Oxygen Saturation Monitoring with Pulse Oximetry
PREREQUISITE NURSING KNOWLEDGE
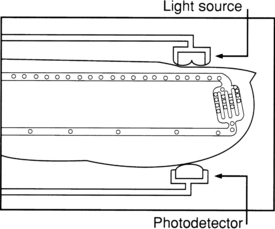
• Oxygen saturation is an indicator of the percentage of hemoglobin saturated with oxygen at the time of the measurement. The reading, obtained with standard pulse oximetry, uses a light sensor that contains two sources of light (red and infrared) absorbed by hemoglobin and transmitted through tissues to a photodetector. The infrared light is absorbed by the oxyhemoglobin, and the red light is absorbed by the reduced hemoglobin. The amount and type of light transmitted through the tissue is converted to a digital value that represents the percentage of hemoglobin saturated with oxygen (Fig. 17-1).
• Oxygen saturation values obtained with pulse oximetry (SpO2) represent one part of a complete assessment of a patient’s oxygenation status and are not a substitute for measurement of arterial saturation of oxygen (SaO2) or of ventilation (as measured with arterial partial pressure of carbon dioxide [PaCO2]).
• The accuracy of SpO2, measurements requires consideration of many physiologic variables. Patient variables include the following:
 Presence of dyshemoglobinemias (i.e., carboxyhemoglobinemia after carbon monoxide exposure)
Presence of dyshemoglobinemias (i.e., carboxyhemoglobinemia after carbon monoxide exposure)
 Arterial blood flow to the vascular bed
Arterial blood flow to the vascular bed
 Temperature of the digit or the area where the oximetry sensor is located
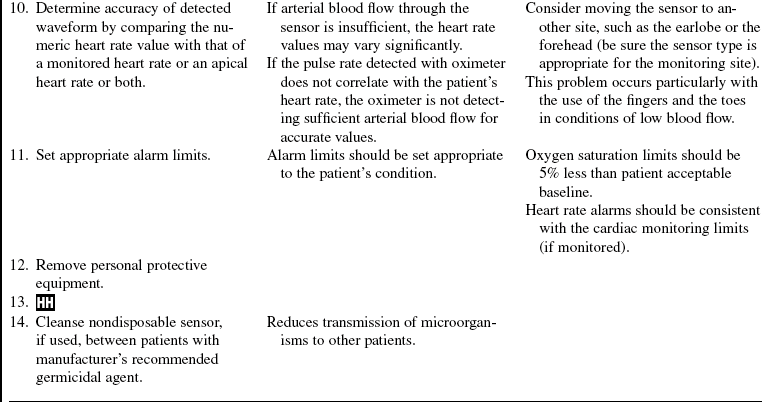
Temperature of the digit or the area where the oximetry sensor is located
 Fraction of inspired oxygen (percentage of inspired oxygen)
Fraction of inspired oxygen (percentage of inspired oxygen)
 Evidence of ventilation-perfusion mismatch
Evidence of ventilation-perfusion mismatch
• A complete assessment of oxygenation includes evaluation of oxygen content and delivery, which includes the following parameters: arterial partial pressure of oxygen (PaO2), SaO2 hemoglobin, cardiac output, and, when available, mixed venous oxygen saturation.
• Normal oxygen saturation values are approximately 97% to 99% in a healthy individual breathing room air. An oxygen saturation value of 95% is clinically accepted in a patient with a normal hemoglobin level. With a normal blood pH and body temperature, an oxygen saturation value of 90% is generally equated with a PaO2 of 60 mm Hg.
• Tissue oxygenation is not reflected by arterial or oxygen saturation obtained with pulse oximetry.
• The affinity of hemoglobin with oxygen may impair or enhance oxygen release at the tissue level.
 Oxygen is more readily released to the tissues when pH is decreased (acidosis), body temperature is increased, PaCO2, is increased, and 2,3-diphosphoglycerate levels (a by-product of glucose metabolism that facilitates the dissociation of oxygen from the hemoglobin molecule to tissue) are increased (decreased oxygen affinity).
Oxygen is more readily released to the tissues when pH is decreased (acidosis), body temperature is increased, PaCO2, is increased, and 2,3-diphosphoglycerate levels (a by-product of glucose metabolism that facilitates the dissociation of oxygen from the hemoglobin molecule to tissue) are increased (decreased oxygen affinity).
 When hemoglobin has greater affinity for oxygen, less is available to the tissues (increased oxygen affinity). Conditions such as increased pH (alkalosis), decreased temperature, decreased PaCO2, and decreased 2,3-diphosphoglycerate (as found in stored blood products) increase oxygen binding to the hemoglobin and limit its release to the tissue.
When hemoglobin has greater affinity for oxygen, less is available to the tissues (increased oxygen affinity). Conditions such as increased pH (alkalosis), decreased temperature, decreased PaCO2, and decreased 2,3-diphosphoglycerate (as found in stored blood products) increase oxygen binding to the hemoglobin and limit its release to the tissue.
• Oxygen saturation values may vary with the amount of oxygen usage or uptake by the tissues. In some patients, a difference is seen in SpO2 values at rest compared with values during activity, such as ambulation or positioning.
• Oxygen saturation does not directly reflect the patient’s ability to ventilate. The true measure of ventilation is determination of the PaCO2 in arterial blood. Use of SpO2 in a patient with obstructive pulmonary disease may result in erroneous clinical assessments of condition. As the degree of lung disease increases, the patient’s drive to breathe may shift from an increased carbon dioxide stimulus to a hypoxic stimulus. Enhancing the patient’s oxygenation and increasing the SpO2 may limit the ability to ventilate. The normal baseline SpO2 for a patient with known severe restrictive disease and more definitive methods of determination of the effectiveness of ventilation must be assessed before consideration of interventions that enhance oxygenation.
• Any discoloration of the nail bed or obstruction of the nail bed can potentially affect the transmission of light through the digit. The impact of dark nail polish, such as blue, green, brown, or black colors,4,5,11,17 has been reported to limit the transmission of light and thus impact the SpO2, although a recent study showed that fingernail polish does not cause a clinically significant change in the pulse oximeter readings in healthy individuals.15 If the nail polish cannot be removed and is believed to be affecting the accuracy of the reading, the sensor can be placed in a lateral side-to-side position on the finger to obtain readings if no other method of sampling the arterial bed is available.5,15 Bruising under the nail can limit the transmission of light and result in an artificially decreased SpO2 value. Pulse oximetry has not been shown to be affected by the presence of an elevated bilirubin.2 The presence of acrylic fingernails may impair the accuracy of the pulse oximetry reading, and removal of the nail covering may be necessary to ensure accurate measurement,9 although unpolished acrylic nails have been proven not to affect pulse oximetry readings.14
• Standard pulse oximeters use two wavelengths and are unable to differentiate between oxygen and carbon monoxide bound to hemoglobin and falsely elevated SpO2 measurements. Standard pulse oximetry equipment should never be used in suspected cases of carbon monoxide exposure. However, recent technology advancements in pulse oximetry have included the introduction of a monitor system that uses up to 12 wavelengths with a digit-based pulse oximeter sensor and that allows for measurement estimates of certain, dyshemoglobinemias (i.e., carboxyhemoglobinemia).12 An arterial blood gas always should be obtained to determine the accurate oxygen saturation and, if a CO oximeter is available, measurement of carboxyhemoglobin and methemoglobin.3
• Dark skin has been suggested to possibly affect the ability of the pulse oximeter to detect arterial pulsations. One study found more frequent differences between the SpO2 and SaO2 in black patients when compared with lighter skinned patients10; another study did not find a significant difference.13
• Certain dyes used intravenously may interfere with the accuracy of measurements, although as a result of rapid clearance, the impact is limited. Dyes include methylene blue, indigo carmine, indocyanine green, and fluorescein.8
• A pulse oximeter should not be used as a predictive indicator of the actual arterial blood gas saturation.
• A pulse oximeter should never be used during a cardiac arrest situation because of the extreme limitations of blood flow during cardiopulmonary resuscitation and the pharmacologic action of vasoactive agents administered during the resuscitation effort.
• Low perfusion states such as hypotension, vasoconstriction, hypothermia, or administration of vasoconstrictive agents limit the ability of the oximeter to distinguish the true pulsatile wave form from background noise.
• In vasoconstrictive states, oxygen saturation may be measured with a finger probe, but in patients with significant shifts in hemodynamic stability, the ear or forehead has been shown to be reasonably resistant to the vasoconstrictive effects of the sympathetic nervous system.1,16
• Forehead sensors used in patients placed in Trendelenburg’s position may require up to 20 mm Hg external pressure to achieve accurate readings, which may be accomplished with an appropriately applied headband.1
PATIENT AND FAMILY EDUCATION
• Explain the need for determination of oxygen saturation with a pulse oximeter.  Rationale: This explanation informs the patient of the purpose of monitoring, enhances patient cooperation, and decreases patient anxiety.
Rationale: This explanation informs the patient of the purpose of monitoring, enhances patient cooperation, and decreases patient anxiety.
• Explain that the values displayed may vary with patient movement, amount of environmental light, patient level of consciousness (awake or asleep), and position of the sensor.  Rationale: This explanation decreases patient and family anxiety over the constant variability of the values.
Rationale: This explanation decreases patient and family anxiety over the constant variability of the values.
• Explain that the use of pulse oximetry is part of a much larger assessment of respiratory status.  Rationale: This explanation prepares the patient and family for other possible diagnostic tests of oxygenation (e.g., arterial blood gas).
Rationale: This explanation prepares the patient and family for other possible diagnostic tests of oxygenation (e.g., arterial blood gas).
• Explain the equipment to the patient.  Rationale: This information facilitates patient cooperation in maintaining sensor placement.
Rationale: This information facilitates patient cooperation in maintaining sensor placement.
• Explain the need for an audible alarm system for alerting clinicians of oxygen saturation values below a set acceptable limit, as determined by the clinician. Demonstrate the alarm system, alerting the patient and family to the possibility of alarms, including causes of false alarms.  Rationale: Provision of an understanding of the use of an alarm system and its importance in the overall management of the patient’s condition and of circumstances in which a false alarm may occur assists in understanding of the SpO2 values seen at the bedside.
Rationale: Provision of an understanding of the use of an alarm system and its importance in the overall management of the patient’s condition and of circumstances in which a false alarm may occur assists in understanding of the SpO2 values seen at the bedside.
• Explain the need to move or remove the sensor on a routine basis to prevent complications related to the type of sensor used and monitoring site (i.e., digit, forehead, ear).  Rationale: An understanding of the need to move the sensor routinely assists in patient understanding of the frequency of sensor movement.
Rationale: An understanding of the need to move the sensor routinely assists in patient understanding of the frequency of sensor movement.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Signs and symptoms of decreased oxygenation include the following:
•  Rationale: Patient assessment determines the need for continuous pulse oximetry monitoring. Anticipation of conditions in which hypoxia could be present allows earlier intervention before unfavorable outcomes occur.
Rationale: Patient assessment determines the need for continuous pulse oximetry monitoring. Anticipation of conditions in which hypoxia could be present allows earlier intervention before unfavorable outcomes occur.
• Assess the extremity (digit) or area where the sensor will be placed including the following:
 Exposure to excessive environmental light sources (e.g., examination lights)
Exposure to excessive environmental light sources (e.g., examination lights)
 Excessive movement or tremor in the digit
Excessive movement or tremor in the digit
•  Rationale: Assessment of factors that may inhibit accuracy of the measurement of oxygenation before attempting to obtain the SpO2 reading enhances the validity of the measurement and allows for correction of factors as possible.
Rationale: Assessment of factors that may inhibit accuracy of the measurement of oxygenation before attempting to obtain the SpO2 reading enhances the validity of the measurement and allows for correction of factors as possible.
Patient Preparation
• Verify the correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
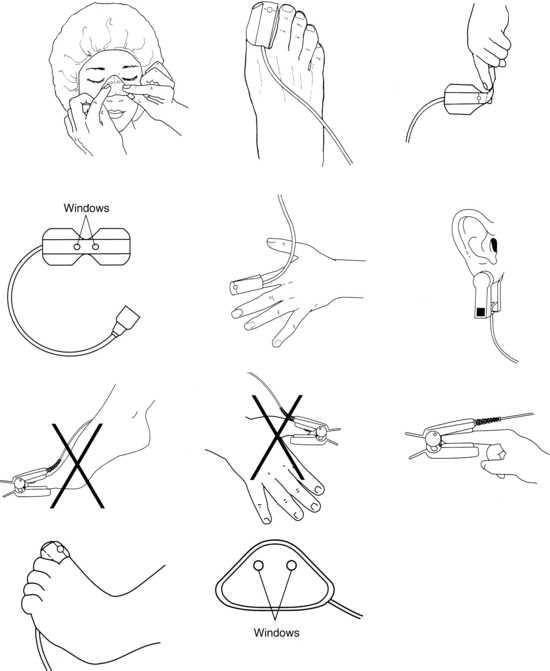
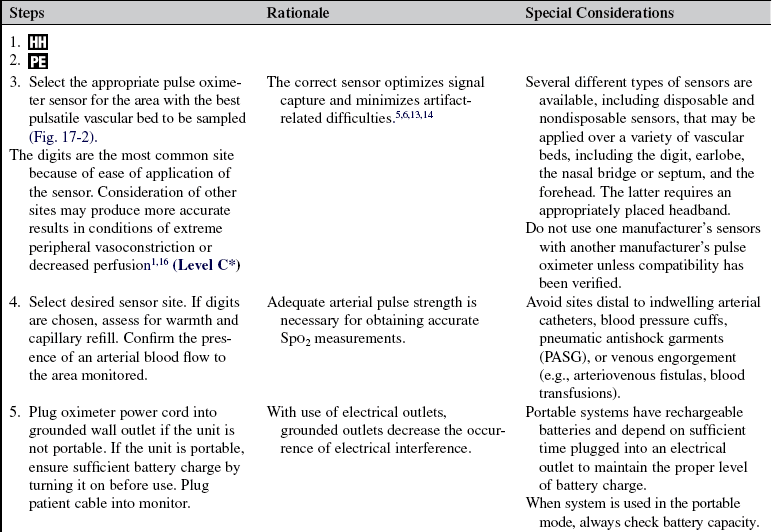
Figure 17-2 Sensor types and sensor sites for pulse oximetry monitoring. Use “wrap” or “clip” style sensors on the fingers (including thumb), great toe, and nose. The windows for the light source and photodetector must be placed directly opposite each other on each side of the arteriolar bed to ensure accuracy of SpO2 measurements. Choice of the correct size of the sensor helps decrease the incidence of excess ambient light interference and optical shunting. “Clip” style sensors are appropriate for fingers (except the thumb) and the earlobe. Ensuring that the arteriolar bed is well within the clip with the windows directly opposite each other decreases the possibility of excess ambient light interference and optical shunting. (Reprinted by permission of Nellcor Puritan Bennett LLC, Boulder, CO, part of Covidien.)
References
1. Agashe, GS, Coakley, J, Mannheimer, PD. Forehead pulse oximetry. Anesthesiology. 2006; 105:1111–1115.
![]() 2. Awad, AA, et al. Different responses of ear and finger pulse oximeter wave form to cold pressor test. Anesth Analg. 2001; 92:1483–1486.
2. Awad, AA, et al. Different responses of ear and finger pulse oximeter wave form to cold pressor test. Anesth Analg. 2001; 92:1483–1486.
3. Barker, SJ, et al, Measurement of carboxyhemoglobin and methemoglobin by pulse oximetry . Anesthesiology . 2006; 105:892–897.
![]() 4. Chan, MM. What is the effect of fingernail polish on pulse oximetry. Chest. 2003; 123:2163–2164.
4. Chan, MM. What is the effect of fingernail polish on pulse oximetry. Chest. 2003; 123:2163–2164.
![]() 5. Grap, MJ. Pulse oximetry. Crit Care Nurse. 1998; 18:94–99.
5. Grap, MJ. Pulse oximetry. Crit Care Nurse. 1998; 18:94–99.
6. Grap, MJ, Pulse oximetry. AACN protocols for practice . technology series. American Association of Critical-Care Nurses: Aliso Viejo, CA, 2005.
![]() 7. Hanowell, L, Eisele, JH, Downs, D. Ambient light affects pulse oximeters. Anesthesiology. 1987; 67:864–865.
7. Hanowell, L, Eisele, JH, Downs, D. Ambient light affects pulse oximeters. Anesthesiology. 1987; 67:864–865.
![]() 8. Hedges, J, Baker, WE, Lanoix, R, et al, Pulse oximetry. Roberts . clinical procedures in emergency medicine. ed 4. PA Saunders, Philadelphia, 2004:32–36.
8. Hedges, J, Baker, WE, Lanoix, R, et al, Pulse oximetry. Roberts . clinical procedures in emergency medicine. ed 4. PA Saunders, Philadelphia, 2004:32–36.
9. Hinkelbein, J, Koehler, H, Genzwuerker, HV, et al, Artificial acrylic finger nails may alter pulse oximetry measurement . Resuscitation 2006; 74:75–82.
![]() 10. Jubran, A. Reliability of pulse oximetry in titrating supplemental oxygen therapy in ventilator-dependent patients. Chest,. 1990; 97:1420–1425.
10. Jubran, A. Reliability of pulse oximetry in titrating supplemental oxygen therapy in ventilator-dependent patients. Chest,. 1990; 97:1420–1425.
![]() 11. Kelleher, JF. Pulse oximetry. J Clin Monit. 1989; 5:37–62.
11. Kelleher, JF. Pulse oximetry. J Clin Monit. 1989; 5:37–62.
12. Masimo, Rainbow SET Pulse CO-Oximetery. http://www.masimo.com/Rainbow/about.htm., 2008 [retrieved March 21, 2009, from].
![]() 13. McConnell, EA, Performing pulse oximetry . Nursing 1999; 99:11–17.
13. McConnell, EA, Performing pulse oximetry . Nursing 1999; 99:11–17.
![]() 14. Peters, SM. The effect of acrylic nails on the measurement of oxygen saturation as determined by pulse oximetry. AANAJ. 1997; 65:361–363.
14. Peters, SM. The effect of acrylic nails on the measurement of oxygen saturation as determined by pulse oximetry. AANAJ. 1997; 65:361–363.
15. Rodden, AM, Spicer, L, Diaz, VA, et al. Does fingernail polish affect pulse oximeter readings. Intensive Crit Care Nurs. 2007; 23:51–55.
16. Schallom, L. Comparison of forehead and digit oximetry in surgical/trauma patients at risk of decreased peripheral perfusion. Heart Lung. 2007; 36:188–194.
![]() 17. Szarlarski, NL, Cohen, NH. Use of pulse oximetry in critically ill adults. Heart Lung. 1989; 18:444–453.
17. Szarlarski, NL, Cohen, NH. Use of pulse oximetry in critically ill adults. Heart Lung. 1989; 18:444–453.
18. Zablocki, AD, Rasch, DK, A simple method to prevent interference with pulse oximetry by infrared heating . Anesth Analg . 1987; 66:915.
Bianchi, J, et al, Pulse oximetry index. a simple arterial assessment for patients with venous disease. J Wound Care 2008; 17:253–260.
Clark, AP, Legal lessons. “But his O2 sat was normal. Clin Nurse Specialist 2002; 16:162–163.
Giuliano, KK, et al. New-generation pulse oximetry in the care of critically ill patients. Am J Crit Care. 2005; 14:26–39.
Witting, MD, Scharf, SM, Diagnostic room-air pulse oximetry. effects of smoking, race, and sex. Am J Emerg Med 2008; 26:131–136.