Procedure 17 Anterior Thoracolumbar Spinal Fusion via Open Approach for Idiopathic Scoliosis
Indications
 To halt progression of spinal curvature
To halt progression of spinal curvature
 To restore spinal alignment and balance
To restore spinal alignment and balance
 To preserve caudal motion segments (typically one to two segments) when compared with posterior spinal fusion (PSF)
To preserve caudal motion segments (typically one to two segments) when compared with posterior spinal fusion (PSF)
 To prevent the crankshaft phenomenon in skeletally immature patients (Risser 0, open triradiate cartilage)
To prevent the crankshaft phenomenon in skeletally immature patients (Risser 0, open triradiate cartilage)
 To allow for a thoracoscopic approach in selected cases
To allow for a thoracoscopic approach in selected cases
 Appropriate candidates typically include Lenke type 1 (single structural thoracic) and Lenke type 5 (single structural thoracolumbar/lumbar) curves (Figure 17-1, A and B).
Appropriate candidates typically include Lenke type 1 (single structural thoracic) and Lenke type 5 (single structural thoracolumbar/lumbar) curves (Figure 17-1, A and B).
Indications Pitfalls
• Anterior surgery tends to be “kyphogenic.” This may not be appropriate in curves with thoracic kyphosis greater than 40 degrees or in cases of thoracolumbar (“junctional”) kyphosis or lumbar hypolordosis.
• Patients weighing greater than 60 kg, with curves greater than 75 degrees, with or without hyperkyphosis, are not candidates for single-rod thoracic open or thoracoscopic fusion.
Examination/Imaging
 Clinical assessment of curve location, coronal and sagittal balance, trunk rotation, shoulder asymmetry, pelvic obliquity, integrity of the neuraxis, and any other associated anomalies
Clinical assessment of curve location, coronal and sagittal balance, trunk rotation, shoulder asymmetry, pelvic obliquity, integrity of the neuraxis, and any other associated anomalies
 Full-length standing posteroanterior, lateral, and right and left supine bending radiographs to assist in curve classification, assessment of curve flexibility, and selection of fusion levels
Full-length standing posteroanterior, lateral, and right and left supine bending radiographs to assist in curve classification, assessment of curve flexibility, and selection of fusion levels
 Magnetic resonance imaging in selected cases (e.g., neurologic signs or symptoms, early- or juvenile-onset scoliosis, rapid curve progression, unusual curve pattern)
Magnetic resonance imaging in selected cases (e.g., neurologic signs or symptoms, early- or juvenile-onset scoliosis, rapid curve progression, unusual curve pattern)
Positioning
 The surgical approach is always from the convex side of the curvature in the lateral decubitus position.
The surgical approach is always from the convex side of the curvature in the lateral decubitus position.
Positioning Pearls
• Copious padding of all bony and soft tissue prominences, such as the axilla (“axillary roll”) and lateral knee, is required to prevent a compressive neuropathy or pressure necrosis of the upper or lower extremity or trunk.
• Electrophysiologic monitoring of the upper extremities will allow early detection of compressive neuropathies, prompting immediate repositioning and/or repadding of the upper extremity.
• A flat radiolucent table and beanbag positioner are utilized.
• When utilized, unobstructed fluoroscopic access is verified before preparation and draping.
• Neurophysiologic monitoring of spinal cord function, using both somatosensory evoked potential and transcranial motor evoked potential monitoring, is recommended to optimize patient safety.
Portals/Exposures
Thoracolumbar
Lumbar
Portals/Exposures Pearls
Procedure: Thoracolumbar Spine Fusion via an Open Approach Using Single-Rod Instrumentation
Step 1: Anterior Release and Diskectomy
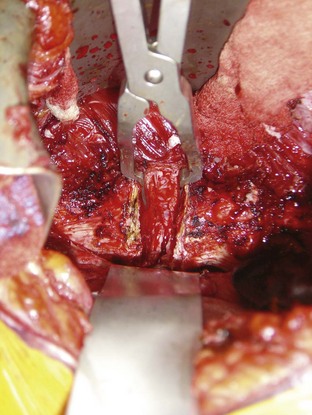
 Once adequate spinal exposure has been obtained, transection of the anterior longitudinal ligament and complete diskectomy is performed to, or including, the posterior longitudinal ligament.
Once adequate spinal exposure has been obtained, transection of the anterior longitudinal ligament and complete diskectomy is performed to, or including, the posterior longitudinal ligament.
Step 1 Pearls
• Release of the anterior longitudinal ligament and complete diskectomy allows for maximal curve flexibility and deformity correction.
• A malleable ribbon retractor placed around to the far side of the disk space affords protection to the vascular structures.
• For severe, rigid curvatures that have developed wedging of the vertebral bodies, vertebral osteotomy may be required to gain maximum correction.
Step 2: Placement of the Anterior Vertebral Body Screws
 The entry point of the vertebral body screw is preferentially the junction of the pedicular origin and the vertebral body, crossing the center of the vertebral body and directed perpendicularly across to the far side. At the cephalad and caudad end vertebrae a staple can be impacted to prevent pullout or plow-through of the screws. At intervening levels, a washer can be placed to help distribute load.
The entry point of the vertebral body screw is preferentially the junction of the pedicular origin and the vertebral body, crossing the center of the vertebral body and directed perpendicularly across to the far side. At the cephalad and caudad end vertebrae a staple can be impacted to prevent pullout or plow-through of the screws. At intervening levels, a washer can be placed to help distribute load.
 The entry hole is made first with a sharp awl. A straight pedicle probe is then directed toward the surgeon’s finger on the far side of the body. The desired screw length is then measured. A tap is then placed, followed by screw placement. Image guidance is optional, but can assure screw placement central in the body and parallel to the vertebral end plates.
The entry hole is made first with a sharp awl. A straight pedicle probe is then directed toward the surgeon’s finger on the far side of the body. The desired screw length is then measured. A tap is then placed, followed by screw placement. Image guidance is optional, but can assure screw placement central in the body and parallel to the vertebral end plates.
Step 3: End-Plate Ablation
Step 4: Placement of Anterior Interbody Structural Supports
 Anterior interbody structural supports are important for overall strength of the construct and for setting the desired lordosis in the lumbar spine. When using single-rod instrumentation, a structural support is placed at each level in the lumbar spine, starting from the apex and moving cephalad and caudad. The graft should be impacted toward the concave side and positioned to lie flush with the anterior aspect of the vertebral body when setting the lordosis. Upon placement of the structural grafts, the spinal curvature is usually fully corrected and the lumbar lordosis is “set” before rod placement.
Anterior interbody structural supports are important for overall strength of the construct and for setting the desired lordosis in the lumbar spine. When using single-rod instrumentation, a structural support is placed at each level in the lumbar spine, starting from the apex and moving cephalad and caudad. The graft should be impacted toward the concave side and positioned to lie flush with the anterior aspect of the vertebral body when setting the lordosis. Upon placement of the structural grafts, the spinal curvature is usually fully corrected and the lumbar lordosis is “set” before rod placement.
 In the case of single structural thoracic (Lenke 1) curves fused to the thoracolumbar junction (T12 or L1), structural grafts are used one or two levels above the last instrumented vertebra to prevent junctional kyphosis.
In the case of single structural thoracic (Lenke 1) curves fused to the thoracolumbar junction (T12 or L1), structural grafts are used one or two levels above the last instrumented vertebra to prevent junctional kyphosis.
Step 5: Rod Placement
 The rod is appropriately contoured to the desired sagittal and coronal plane configuration and introduced into the screws. The rod is reduced to the screws and captured sequentially.
The rod is appropriately contoured to the desired sagittal and coronal plane configuration and introduced into the screws. The rod is reduced to the screws and captured sequentially.
 Some degree of rod rotation or screw rotation may be necessary to “fine-tune” the correction. This should not require much force at this stage.
Some degree of rod rotation or screw rotation may be necessary to “fine-tune” the correction. This should not require much force at this stage.
 Some final compression of the screws across the disk spaces to firmly compress the grafts can be performed at this stage if necessary.
Some final compression of the screws across the disk spaces to firmly compress the grafts can be performed at this stage if necessary.
Step 6: Placement of Chest Tube and Wound Closure
 A standard chest tube is placed and withdrawn from a small separate stab incision.
A standard chest tube is placed and withdrawn from a small separate stab incision.
 Wound closure must allow for meticulous reapproximation of the diaphragm (see Portals/Exposures Pearls).
Wound closure must allow for meticulous reapproximation of the diaphragm (see Portals/Exposures Pearls).
 The chest tube is maintained on wall suction until the first or second postoperative day. It is removed upon resolution of the pneumothorax/hemothorax and when output decreases to less than 75 to 100 mL over a 12-hour period.
The chest tube is maintained on wall suction until the first or second postoperative day. It is removed upon resolution of the pneumothorax/hemothorax and when output decreases to less than 75 to 100 mL over a 12-hour period.
Procedure: Thoracolumbar Spine Fusion via an Open Approach Using Dual-Rod Instrumentation
Step 2: Placement of the Anterior Vertebral Body Screws
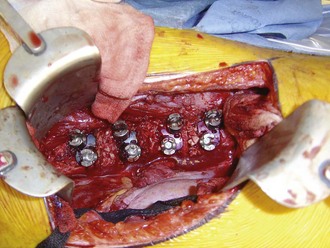
 With systems using a dual-rod construct, there is typically a two-holed tined vertebral staple that is implanted first, which then receives the vertebral body screws (Figure 17-4). When positioning these devices, care should be taken not to allow the anterior screw to be too close to the anterior aspect of the vertebral body, because vertebral body fracture can occur. The proper staple is selected by identifying the size that maximizes the coverage of the lateral aspect of the vertebral body without violating the adjacent disk space.
With systems using a dual-rod construct, there is typically a two-holed tined vertebral staple that is implanted first, which then receives the vertebral body screws (Figure 17-4). When positioning these devices, care should be taken not to allow the anterior screw to be too close to the anterior aspect of the vertebral body, because vertebral body fracture can occur. The proper staple is selected by identifying the size that maximizes the coverage of the lateral aspect of the vertebral body without violating the adjacent disk space.
 Anteriorly placed devices may also incur more kyphosis, which is undesirable in the lumbar spine. The posterior screw should be placed in a position as posterior as possible, without allowing for canal intrusion.
Anteriorly placed devices may also incur more kyphosis, which is undesirable in the lumbar spine. The posterior screw should be placed in a position as posterior as possible, without allowing for canal intrusion.
Step 5: Rod Placement
 The rods are appropriately contoured to the desired sagittal and coronal plane configuration.
The rods are appropriately contoured to the desired sagittal and coronal plane configuration.
 The posteriormost rod is reduced to the screws first and captured sequentially.
The posteriormost rod is reduced to the screws first and captured sequentially.
 Some degree of rod rotation may be necessary to “fine tune” the correction, which has already largely occurred from the meticulous diskectomy and structural graft placement.
Some degree of rod rotation may be necessary to “fine tune” the correction, which has already largely occurred from the meticulous diskectomy and structural graft placement.
 The anterior screws can be used to further derotate the vertebrae at this point, if necessary. Some final compression of the posterior screws across the disk spaces to firmly compress the grafts before final tightening can be performed at this stage. The anteriormost rod is then placed and captured at this point, essentially in situ.
The anterior screws can be used to further derotate the vertebrae at this point, if necessary. Some final compression of the posterior screws across the disk spaces to firmly compress the grafts before final tightening can be performed at this stage. The anteriormost rod is then placed and captured at this point, essentially in situ.
 Some spinal implant systems will use a cross connector, which can be placed at this point (Figure 17-5).
Some spinal implant systems will use a cross connector, which can be placed at this point (Figure 17-5).
Postoperative Care and Expected Outcomes
 The patient is mobilized beginning on the day following surgery. If single-rod instrumentation is utilized, a spinal orthosis is fashioned and worn for 3 to 4 months postoperatively. If dual-rod instrumentation is utilized, no brace is employed.
The patient is mobilized beginning on the day following surgery. If single-rod instrumentation is utilized, a spinal orthosis is fashioned and worn for 3 to 4 months postoperatively. If dual-rod instrumentation is utilized, no brace is employed.
 Activity modifications are necessary for at least the first 6 months postoperatively, with a return to competitive sports at 12 months or when clear evidence of fusion is seen radiographically.
Activity modifications are necessary for at least the first 6 months postoperatively, with a return to competitive sports at 12 months or when clear evidence of fusion is seen radiographically.
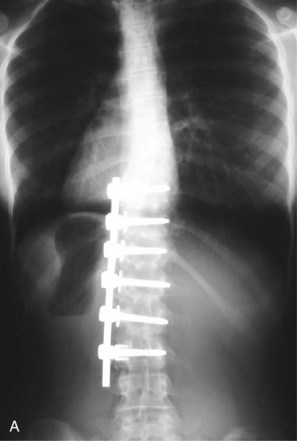
 Radiographs are taken to assess the implant stability, maintenance of correction and maturation of the fusion at 1, 3, 6, and 12 months postoperatively (Figures 17-6, A and B, and 17-7). Yearly radiographs are obtained thereafter until definitive fusion is seen.
Radiographs are taken to assess the implant stability, maintenance of correction and maturation of the fusion at 1, 3, 6, and 12 months postoperatively (Figures 17-6, A and B, and 17-7). Yearly radiographs are obtained thereafter until definitive fusion is seen.
Fricka KB, Mahar AT, Newton PO. Biomechanical analysis of anterior scoliosis instrumentation: differences between single and dual rod systems with and without structural interbody support. Spine. 2002;27:702-706.
Lowe TG, Alongi PR, Smith DA, et al. Anterior single-rod instrumentation for thoracolumbar adolescent idiopathic scoliosis with and without the use of structural interbody support. Spine. 2003;28:2221-2232.
Lowe TG, Enguidanos ST, Smith DA, et al. Single-rod versus dual-rod anterior instrumentation for idiopathic scoliosis: a biomechanical study. Spine. 2005;30:311-317.
Polly DWJr, Cunningham BW, Kuklo TR, et al. Anterior thoracic scoliosis constructs: effect of rod diameter and intervertebral cages on multi-segmental construct stability. Spine J. 2003;3:213-219.
Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke type I adolescent idiopathic scoliosis curves. Spine. 2005;30:1859-1866.
Rhee JM, Bridwell KH, Won DS, et al. Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine. 2002;27:2350-2356.
Smith JA, Deviren V, Berven S, Bradford DS. Does instrumented anterior scoliosis surgery lead to kyphosis, pseudarthrosis or inadequate correction in adults? Spine. 2002;27:529-534.