly recurrent intramedullary spinal tumors (although optimum management in such cases remains controversial).
Surgical Anatomy
 Spinal column defines boundaries of the spinal canal. These boundaries are
Spinal column defines boundaries of the spinal canal. These boundaries are
 Levels of the spinal column are
Levels of the spinal column are
 Spinal meninges or coverings of the spinal cord
Spinal meninges or coverings of the spinal cord
Positioning
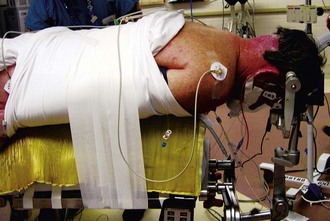
 General anesthesia with neurophysiologic monitoring
General anesthesia with neurophysiologic monitoring
 Prone position with spinal axis in the midline
Prone position with spinal axis in the midline
Positioning Pearls
• With surgical positioning, minimizing compression upon the abdomen reduces intraabdominal pressure and thus epidural venous pressure. This reduces intraoperative blood loss.
• Localization of thoracic lesions may be difficult. Either preoperative localizer or entire spine radiograph may aid in localizing incision and tumor.
Portals/Exposures
 Localize midline region and plan extent of laminectomy or bony removal.
Localize midline region and plan extent of laminectomy or bony removal.
 Make a midline incision down to the paraspinal fascia.
Make a midline incision down to the paraspinal fascia.
 Avascular subperiosteal dissection is continued bilaterally, centered over spinous process and laminae.
Avascular subperiosteal dissection is continued bilaterally, centered over spinous process and laminae.
 The retractor system should be low profile and away from the surgical site.
The retractor system should be low profile and away from the surgical site.
 Use a high-speed drill to resect posterior elements.
Use a high-speed drill to resect posterior elements.
 Drill through the laminae bilaterally at the facet–laminae junction.
Drill through the laminae bilaterally at the facet–laminae junction.
 Resect the rostral and caudal interspinous ligaments.
Resect the rostral and caudal interspinous ligaments.
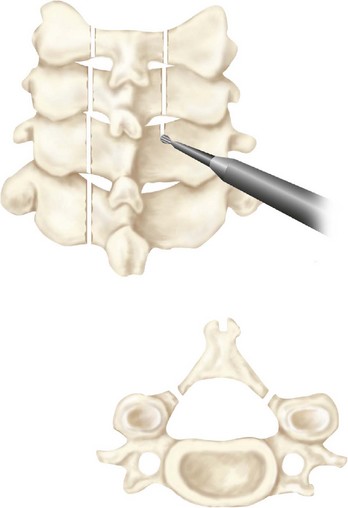
 Resect the laminae en bloc and carefully dissect free all dural adhesions (Figure 19-5).
Resect the laminae en bloc and carefully dissect free all dural adhesions (Figure 19-5).
 Confirm that the extent of dural exposure is adequate through
Confirm that the extent of dural exposure is adequate through
 Confirm that hemostasis is excellent, particularly at dural margins.
Confirm that hemostasis is excellent, particularly at dural margins.
Portals/Exposures Pearls
• A short-acting muscle relaxant will provide easier dissection but also enable the use of neurophysiologic monitoring.
• An intraoperative localizing radiograph aids in minimizing osseous removal.
• Laminectomy should provide exposure of dural region necessary to define neoplasm margins, and a slightly greater incision provides for manipulation of the lesion.
• A hemostatic agent applied along the epidural and bony edges will be useful to tamponade any venous bleeding.
Portals/Exposures Pitfalls
• Do not expose facet joints, because this may lead to delayed instability.
• With inadequate hemostasis, particularly for epidural bleeding, bleeding will become excessive once the dura is opened.
• Inadequate exposure may create the need for further bony resection when the dura is opened and will allow unnecessary entry of blood and osseous shavings into the dural sac.
Procedure
Step 1
 Hemostasis is meticulously maintained, particularly in the epidural region, before opening the dura.
Hemostasis is meticulously maintained, particularly in the epidural region, before opening the dura.
 The rostral and caudal extent of the spinal lesion are defined and assured to be within the bony opening.
The rostral and caudal extent of the spinal lesion are defined and assured to be within the bony opening.
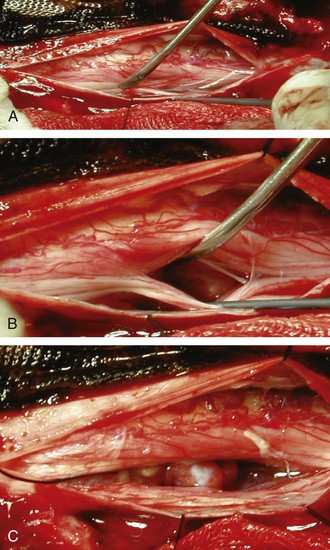
 Based on preoperative images, a single dural suture is placed, through which traction is applied to draw the dura away from the spinal cord.
Based on preoperative images, a single dural suture is placed, through which traction is applied to draw the dura away from the spinal cord.
 A midline or lateral dural incision is made with a sharp instrument.
A midline or lateral dural incision is made with a sharp instrument.
 Dural tack-up sutures bilaterally maintain the exposure of the spinal lesion and prevent blood products from entering the cerebrospinal fluid (Figure 19-6). In addition, the epidural space can be visualized with the use of hemostatic material (Surgicel; Ethicon, Somerville, N.J.).
Dural tack-up sutures bilaterally maintain the exposure of the spinal lesion and prevent blood products from entering the cerebrospinal fluid (Figure 19-6). In addition, the epidural space can be visualized with the use of hemostatic material (Surgicel; Ethicon, Somerville, N.J.).
Step 3
Step 4
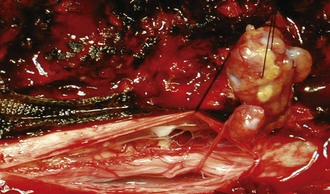
 After resection of the lesion, the wound is confirmed to have no active bleeding.
After resection of the lesion, the wound is confirmed to have no active bleeding.
 Exploration of the surgical bed for residual neoplasm is necessary to confirm gross total resection.
Exploration of the surgical bed for residual neoplasm is necessary to confirm gross total resection.
 Dura is closed with nonabsorbable suture.
Dura is closed with nonabsorbable suture.
 Before completion of the dural closure, saline is injected into the subarachnoid space to confirm a watertight closure.
Before completion of the dural closure, saline is injected into the subarachnoid space to confirm a watertight closure.
Berhouma M, Bahri K, Houissa S, et al. Management of intramedullary spinal cord tumors: surgical considerations and results in 45 cases. Neurochirurgie. 2009;55:293-302.
Biswas A, Puri T, Goyal S, et al. Spinal intradural primary germ cell tumour—review of literature and case report. Acta Neurochir. 2009;151:277-284.
Brotchi J. Intrinsic spinal cord tumor resection. Neurosurgery. 2002;50:1059-1066.
Burger PC, Scheithauer BW. Tumors of the central nervous system. In: Rosai J, Sobin LH, editors. Atlas of Tumor Pathology, series 3, facs 10. Washington, DC: Armed Forces Institute of Pathology; 1994.
Cavalcanti DD, Martirosyan NL, Verma K, et al. Surgical management and outcome of schwannomas in the craniocervical region. J Neurosurg. 2010;114:1257-1267.
Constantini S, Miller DC, Allen JC, et al. Radical excision of intramedullary spinal cord tumors: surgical morbidity and long-term follow-up evaluation in 164 children and young adults. J Neurosurg Spine. 2000;93:183-193.
Dong-Ki Ahn, Hoon-Seok Park, Daw-Jung Choi, et al. The surgical treatment for spinal intradural extramedullary tumors. Clin Orthop Surg. 2009;1:165-172.
Epstein FJ, Farmer JP, Freed D. Adult intramedullary astrocytomas of the spinal cord. J Neurosurg. 1992;77:355-359.
Mechtler L, Cohen ME. Clinical presentation and therapy of spinal tumors. In Bradley WG, Daroff RB, Fenchel GM, Marsden CD, editors: Neurology in Clinical Practice: The Neurological Disorders, 2nd ed, Boston: Butterworth-Heinemann, 1996.
Osborn AG. Diagnostic Neuroradiology. St Louis: Mosby–Year Book; 1994.
Simeone FA. Intradural tumors. In Rothman RH, Simeone FA, editors: The Spine, 3rd ed, Philadelphia: WB Saunders, 1992.