CHAPTER 19. LUMBAR PUNCTURE
Indications155
Contraindications156
Equipment156
Structures through which the spinal needle passes158
Practical procedure158
Post-procedure investigations163
Complications164
Suggested reading164
In 1885 the American neurologist James Leonard Corning (1855–1923) performed a lumbar puncture on a dog and injected cocaine in what proved to be the first demonstration of spinal anaesthesia. Heinrick Quincke (1842–1922) of Quincke’s sign fame (capillary nailbed pulsation of aortic regurgitation) reported a lumbar puncture performed in 1888 for hydrocephalus-associated headaches 1 month before Walter Essex Wynter’s (1860–1945) publication in the Lancet in 1889. Wynter described four cases of cerebrospinal fluid (CSF) aspiration in children with TB meningitis at the Middlesex Hospital, London which he performed by cut down to dura at L2 and placement of Southey’s tubes for drainage.
INTRODUCTION
Lumbar puncture in the ward-based setting is usually performed in order to obtain CSF for investigation of neuroaxial conditions. Lumbar puncture is also commonly undertaken in order to provide spinal anaesthesia for operative procedures on the lower abdomen and lower limbs. Additionally lumbar puncture may be used for delivering intrathecal chemotherapy. However, these latter two situations are outside the remit of this chapter.
INDICATIONS
CONTRAINDICATIONS
• Coagulopathy (recent aspirin, heparin last 12 hours, international normalized ratio above 1.2, activated partial thromboplastin time ratio above 1.2).
• Local sepsis over puncture site.
• Raised intracranial pressure (see Tip Box).
• Cardiorespiratory compromise.
• Suspected spinal cord mass or intracranial lesion (see Tip Box).
• Spinal cord compression.
• Lack of consent.
• Spinal cord deformities are a relative contraindication depending upon the spinal anatomy and the experience of the operator (e.g. scoliosis). If you are unsure of the anatomy, consult a senior colleague.
 Tip Box
Tip Box
When to perform a head CT prior to lumbar puncture:
• >60 years of age.
• Symptoms or signs of raised intracranial pressure (persistent vomiting, history of recent seizure(s), reduced Glasgow coma scale, papilloedema).
• Focal abnormal neurology on examination.
• Immunocompromised (e.g. HIV positive).
• Recent head injury.
• When a possible intracranial bleed is the preliminary diagnosis (in which case a negative computerized tomography of the head should precede subsequent lumbar puncture).
EQUIPMENT
 Tip Box
Tip Box
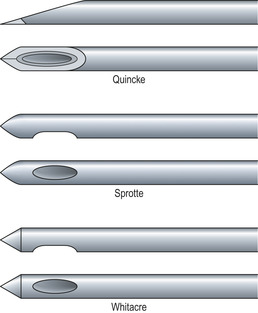
Lumbar puncture needles are divided into two types: ‘atraumatic’ needles (e.g. Sprotte or Whitacre) and typical ‘cutting’ needles (Quincke) (Fig. 19.1).
 |
| Fig. 19.1 |
The ‘non-cutting’ tip of atraumatic needles is designed to part the dural fibres rather than shear them, and so upon removal of the needle from the dura a smaller hole remains than with a cutting needle. This reduces the amount of CSF loss post-lumbar puncture, and several randomized double-blind studies have been published showing that post-lumbar puncture headaches are reduced ten-fold when using atraumatic needles.
Given their non-cutting tip design, atraumatic needles do not puncture the skin as freely as a typical Quincke needle. They require an introducer needle to puncture the skin, through which the atraumatic needle is passed. If you go on to use atraumatic needles, familiarize yourself with the apparatus prior to use.
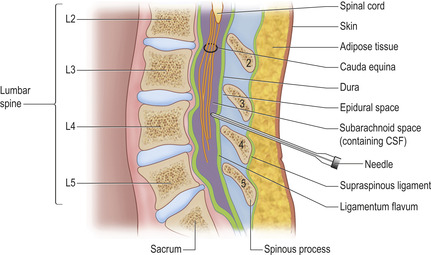
STRUCTURES THROUGH WHICH THE SPINAL NEEDLE PASSES
The lumbar puncture needle passes through the following tissues in sequence to reach the subarachnoid space (Fig. 19.2): skin, subcutaneous tissue, the supraspinal ligament, the interspinal ligament, the ligamentum flavum, the dura mater and finally the arachnoid mater.
PRACTICAL PROCEDURE
• Obtain consent.
• Provide analgesia, e.g. paracetamol or codeine.
POSITIONING
Correct positioning of the patient is paramount in successfully performing a lumbar puncture.
• Lateral decubitus/‘foetal’ position – Ensuring that the bed is flat, ask the patient to lie on their left side with their back flat to the edge of the bed and their shoulders square to their hips. Ensure that their knees are drawn into their chest and head tucked to chin to help open up the spinous processes. Once in position place a pillow under the head of the patient. It is also often helpful to have a pillow between the legs to avoid pelvic rotation, the aim being to ensure that the patient’s back is flat flush to the edge of the bed.
• Seated position – This position is normally used in the event of a failed procedure in the lateral decubitus position. It has the advantage that there is less distortion of spinal anatomy, but with the disadvantage that the CSF pressure cannot be reliably ascertained in this position. Ask the patient to sit on the edge of the bed holding a pillow into their chest so that their spine is flexed forwards. Place their feet on a stool and point their chin to their chest to maximize spinal flexion. Alternatively, ask them to straddle a chair and lean onto a pillow ensuring the spine is flexed so the intervertebral spaces are open adequately.
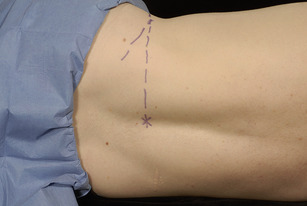
The lower border of the spinal cord ends at the level of L1–2 at the conus medullaris. To ensure no damage to the cord, the spinal needle is inserted into the L3–4 intervertebral space. With the patient in the correct position, palpate the vertebral column at the L3–4 intervertebral space by joining an imaginary vertical line between the iliac crests across the back (Fig. 19.3). Mark this space with a skin pen so that it is clearly indicated.
 Tip Box
Tip Box
Should you fail to obtain CSF via the L3–4 interspace, try one intervertebral space higher at L2–3.
PROCEDURE
• Number the specimen pots sequentially prior to specimen collection.
• Wash your hands, wear the sterile gown and gloves and lay out sterile environment and dressing pack.
• Check equipment:
— Familiarize yourself with the manometer directions (‘open and closed to the patient’ and ‘neutral position’), and assemble the manometer with the 3-way tap turned to the ‘closed to you’ direction.
 Tip Box
Tip Box
The 3-way tap is frequently very stiff for the initial few attempts at turning it and can consequently be cumbersome to manipulate during the procedure. For this reason, manipulate and loosen the 3-way tap between these positions several times prior to use.
• Clean the lumbar area – remember to clean spirally outwards from the central target to the periphery to avoid bringing dirty solution in contact with a previously cleaned area. Ensure that all cleaning fluid is wiped away prior to needle insertion.
• Place a drape over the iliac crest, enabling palpation of anatomical landmarks during the procedure whilst remaining sterile.
• Ensure you are comfortable. Most doctors sit on a chair, as standing in a very flexed position (especially if you are tall) is awkward and less controlled. Alter the bed height to help your personal comfort.
• Infiltrate local anaesthetic subcutaneously with an orange needle.
• Infiltrate local anaesthetic with a green needle between the spinous processes, to a maximum depth of approximately 2 cm.
 Tip Box
Tip Box
Allow sufficient time for the anaesthetic block to take effect. If the superficial tissues are appropriately anaesthetized, lumbar puncture should be a painless procedure.
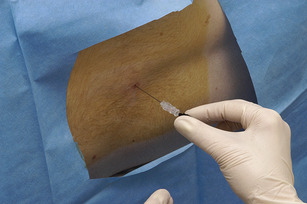
• Feel the disc interspace at level L3–4 and slowly insert the lumbar puncture needle bevel-up, pointing towards the patient’s umbilicus.
• Advance the needle for the first 2 cm, and thereafter periodically remove the stylet for approximately every 3 mm you advance (Fig. 19.4) to check for CSF (or blood if a venous plexus has been hit – in this case remove the needle).
• You may feel slight resistance passing through the ligamentum flavum before a ‘push/give’ through the dura into the subarachnoid space (usually at around 5–8 cm deep from the skin depending upon body habitus).
• On removing the stylet you will note CSF backflow through the needle. The CSF flow will depend on the gauge of the needle. The flow should be continuous. It might be initially blood stained but should clear (unless the diagnosis is subarachnoid haemorrhage).
• CSF opening pressure is measured by attaching the manometer (Fig. 19.5). This should be done as soon as one is satisfied that the CSF flow is continuous, although too much CSF free flow and loss will reduce the CSF pressure. Allow CSF to rise through the manometer until it completely stops rising. Record this level post-procedure.
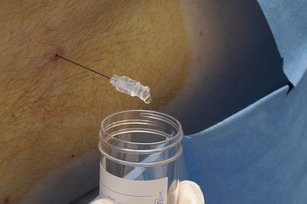
• Switch the manometer to the ‘closed to patient’ direction and collect the first 5–10 drops of CSF in container 1.
• Remove the manometer and collect further samples of CSF in the corresponding numbered bottles, collecting 5–10 drops of CSF in each bottle (Fig. 19.6).
• When collected, replace the stylet and slowly remove the needle. Place a plaster over the site.
• Lie the patient on their back for an hour, remind them that they may feel light-headed or have a headache post-procedure.
• Prescribe analgesia, encourage oral fluid intake (if poor intake consider intravenous fluids, especially as the patient is lying flat).
 Tip Box
Tip Box
• If you are having trouble getting into the subarachnoid space (i.e. a dry tap), try rotating the needle, pulling the needle back or manoeuvring the needle slowly into different positions. If this fails, try the L2–3 interspace or move the patient into another position (see positioning above).
• If you hit bone or the patient experiences pain, slowly withdraw slightly and change the horizontal angle of trajectory of the needle.
• The amount of CSF needed by each laboratory varies. CSF cell count can be achieved with a few drops. However, virology, microbiology and cytology usually require at least 10 drops.
• It is prudent to take an extra specimen bottle for a spare CSF sample to save for any retrospective investigations or tests that require a large volume of CSF (and thus avoid a repeated lumbar puncture).
POST-PROCEDURE INVESTIGATIONS
Use a clear specimen bottle unless stated otherwise.
• Macroscopic appearance of CSF (normal is ‘gin clear’).
• CSF opening pressure (recorded on manometer).
• Cell count – white blood cell (including differential) and red blood cell counts.
 Tip Box
Tip Box
In suspected subarachnoid haemorrhage, send bottles one and three for cell count. If the red blood cell count falls from bottle one to three this suggests a traumatic tap rather than blood truly within the CSF.
• Xanthochromia – spectrophotometry of sequential samples. The container should be shielded from external light by wrapping it in tin foil.
• CSF smear, Gram stain, MC+S, cell count – culture for bacteria, fungi, acid-fast bacilli (AFB).
• Glucose – in fluoride–oxalate tube. Send a concurrent serum glucose sample for accurate interpretation of the CSF glucose result (i.e. paired with CSF glucose).
• Protein and lactate dehydrogenase (LDH) levels.
• Viral PCR.
• Electrophoresis for oligoclonal bands.
• India ink stain for Cryptococcus neoformans.
• Treponemal titres for neurosyphilis.
COMPLICATIONS
• Post-procedure headache.
• Traumatic puncture.
• Puncture of lumbar veins.
• Subdural haematoma.
• Subarachnoid haemorrhage.
• Infection (meningitis).
• Epidural haematoma.
SUGGESTED READING
Kleyweg, R.P.; Hertzberger, L.I.; Carbaat, P.A.; et al., Significant reduction in post-lumbar puncture headache using an atraumatic needle. A double-blind, controlled clinical trial, Cephalalgia 18 (9) (1998) 635–637; discussion 591.
Müller, B.; Adelt, K.; Reichmann, H.; Toyka, K., Atraumatic needle reduces the incidence of post-lumbar puncture syndrome, J Neurol 241 (6) (1994) 376–380.
Strupp, M.; Schueler, O.; Straube, A.; et al., “Atraumatic” Sprotte needle reduces the incidence of post-lumbar puncture headaches, Neurology 57 (12) (2001) 2310–2312.