Pronation Therapy
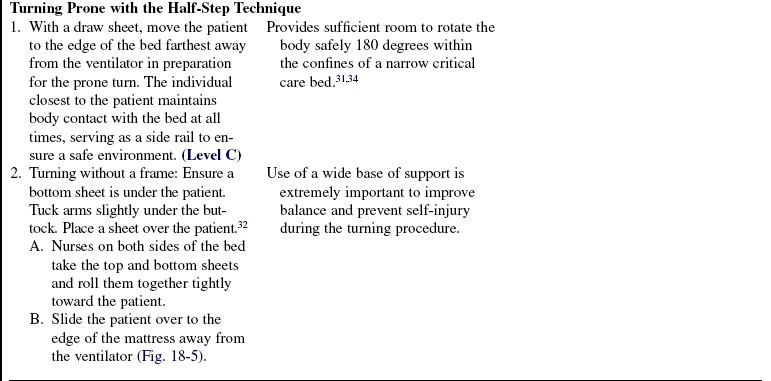
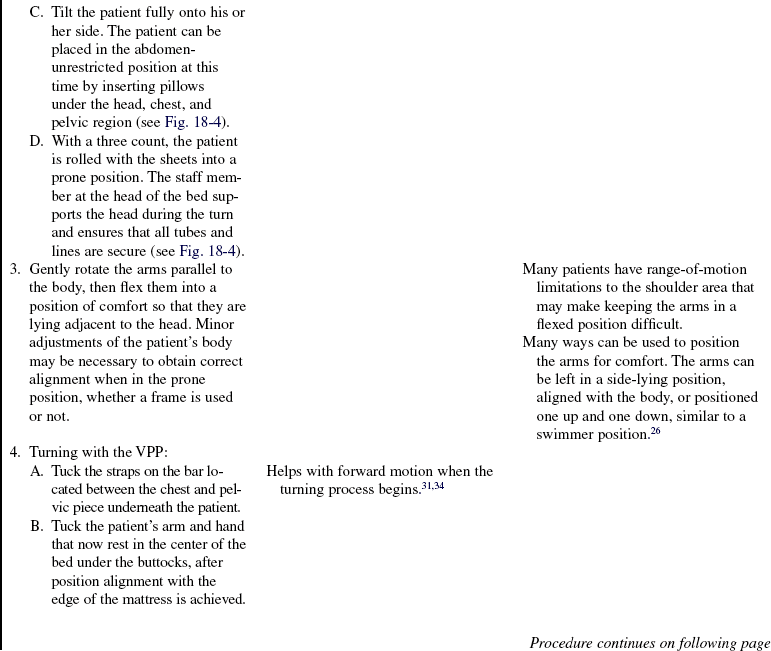
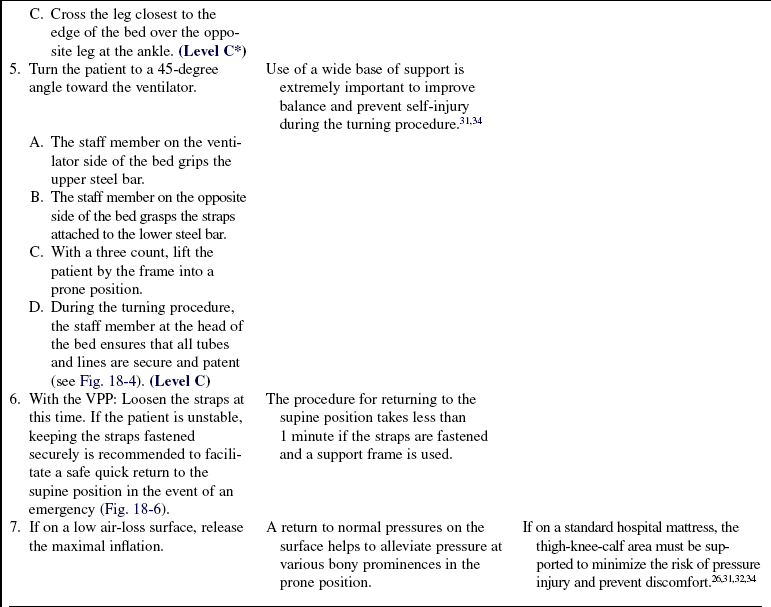
PREREQUISITE NURSING KNOWLEDGE
• Prone positioning is used as an adjunct short-term supportive therapy in an attempt to recruit alveoli to improve gas exchange in a critically ill patient with severely compromised lungs.
 On the basis of numerous studies and three recent meta-analyses, patients with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) placed in the prone position significantly increase partial pressure of arterial oxygen (PaO2) to fraction of inspired oxygen (FiO2) when compared with the supine position. The greatest effect was seen within the first day, with continuing benefit with subsequent prone position placements up to 4 days.1–5,7,9,10,13,18,22,24,28,30,32
On the basis of numerous studies and three recent meta-analyses, patients with acute lung injury (ALI) and acute respiratory distress syndrome (ARDS) placed in the prone position significantly increase partial pressure of arterial oxygen (PaO2) to fraction of inspired oxygen (FiO2) when compared with the supine position. The greatest effect was seen within the first day, with continuing benefit with subsequent prone position placements up to 4 days.1–5,7,9,10,13,18,22,24,28,30,32
 Two of the three meta-analyses showed no improvement in mortality with the use of the prone position.1,28 One showed significant improvement in mortality in patients with severe ARDS and a higher severity of illness.2
Two of the three meta-analyses showed no improvement in mortality with the use of the prone position.1,28 One showed significant improvement in mortality in patients with severe ARDS and a higher severity of illness.2
 No significant difference was seen in number of days on mechanical ventilation with the prone position.1,2,28 One meta-analysis showed significant reduction in the incidence of ventilator-associated pneumonia (VAP) in the prone position28; another showed a trend toward significance in VAP reduction of 23% (P = 0.09)1; and the third showed no difference in VAP rates between the two positions.2
No significant difference was seen in number of days on mechanical ventilation with the prone position.1,2,28 One meta-analysis showed significant reduction in the incidence of ventilator-associated pneumonia (VAP) in the prone position28; another showed a trend toward significance in VAP reduction of 23% (P = 0.09)1; and the third showed no difference in VAP rates between the two positions.2
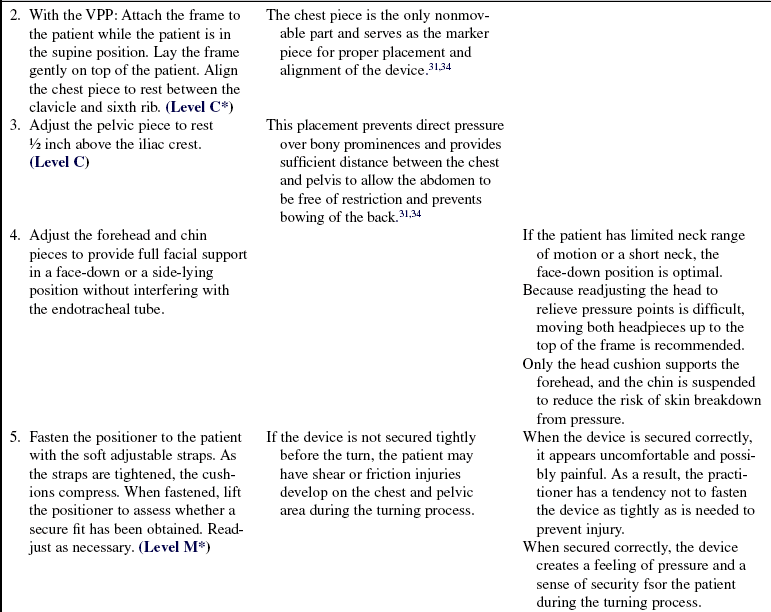
 Part of the variability between the analyses has to do with the inclusion criteria used to choose the studies incorporated in the meta-analysis. The analysis by Alsaghir and Martian2 resulted in five studies that met inclusion criteria out of 63 with a total of 1316 patients. The meta-analysis preformed by Abroung and group1 included 5 trials out of 72 with a total of 1372 patients, and the analysis by Sud and colleagues28 included 13 trials out of 1676 studies with analysis being performed on 1559 patients.
Part of the variability between the analyses has to do with the inclusion criteria used to choose the studies incorporated in the meta-analysis. The analysis by Alsaghir and Martian2 resulted in five studies that met inclusion criteria out of 63 with a total of 1316 patients. The meta-analysis preformed by Abroung and group1 included 5 trials out of 72 with a total of 1372 patients, and the analysis by Sud and colleagues28 included 13 trials out of 1676 studies with analysis being performed on 1559 patients.
• The last major outcomes to be examined in the meta-analyses were the presence of significant complications when the prone position was compared with the supine position. Two of the three analyses reported on complications. One analysis showed a statistically significant higher risk for the development of pressure ulcers in the prone position,28 and Abroung and group1 showed no significant difference in major airway complications in the prone position. All three meta-analyses concluded that an adequately sized study optimizing the duration of proning and ventilation strategy is warranted to be able to draw definitive conclusions. A phase III trial looking at these issues has been completed but the results have not been published to date. To enhance an understanding of how prone positioning may affect gas exchange, understanding the factors that influence the distribution of ventilation and perfusion within the lung is important.
• Distribution of ventilation: Regional pleural pressures and local lung compliance jointly determine the volume of air distributed regionally throughout the lungs. Three major factors—gravity and weight of the lung, compliance, and heterogeneously diseased lungs—influence regional distribution. In an upright individual, the pleural pressure next to the diaphragm is less negative than at the pleural apices. The weight of the lung and the effect of gravity on the lung and its supporting structures in the upright position create this difference in regional pleural pressures. This relationship results in a higher functional residual capacity (FRC) in the nondependent zone or the apices, redirecting ventilation to the dependent zone.8,15,35 When body position changes, changes occur in regional pleural pressures, compliance, and volume distribution. In the supine position, distribution becomes more uniform from apex to base. The ventilation of dependent lung units exceeds that of nondependent lung units, however, and a reduction in FRC is seen.8,35 The two factors that contribute to the reduction in FRC seen in moving from the upright to the supine position include: 1, the pressure of the abdominal contents on the diaphragm8; and 2, the position of the heart and the relationship of the supporting structures to the lung and its influence on pleural pressure gradients.17,20
 The first factor to influence pleural pressure, regional volumes, and FRC is the impact of the abdominal contents on the function of the diaphragm. In spontaneously breathing individuals in the supine position, the diaphragm acts as a shield against the pressure exerted by the abdominal contents, preventing the contents from interfering with dependent lung volume distribution. When patients are mechanically ventilated with positive-pressure breaths, sedated, or paralyzed, the active muscle tension in the diaphragm is lost, which results in a cephalad displacement of the diaphragm and allows abdominal pressures to decrease dependent lung volume inflation and FRC.8,15 The only way to modify this influence is to change the posture to a prone position with the abdomen unsupported.8,24
The first factor to influence pleural pressure, regional volumes, and FRC is the impact of the abdominal contents on the function of the diaphragm. In spontaneously breathing individuals in the supine position, the diaphragm acts as a shield against the pressure exerted by the abdominal contents, preventing the contents from interfering with dependent lung volume distribution. When patients are mechanically ventilated with positive-pressure breaths, sedated, or paralyzed, the active muscle tension in the diaphragm is lost, which results in a cephalad displacement of the diaphragm and allows abdominal pressures to decrease dependent lung volume inflation and FRC.8,15 The only way to modify this influence is to change the posture to a prone position with the abdomen unsupported.8,24
 The second factor to influence pleural pressure, regional volumes, FRC, and compliance is the position of the heart and supporting structures. The heart and the diaphragm extend farther dorsally and rest against a rigid spine in the supine position, squeezing the lungs beneath them. This pressure on the lungs generates more positive pleural pressures, which results in a greater propensity to collapse of the alveoli at end expiration. In the prone position, the heart and upper abdomen rest against the sternum, exerting less weight on the lung tissue. Less effect on pleural pressure occurs, which leaves the pleural pressures more negative, maintaining open alveoli.17,21,24
The second factor to influence pleural pressure, regional volumes, FRC, and compliance is the position of the heart and supporting structures. The heart and the diaphragm extend farther dorsally and rest against a rigid spine in the supine position, squeezing the lungs beneath them. This pressure on the lungs generates more positive pleural pressures, which results in a greater propensity to collapse of the alveoli at end expiration. In the prone position, the heart and upper abdomen rest against the sternum, exerting less weight on the lung tissue. Less effect on pleural pressure occurs, which leaves the pleural pressures more negative, maintaining open alveoli.17,21,24
 A third factor that contributes to the distribution of volume is heterogeneously or unevenly distributed diseased lung. The acute respiratory distress syndrome lung weight is increased twofold to threefold from normal. The increased weight is from edema and the resulting hydrostatic forces. A progressive squeezing of gas along a vertical-dorsal axis results. This decrease of regional inflation along the vertical axis results in dependent or dorsal lung collapse. In the prone position, these densities shift. The pattern almost completely reverts toward normal. The inflation gradient is less steep, and the difference results in a more homogeneous regional inflation. This inflation may be related to a redistribution of gas because of the change in hydrostatic forces caused by differences in pleural pressure, as described previously.9,11,24
A third factor that contributes to the distribution of volume is heterogeneously or unevenly distributed diseased lung. The acute respiratory distress syndrome lung weight is increased twofold to threefold from normal. The increased weight is from edema and the resulting hydrostatic forces. A progressive squeezing of gas along a vertical-dorsal axis results. This decrease of regional inflation along the vertical axis results in dependent or dorsal lung collapse. In the prone position, these densities shift. The pattern almost completely reverts toward normal. The inflation gradient is less steep, and the difference results in a more homogeneous regional inflation. This inflation may be related to a redistribution of gas because of the change in hydrostatic forces caused by differences in pleural pressure, as described previously.9,11,24
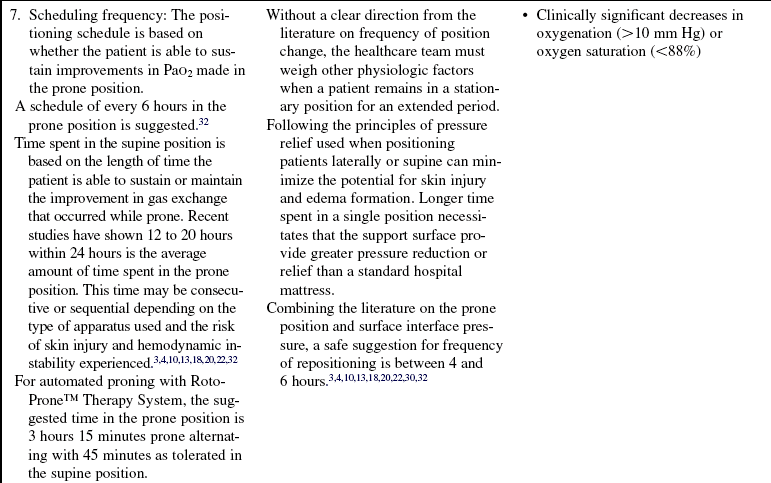
• Distribution of perfusion: Similar to ventilation, regional distribution of perfusion is influenced by three factors: cardiac output, pulmonary vascular resistance, and gravity or body position.
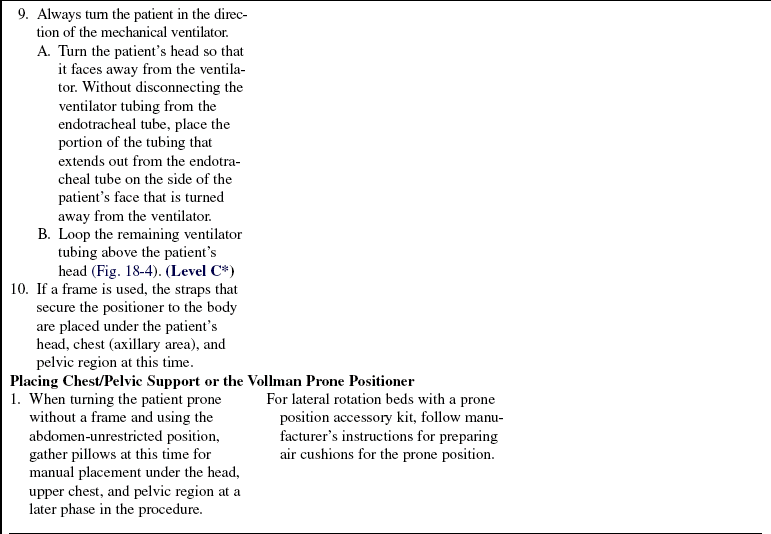
• In an upright individual, blood flow decreases as it moves from base to apex with virtually no flow at the apex. This decrease is caused by the influence of gravity on pulmonary vascular pressures within the lung (Fig. 18-1).
Figure 18-1 Zone model of the lung. Three-zone model of the lung is used to explain distribution of blood flow based on pressure variations. (From West JB, Dollery CT, Naimark A: Distribution of blood flow in isolated lung; relation to vascular and alveolar pressures, J Appl Physiol, 19:713-724, 1964.)
 In zone 1, near the apex, alveolar pressure exceeds arterial pressure, creating little or no flow.
In zone 1, near the apex, alveolar pressure exceeds arterial pressure, creating little or no flow.
 In zone 2, the pulmonary artery pressure exceeds alveolar pressure, which exceeds the venous pressure. Blood flow in this area occurs based on the differences in pressure between the arterial and alveolar bed.
In zone 2, the pulmonary artery pressure exceeds alveolar pressure, which exceeds the venous pressure. Blood flow in this area occurs based on the differences in pressure between the arterial and alveolar bed.
 In zone 3, the arterial pressure is greater than the venous pressure, which is greater than the alveolar pressure. In this zone, the influence of the alveolar pressure on blood flow is reduced, resulting in freedom of flow in this region.35,36
In zone 3, the arterial pressure is greater than the venous pressure, which is greater than the alveolar pressure. In this zone, the influence of the alveolar pressure on blood flow is reduced, resulting in freedom of flow in this region.35,36
• In supine and lateral positions, apical region blood flow changes. No real change is seen in basilar units, but a greater dependent versus nondependent blood flow occurs. In the prone position, a marked reduction occurs, however, in the gravitational perfusion gradient, which suggests no gravity-dependent benefit to flow in the prone position.21
• On the basis of the current available data as outlined here, changes in oxygenation seem to be related to differences in the regional inflation/ventilation of the lung while prone and are not related to a redistribution of blood flow.6,17,23
• Suggested criteria for use of the prone position include:
 Consider use of the prone position for patients with ARDS who need potentially injurious levels of FiO2 or plateau pressure, provided they are not put at risk from positional changes6
Consider use of the prone position for patients with ARDS who need potentially injurious levels of FiO2 or plateau pressure, provided they are not put at risk from positional changes6
 PaO2/FiO2 ratio less than 200 on a FiO2 greater than 50% with sufficient positive end-expiratory pressure used to recruit alveoli
PaO2/FiO2 ratio less than 200 on a FiO2 greater than 50% with sufficient positive end-expiratory pressure used to recruit alveoli
• Contraindications and precautions to manual pronation therapy include the following3,7,23,26,31,32:
 Patient unable to tolerate a head-down position
Patient unable to tolerate a head-down position
 Increased intracranial pressure
Increased intracranial pressure
 Unstable spine (unless Stryker Frame [Stryker Medical], Kalamazoo, MI used)
Unstable spine (unless Stryker Frame [Stryker Medical], Kalamazoo, MI used)
 Patient with hemodynamically unstable condition (as defined by a systolic blood pressure less than 90 mm Hg) with fluid and vasoactive support in place
Patient with hemodynamically unstable condition (as defined by a systolic blood pressure less than 90 mm Hg) with fluid and vasoactive support in place
 With use of a support frame, patient weight greater than 135 kg
With use of a support frame, patient weight greater than 135 kg
 Weight 160 kg or greater (weigh the risk/benefit ratio for the patient and staff)
Weight 160 kg or greater (weigh the risk/benefit ratio for the patient and staff)
 Extracorporeal membrane oxygenator cannula placement problems
Extracorporeal membrane oxygenator cannula placement problems
 Open chest or unstable chest wall
Open chest or unstable chest wall
• Absolute contraindications for use of Automated Prone Positioning RotoProne™ Therapy System (KCI Licensing, Inc.) include:
 Unstable cervical, thoracic, lumbar, pelvic, skull, or facial fractures
Unstable cervical, thoracic, lumbar, pelvic, skull, or facial fractures
 Uncontrolled intracranial pressure (ICP)
Uncontrolled intracranial pressure (ICP)
 Patient weight less than 40 kg (88 lb)
Patient weight less than 40 kg (88 lb)
• Relative contraindications for use of Automated Prone Positioning RotoProne™ Therapy System (must weigh risk and benefits) include:
 Patients in prone position with open sternal wound or thoracic postsurgical incision
Patients in prone position with open sternal wound or thoracic postsurgical incision
 Intolerance to face-down position
Intolerance to face-down position
 Any implant that potentially increases risk of skin breakdown, including, but not limited to, breast implants or penile prosthesis
Any implant that potentially increases risk of skin breakdown, including, but not limited to, breast implants or penile prosthesis
• The use of the prone position is discontinued when the patient no longer shows a positive response to the position change or mechanical ventilation support has been optimized. The literature has not clearly identified when the use of prone positioning should be discontinued. One suggestion for discontinuation is when the patient’s PaO2/FiO2 ratio is greater than 200 on less than 50% FiO2 and less than or equal to 10 cm of H2O of positive end-expiratory pressure. With use of the RotoProne™ Therapy System Surface, weaning from the prone position is recommended. Increase supine time while decreasing time in the prone position until the patient is able to tolerate 24 hours in the supine position with no decrease in oxygenation response. The patient can then be taken off the RotoProne and placed on an appropriate surface to achieve patient goals.
EQUIPMENT
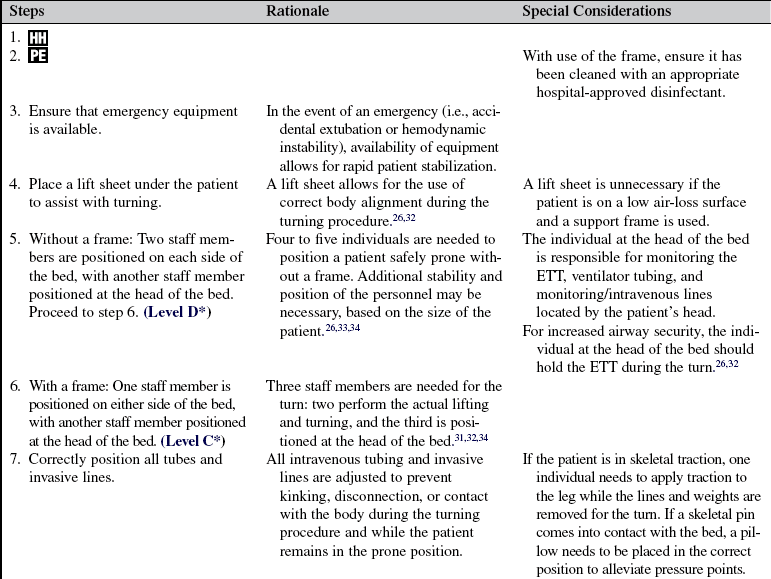
• Vollman Prone Positioner (VPP; Hill-Rom, Inc, Batesville, IN; Fig. 18-2): weight limit per manufacturer’s recommendation, 300 1b
Additional equipment (to have available depending on patient need) includes the following:
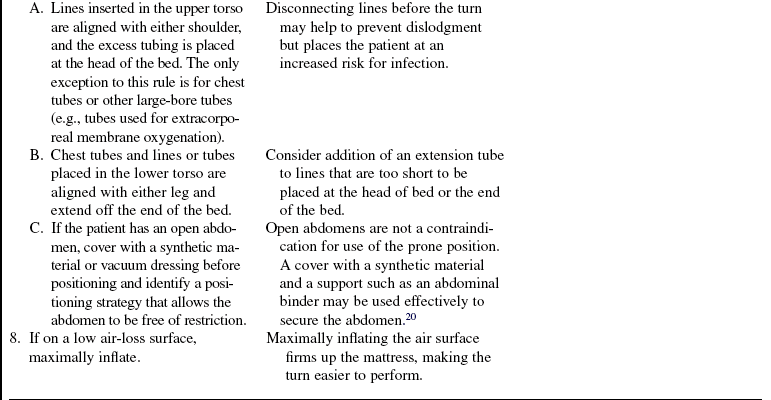
• RotoProne™ Therapy System for use in all patient populations (Fig. 18-3): weight limit per manufacturer’s recommendations, 88 to 350 lb (40 to 159 kg); height limit per manufacturer’s recommendations, 54 to 78 inches (140 to 200 cm)
• Stryker Frame for use in patients with unstable spines, if available: weight limit per manufacturer’s recommendations
PATIENT AND FAMILY EDUCATION
• Explain to the patient and family the patient’s lung/oxygenation problem and the reason for the use of the prone position.  Rationale: This explanation decreases patient and family anxiety by providing information and clarification.
Rationale: This explanation decreases patient and family anxiety by providing information and clarification.
• Explain the care procedure to the patient and family, including positioning procedure, perceived benefit, frequency of assessments, expected response, and parameters for discontinuation of the positioning technique and equipment (if special bed or frame is initiated).  Rationale: This communication provides an opportunity for the patient and family to verbalize concerns or ask questions about the procedure.
Rationale: This communication provides an opportunity for the patient and family to verbalize concerns or ask questions about the procedure.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess time interval from injury to position change.  Rationale: A trial of prone positioning should be performed within 48 hours in the course of ARDS to assess the patient’s level of response. A positive response is defined by a PaO2/FiO2 ratio greater than 20% or a PaO2 greater than 10 mm Hg.3,24 If initial positioning does not elicit a positive response, however, periodic attempts to assess the patient’s responsiveness throughout the course of lung injury should not be ruled out. Response to severe position change has been noted at all stages of ARDS.
Rationale: A trial of prone positioning should be performed within 48 hours in the course of ARDS to assess the patient’s level of response. A positive response is defined by a PaO2/FiO2 ratio greater than 20% or a PaO2 greater than 10 mm Hg.3,24 If initial positioning does not elicit a positive response, however, periodic attempts to assess the patient’s responsiveness throughout the course of lung injury should not be ruled out. Response to severe position change has been noted at all stages of ARDS.
• Assess the hemodynamic status of the patient to identify the ability to tolerate a position change.26  Rationale: Imbalances between oxygen supply and demand must be addressed before the pronation procedure to offset any increases in oxygen demand that may be created by the physical turning. The final decision to place a patient with a hemodynamically unstable condition prone rests with the physician or advanced practice nurse who must weigh the risks against the potential benefits of the prone position.
Rationale: Imbalances between oxygen supply and demand must be addressed before the pronation procedure to offset any increases in oxygen demand that may be created by the physical turning. The final decision to place a patient with a hemodynamically unstable condition prone rests with the physician or advanced practice nurse who must weigh the risks against the potential benefits of the prone position.
• Assess mental status before use of the prone position.  Rationale: Agitation, whether caused by delirium, anxiety, or pain, can have a negative effect with the prone position. Nevertheless, agitation is not a contraindication for use of the prone position. The healthcare team should strive to manage the agitation effectively to provide a safe environment for the use of the prone position.
Rationale: Agitation, whether caused by delirium, anxiety, or pain, can have a negative effect with the prone position. Nevertheless, agitation is not a contraindication for use of the prone position. The healthcare team should strive to manage the agitation effectively to provide a safe environment for the use of the prone position.
• Assess size and weight load to determine the ability to turn within the narrow critical care bed frame and to weigh the potential risk of injury to the healthcare worker.  Rationale: When manually turning a patient prone in a hospital bed, with or without a frame, one must determine whether a 180-degree turn can be accomplished within the confines of the space available. Critical care bed frames are narrow, which makes completion of the turn difficult on patients who weigh more than 160 kg. The team must consider the potential for injury to the healthcare workers when making the decision to turn morbidly obese patients prone. With use of a special bed made specifically for prone positioning, follow the weight and height limitations recommended by the manufacturer.
Rationale: When manually turning a patient prone in a hospital bed, with or without a frame, one must determine whether a 180-degree turn can be accomplished within the confines of the space available. Critical care bed frames are narrow, which makes completion of the turn difficult on patients who weigh more than 160 kg. The team must consider the potential for injury to the healthcare workers when making the decision to turn morbidly obese patients prone. With use of a special bed made specifically for prone positioning, follow the weight and height limitations recommended by the manufacturer.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teachings. Answer questions as they arise and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Assess patient’s mental condition.  Rationale: Assessment of agitation with a reliable and valid scale and provide appropriate management before, during, and after the turn are key to accomplishing a safe procedure.
Rationale: Assessment of agitation with a reliable and valid scale and provide appropriate management before, during, and after the turn are key to accomplishing a safe procedure.
• Turn off the tube feeding 1 hour before the prone position turn.  Rationale: This action assists with gastric emptying and reduces the risk of aspiration during the turning procedure.35 Enteral feeding can be continued during prone position29; use of prokinetic agents or transpyloric feedings is recommended to prevent complications associated with vomiting.25
Rationale: This action assists with gastric emptying and reduces the risk of aspiration during the turning procedure.35 Enteral feeding can be continued during prone position29; use of prokinetic agents or transpyloric feedings is recommended to prevent complications associated with vomiting.25
• Before positioning the patient prone, the following care activities should be performed:
 Remove electrocardiogram leads from the anterior chest wall.
Remove electrocardiogram leads from the anterior chest wall.
 Perform eye care, including lubrication and taping of the eyelids closed in a horizontal fashion.
Perform eye care, including lubrication and taping of the eyelids closed in a horizontal fashion.
 Ensure the tongue is inside the patient’s mouth. If the tongue is swollen or protruding, insert a bite-block.
Ensure the tongue is inside the patient’s mouth. If the tongue is swollen or protruding, insert a bite-block.
 Ensure the tape or ties of the endotracheal tube or tracheotomy tube are secure. Changing of the ties may be necessary on return to the supine position if they are not secure. If adhesive tape is used to secure the endotracheal tube, consider double taping or wrapping completely around the head because increased salivary drainage occurs in the prone position and may loosen the adhesive.26,32 Commercial endotracheal tube (ETT) securement devices are not recommended for use during prone positioning because of possibility of increased skin breakdown and breakdown of adhesive from increased salivary drainage.16
Ensure the tape or ties of the endotracheal tube or tracheotomy tube are secure. Changing of the ties may be necessary on return to the supine position if they are not secure. If adhesive tape is used to secure the endotracheal tube, consider double taping or wrapping completely around the head because increased salivary drainage occurs in the prone position and may loosen the adhesive.26,32 Commercial endotracheal tube (ETT) securement devices are not recommended for use during prone positioning because of possibility of increased skin breakdown and breakdown of adhesive from increased salivary drainage.16
 If a wound dressing on the anterior body is due to be changed during the prone position sequence, perform the dressing change before the turn. If saturated on return from the prone position, the dressing needs to be changed.
If a wound dressing on the anterior body is due to be changed during the prone position sequence, perform the dressing change before the turn. If saturated on return from the prone position, the dressing needs to be changed.
 Empty ileostomy/colostomy bags before positioning. Placement of the drainage bag to gravity drainage and padding around the stoma to prevent pressure directly on stoma are recommended.
Empty ileostomy/colostomy bags before positioning. Placement of the drainage bag to gravity drainage and padding around the stoma to prevent pressure directly on stoma are recommended.
 Capnography monitoring is suggested to help ensure proper positioning of the tube during the turning procedure and in the prone position.
Capnography monitoring is suggested to help ensure proper positioning of the tube during the turning procedure and in the prone position.
•  Rationale: These activities prevent areas of pressure and potential skin breakdown; avoid complications related to injury or accidental extubation; and promote the delivery of comprehensive care before, during, and after the pronation therapy.26,31,32,34
Rationale: These activities prevent areas of pressure and potential skin breakdown; avoid complications related to injury or accidental extubation; and promote the delivery of comprehensive care before, during, and after the pronation therapy.26,31,32,34
References
1. Abroung, F, et al, The effect of prone positioning in acute respiratory distress syndrome or acute lung injury. a meta-analysisareas of uncertainty and recommendations for research. Intensive Care Med. 2008; 34(6):1002–1011.
2. Alsaghir, AH, Martian, CM, Effect of prone positioning in patients with acute respiratory distress syndrome. a meta-analysis. Crit Care Med 2008; 36:603–609.
![]() 3. Chatte, G, et al. Prone position in mechanically ventilated patients with severe acute respiratory failure. Am J Respir Crit Care Med. 1997; 155:473–478.
3. Chatte, G, et al. Prone position in mechanically ventilated patients with severe acute respiratory failure. Am J Respir Crit Care Med. 1997; 155:473–478.
4. Curley, MA, et al, Effect of prone positioning on clinical outcomes in children with acute lung injury. a randomized controlled trial. JAMA 2005; 294:229–237.
![]() 5. Curley, MAQ, Prone positioning of patients with acute respiratory distress syndrome. a systematic review. Am J Crit Care 1999; 8:397–405.
5. Curley, MAQ, Prone positioning of patients with acute respiratory distress syndrome. a systematic review. Am J Crit Care 1999; 8:397–405.
6. Dellinger, PR, et al, Surviving sepsis campaign. international guidelines for management of severe sepsis and septic shock2008. Crit Care Med 2008; 36:296–327.
![]() 7. Fridrich, P, et al. The effects of long-term prone positioning in patients with trauma induced adult respiratory distress syndrome. Anesth Analg. 1996; 83:1206–1211.
7. Fridrich, P, et al. The effects of long-term prone positioning in patients with trauma induced adult respiratory distress syndrome. Anesth Analg. 1996; 83:1206–1211.
![]() 8. Froese, AB, Bryan, AC. Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology. 1974; 41:242–255.
8. Froese, AB, Bryan, AC. Effects of anesthesia and paralysis on diaphragmatic mechanics in man. Anesthesiology. 1974; 41:242–255.
![]() 9. Gattinoni, L, et al. Body position changes redistribute lung computed tomographic density in patients with acute respiratory failure. Anesthesiology. 1991; 74:15–23.
9. Gattinoni, L, et al. Body position changes redistribute lung computed tomographic density in patients with acute respiratory failure. Anesthesiology. 1991; 74:15–23.
![]() 10. Gattinoni, L, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001; 345:568–573.
10. Gattinoni, L, et al. Effect of prone positioning on the survival of patients with acute respiratory failure. N Engl J Med. 2001; 345:568–573.
![]() 11. Gattinoni, L, et al. Relationships between lung computed tomographic density, gas exchange and PEEP in acute respiratory failure. Anesthesiology. 1988; 69:824–832.
11. Gattinoni, L, et al. Relationships between lung computed tomographic density, gas exchange and PEEP in acute respiratory failure. Anesthesiology. 1988; 69:824–832.
12. Goldhill, DR, Imhoff, M, McLean, B, et al, Rotational bed therapy to prevent and treat respiratory complications. a review and meta analysis. Am J Crit Care 2007; 16:50–62.
![]() 13. Guerin, C, et al, Effects of systematic prone positioning in hypoxemic acute respiratory failure. a randomized controlled trial. JAMA 2004; 292:2379–2387.
13. Guerin, C, et al, Effects of systematic prone positioning in hypoxemic acute respiratory failure. a randomized controlled trial. JAMA 2004; 292:2379–2387.
![]() 14. Harcomb, C. Nursing patient with ARDS in prone position. Nurs Stand. 2004; 18(19):33–39.
14. Harcomb, C. Nursing patient with ARDS in prone position. Nurs Stand. 2004; 18(19):33–39.
15. Kaneko, K, et al. Regional distribution of ventilation and perfusion as a function of body position. J Appl Physiol. 1966; 21:767–777.
16. Laux, L, McGonigal, M, Thieret, T, et al. Use of prone positioning in a patient with acute respiratory distress syndrome. Crit Care Nurs Q. 2008; 31(2):178–183.
17. Malbouisson, LM, et al. Role of the heart in the loss of aeration characterizing lower lobes in acute respiratory distress syndrome. Am J Respir Crit Care Med. 2005; 161:2005–2012.
18. Mancebo, J, et al. A multicenter trial of prolonged prone ventilation in severe acute respiratory distress syndrome. Am J Respir Crit Care Med. 2006; 173:1233–1239.
19. Marklew, A. Body positioning and its effect on oxygenation—a literature review. Nurs Crit Care. 2006; 11(1):16–22.
![]() 20. Murray, TA, Patterson, LA. Prone positioning of trauma patients with acute respiratory distress syndrome and open abdominal incisions. Crit Care Nurse. 2002; 22:52–56.
20. Murray, TA, Patterson, LA. Prone positioning of trauma patients with acute respiratory distress syndrome and open abdominal incisions. Crit Care Nurse. 2002; 22:52–56.
![]() 21. Mutoh, T, et al. Prone position alters the effect of volume overload on regional pleural pressures and improves hypoxemia in pigs in vivo. Am Rev Respir Dis. 1992; 146:300–306.
21. Mutoh, T, et al. Prone position alters the effect of volume overload on regional pleural pressures and improves hypoxemia in pigs in vivo. Am Rev Respir Dis. 1992; 146:300–306.
22. Papazian, L, et al. Comparison of prone positioning and high frequency oscillatory ventilation of patients with acute respiratory distress syndrome. Crit Care Med. 2005; 33:2162–2171.
![]() 23. Pappert, D, et al. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994; 106:1511–1516.
23. Pappert, D, et al. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994; 106:1511–1516.
![]() 24. Pelosi, P, Brazzi, L, Gattinoni, L. Prone position in ARDS. Eur Respir J. 2002; 20:1017–1028.
24. Pelosi, P, Brazzi, L, Gattinoni, L. Prone position in ARDS. Eur Respir J. 2002; 20:1017–1028.
![]() 25. Reignier, J, Thenoz-Jost, N, Fiancette, M, et al. Early enteral nutrition in mechanically ventilated patients in the prone position. Crit Care Med. 2004; 32(1):94–99.
25. Reignier, J, Thenoz-Jost, N, Fiancette, M, et al. Early enteral nutrition in mechanically ventilated patients in the prone position. Crit Care Med. 2004; 32(1):94–99.
![]() 26. Rowe, C. Development of clinical guidelines for prone positioning in critically ill adults. Nurs Crit Care. 2004; 9(2):50–57.
26. Rowe, C. Development of clinical guidelines for prone positioning in critically ill adults. Nurs Crit Care. 2004; 9(2):50–57.
27. Sebat, F, Johnson, D, Shoffner, D, et al. Benefits, complications of prone position and utility of automated proning bed in the treatment of acute lung injury (ALI). Chest. 2007; 132(4):572S.
28. Sud, S, et al, Effect of mechanical ventilation in the prone position on clinical outcomes in patients with acute respiratory failure. a systematic review and meta-analysis. CMAJ. 2008; 178(9):1153–1161.
![]() 29. Van der Voort, PH, Zandstra, DF, Enteral feeding in the critically ill. comparison between supine and prone positionsa prospective crossover study in mechanically ventilated patients. Crit Care. 2001; 5(4):216–220.
29. Van der Voort, PH, Zandstra, DF, Enteral feeding in the critically ill. comparison between supine and prone positionsa prospective crossover study in mechanically ventilated patients. Crit Care. 2001; 5(4):216–220.
30. Voggenreiter, G, et al, Prone positioning improves oxygenation in post traumatic lung injury. a prospective randomized trial. J Trauma 2005; 59:333–341.
![]() 31. Vollman, KM. The effect of suspended prone positioning on PaO2 and A-a gradients in adult patients with acute respiratory failure. California State University: Master’s Thesis, Long Beach; 1989.
31. Vollman, KM. The effect of suspended prone positioning on PaO2 and A-a gradients in adult patients with acute respiratory failure. California State University: Master’s Thesis, Long Beach; 1989.
![]() 32. Vollman, KM, Prone positioning in the ARDS patient. the art and science. Crit Care Nurs Clin North Am. 2004; 16(3):319–336.
32. Vollman, KM, Prone positioning in the ARDS patient. the art and science. Crit Care Nurs Clin North Am. 2004; 16(3):319–336.
![]() 33. Vollman, KM. What are the practice guidelines for prone positioning of acutely ill patients? Specifically, what are the recommendations related to hemodynamic monitoring and tube feeding? Crit Care Nurse. 2001; 21:84–86.
33. Vollman, KM. What are the practice guidelines for prone positioning of acutely ill patients? Specifically, what are the recommendations related to hemodynamic monitoring and tube feeding? Crit Care Nurse. 2001; 21:84–86.
![]() 34. Vollman, KM, Bander, JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med. 1996; 22:1105–1111.
34. Vollman, KM, Bander, JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med. 1996; 22:1105–1111.
![]() 35. West, JB, Respiratory physiology. the essentials. ed 3. Williams & Wilkins, Baltimore, 1985.
35. West, JB, Respiratory physiology. the essentials. ed 3. Williams & Wilkins, Baltimore, 1985.
![]() 36. West, JB, Dollery, CT, Naimark, A, Distribution of blood flow in isolated lung. relation to vascular and alveolar pressures. J Appl Physiol 1964; 19:713–724.
36. West, JB, Dollery, CT, Naimark, A, Distribution of blood flow in isolated lung. relation to vascular and alveolar pressures. J Appl Physiol 1964; 19:713–724.
![]() 37. Winslow, EH, et al. Effects of a lateral turn on mixed venous oxygen saturation and heart rate in critically ill adults. Heart Lung. 1990; 19:555–561.
37. Winslow, EH, et al. Effects of a lateral turn on mixed venous oxygen saturation and heart rate in critically ill adults. Heart Lung. 1990; 19:555–561.