Continuous Venous Oxygen Saturation Monitoring
PREREQUISITE NURSING KNOWLEDGE
• Anatomy and physiology of the cardiopulmonary system should be understood.
• Physiologic principles related to invasive hemodynamic monitoring should be understood.
• Technical aspects of central line placement and pressure monitoring should be understood.
• Technical aspects of pulmonary artery (PA) pressure monitoring should be understood.
• Physiologic concepts of oxygen delivery, oxygen demand, and tissue oxygen consumption should be understood.
• The percent of venous oxygen saturation as measured in the PA (SVO2) is flow weighted and represents a true mixing of all venous blood: inferior vena cava (IVC), superior vena cava (SVC), and coronary sinus.
• Clinically, SVO2 provides an index of overall oxygen balance because it is a reflection of the dynamic relationship between the patient’s oxygen delivery (DO2) and oxygen consumption (VO2). Whenever a threat to the oxygen balance occurs, the body’s primary compensatory mechanisms are to increase oxygen delivery by increasing cardiac output or to increase oxygen extraction at the tissue level.
• In a critically ill patient, if cardiac output is limited, increased extraction occurs to meet the demand for oxygen at the tissue level. The result is a decreased level of oxygen returning to the heart and a lower SVO2 measurement. Many factors can affect the requirements for oxygen and subsequently SVO2 (Table 16-1).2,6,8,13
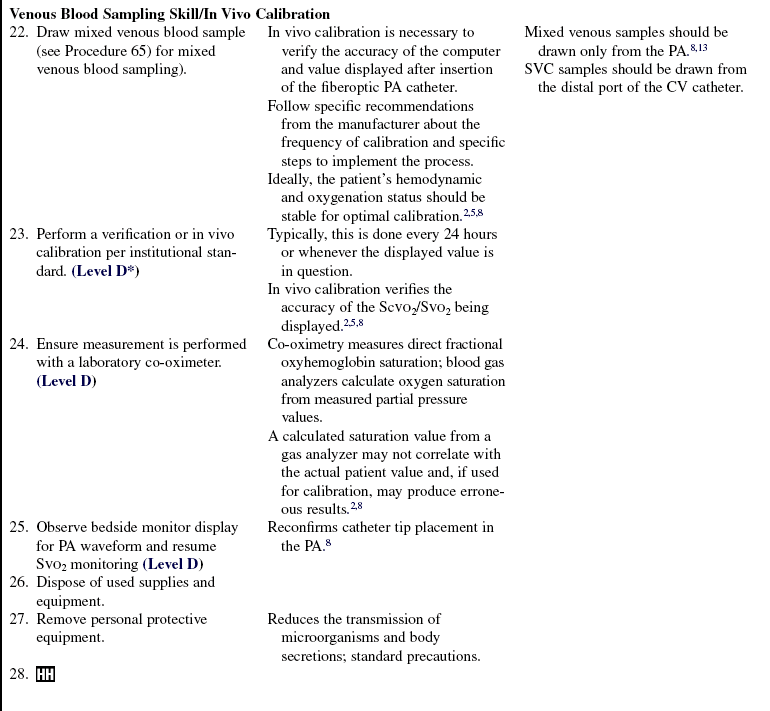
Table 16-1
Common Conditions and Activities That Affect Venous Oxygen Saturation Values
Decreased Central and Mixed Venous Oxygen Saturation
Decreased Oxygen Delivery
Decreased cardiac output
Decreased hemoglobin
Decreased arterial oxygen saturation
Decreased arterial partial pressure of oxygen
Increased Oxygen Consumption
Fever
Pain
Shivering
Seizures
Increased work of breathing
Agitation
Infection and sepsis
Vasoactive and beta-agonist medications
Multiple organ failure
Burns
Head injury
Increased musculoskeletal activities
Numerous nursing procedures (e.g., dressing changes, suctioning, turning, and chest physiotherapy)
Increased Central and Mixed Venous Oxygen Saturation
Increased Oxygen Delivery
Increased cardiac output
Increased hemoglobin
Increased arterial oxygen saturation
Increased arterial partial pressure of oxygen
Decreased Oxygen Consumption
Hypothermia
Hypothyroidism
Pharmacologic paralysis and sedation
Anesthesia
Cellular dysfunction
Decreased work of breathing
Decreased musculoskeletal activities
• SVO2 does not correlate directly with any of the determinants of oxygen delivery or oxygen consumption. Because a critically ill patient is in a dynamic state with rapidly changing oxygen demand and oxygen consumption, SVO2 must be viewed in the light of these changing determinants and considered an index of oxygen balance.1,2,6,8,13
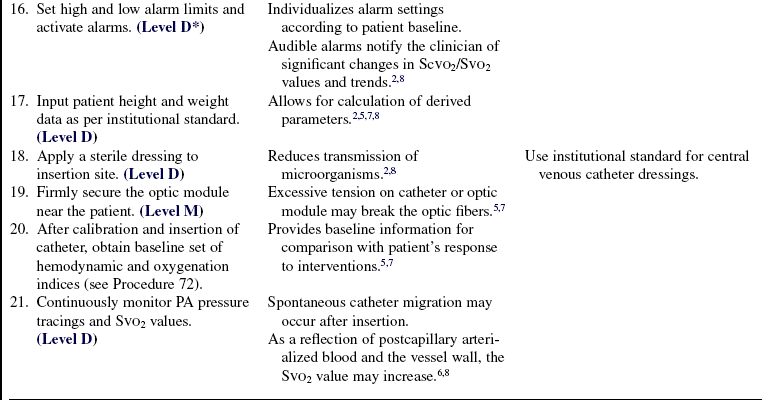
• A normal SVO2 generally is considered to be 60% to 80%,2,8 and a clinically significant change in SVO2 (5% to 10%) can be an early indicator of physiologic instability.2,8 SVO2 values of less than 60% may result from either inadequate oxygen delivery or excess oxygen consumption. SVO2 monitoring is used in critically ill patients for earlier detection of oxygenation instability than that obtained through traditional PA monitoring.2,6,8,13
• The percent of venous oxygen saturation as measured in the superior vena cava (ScVO2) reflects the mixing of venous blood from the superior half of the body. It does not include blood from the IVC and coronary sinus. ScVO2, right atrium (RA), and SVO2 do not correlate absolutely. ScVO2 does trend with SVO2 in a variety of hemodynamic states. In normal conditions, ScVO2 is slightly less than the RA oxygen saturation and lower than SVO2. In septic or shock states, ScVO2 is higher than SVO2, with a difference that ranges from 5% to 7% and up to 18% in severe shock. This difference is in part because of a redistribution of blood flow caused by the various pathophysiologies. Therefore, ScVO2 overestimates SVO2 in shock conditions; a low ScVO2 likely indicates an even lower SVO2.4,9–11
• Small French size and shorter oximetry catheters have pediatric patient applications for assessment of venous saturation.9
• Some common proper setup and maintenance steps for the catheters and bedside computer or module are necessary for accurate monitoring of both ScVO2 and SVO2.
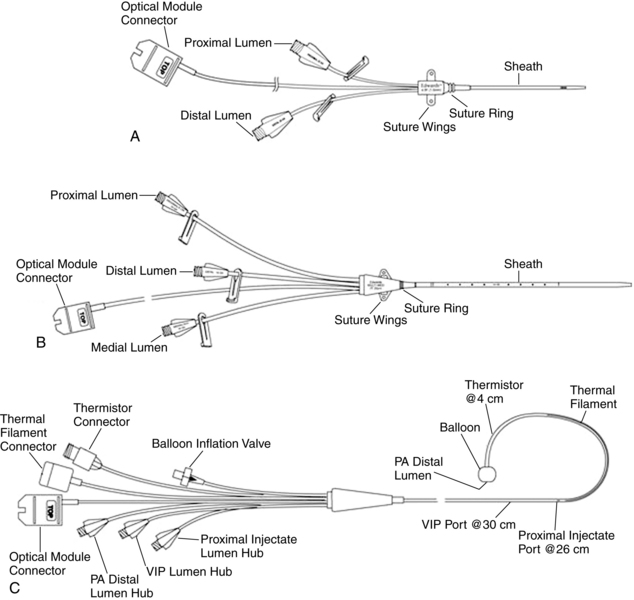
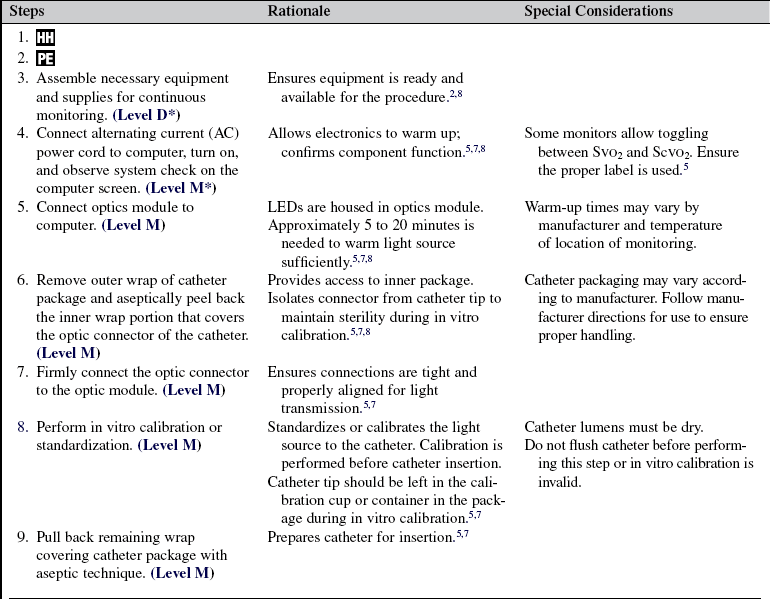
• Continuous venous saturation monitoring is performed with a three-component system (Fig. 16-1)2,5–7:
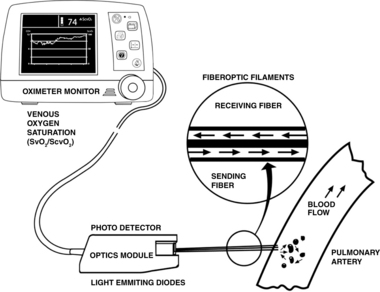
Figure 16-1 Oximetry system with reflectance spectrophotometry. (From Edwards Lifesciences LLC: Understanding mixed venous oxygen saturation [SVO2] monitoring using the Swan Ganz TD System, ed 2, Irvine, CA, 2002, Edwards Lifesciences.)
 A fiberoptic central venous (CV) or PA catheter contains two fiberoptic filaments that exit at the distal lumen. One filament serves as a sending fiber for the emission of light; the other serves as a receiving fiber for the light reflected back from the blood in the vessel (Fig. 16-2).
A fiberoptic central venous (CV) or PA catheter contains two fiberoptic filaments that exit at the distal lumen. One filament serves as a sending fiber for the emission of light; the other serves as a receiving fiber for the light reflected back from the blood in the vessel (Fig. 16-2).
 The optic module houses the light-emitting diodes (LEDs), which transmit various wavelengths of light, and a photodetector, which receives light back. The light wavelengths are shone through a blood sample. Desaturated hemoglobins, saturated hemoglobins (oxyhemoglobin), and dyshemoglobins (carboxyhemoglobin, methemoglobin) have different light absorption characteristics. The ratio of hemoglobin to oxyhemoglobin is determined and reported as a percentage value.2,5,7 All previous patient data, including calibration of saturation values and patient identification information, are stored in this component. This module should not be disconnected. If the module must be disconnected, refer to the manufacturer’s instructions for a disconnection procedure that does not result in memory loss.
The optic module houses the light-emitting diodes (LEDs), which transmit various wavelengths of light, and a photodetector, which receives light back. The light wavelengths are shone through a blood sample. Desaturated hemoglobins, saturated hemoglobins (oxyhemoglobin), and dyshemoglobins (carboxyhemoglobin, methemoglobin) have different light absorption characteristics. The ratio of hemoglobin to oxyhemoglobin is determined and reported as a percentage value.2,5,7 All previous patient data, including calibration of saturation values and patient identification information, are stored in this component. This module should not be disconnected. If the module must be disconnected, refer to the manufacturer’s instructions for a disconnection procedure that does not result in memory loss.
 An oximeter computer, which can be a stand-alone unit or a module for a bedside monitoring system, has a microprocessor that converts the light information from the optic module into an electrical display, updated every few seconds for continuous monitoring. This information is displayed as a continuous graphic trend, a numeric display, or both, depending on the manufacturer.
An oximeter computer, which can be a stand-alone unit or a module for a bedside monitoring system, has a microprocessor that converts the light information from the optic module into an electrical display, updated every few seconds for continuous monitoring. This information is displayed as a continuous graphic trend, a numeric display, or both, depending on the manufacturer.
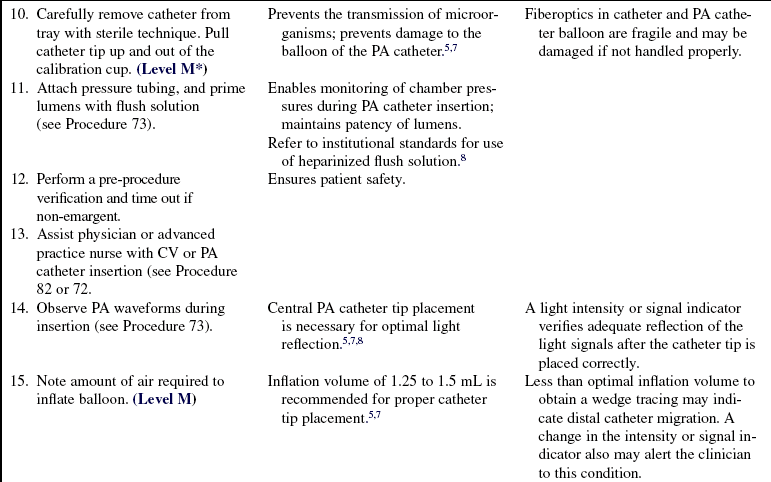
 Proper calibration of the monitor and catheter ensures accuracy of venous saturation values. The two types of calibration are in vitro, in which the catheter and optics module are calibrated before insertion; and in vivo, where the venous saturation value is compared with a laboratory co-oximeter value from a blood sample. Follow manufacturer recommendations for performing calibration procedures. Daily in vivo calibrations are recommended. In addition, proper blood sampling techniques from the distal port of the PA catheter are necessary for ensuring accurate values for calibration.2,5,7,8
Proper calibration of the monitor and catheter ensures accuracy of venous saturation values. The two types of calibration are in vitro, in which the catheter and optics module are calibrated before insertion; and in vivo, where the venous saturation value is compared with a laboratory co-oximeter value from a blood sample. Follow manufacturer recommendations for performing calibration procedures. Daily in vivo calibrations are recommended. In addition, proper blood sampling techniques from the distal port of the PA catheter are necessary for ensuring accurate values for calibration.2,5,7,8
EQUIPMENT
• Fiberoptic PA catheter for SVO2 (various sizes, 4 Fr to 8 Fr; various lumens, 2 Fr to 7 Fr; various lengths, 25 to 110 cm)
• Fiberoptic CV catheter for ScVO2 (various sizes for pediatric to adult use, 4.5 Fr to 8.5 Fr; various lengths, 5 to 20 cm; single, double, or triple lumen)
• Oximeter computer or bedside monitoring system module
• Equipment required for CV monitoring (see Procedure 70) or PA catheterization and pressure monitoring (see Procedure 73)
Additional equipment (to have available depending on patient need) includes the following:
PATIENT AND FAMILY EDUCATION
• Assess patient and family understanding of the clinical benefits of venous oximetry monitoring.  Rationale: For information to be the most appropriate, assessment of the level of patient and family understanding of need for ScVO2 or SVO2 monitoring is important.
Rationale: For information to be the most appropriate, assessment of the level of patient and family understanding of need for ScVO2 or SVO2 monitoring is important.
• Explain the continuous nature of this monitoring system and the significance of the alarms.  Rationale: Explanation of the procedure to the patient and family helps to alleviate fears and concerns. Additional monitors may produce increased anxiety in the patient and family.
Rationale: Explanation of the procedure to the patient and family helps to alleviate fears and concerns. Additional monitors may produce increased anxiety in the patient and family.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Indications for use of ScVO2/SVO2 monitoring include the following1–3,5–13:
 High-risk cardiovascular surgery
High-risk cardiovascular surgery
 Acute respiratory distress syndrome
Acute respiratory distress syndrome
 Use of positive end-expiratory pressure (PEEP)
Use of positive end-expiratory pressure (PEEP)
 As a component of early goal-directed therapy for severe sepsis and septic shock
As a component of early goal-directed therapy for severe sepsis and septic shock  Rationale: ScVO2/SVO2 monitoring is useful in the early detection of oxygenation imbalance, which can facilitate the use of early and more appropriate interventions.
Rationale: ScVO2/SVO2 monitoring is useful in the early detection of oxygenation imbalance, which can facilitate the use of early and more appropriate interventions.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Answer patient questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
References
![]() 1. Bishop, MH, et al, Prospective, randomized trial of survivor values of cardiac index, oxygen delivery, and oxygen consumption as resuscitation endpoints in severe trauma . J Trauma 1995; 38:780–787.
1. Bishop, MH, et al, Prospective, randomized trial of survivor values of cardiac index, oxygen delivery, and oxygen consumption as resuscitation endpoints in severe trauma . J Trauma 1995; 38:780–787.
![]() 2. Darovic, GO. Handbook hemodynamic monitoring, ed 2. St Louis: Saunders; 2004.
2. Darovic, GO. Handbook hemodynamic monitoring, ed 2. St Louis: Saunders; 2004.
3. Dellinger, RP, Levy, MM, Carlet, JM, et al, Surviving sepsis campaign . international guidelines for the management of severe sepsis and septic shock. Crit Care Med 2008; 36:296–327.
![]() 4. Edwards, JD, Mayall, RM. Importance of the sampling site for measurement of mixed venous oxygen saturation in shock. Crit Care Med. 1998; 26:1356–1360.
4. Edwards, JD, Mayall, RM. Importance of the sampling site for measurement of mixed venous oxygen saturation in shock. Crit Care Med. 1998; 26:1356–1360.
![]() 5. Edwards Lifesciences LLC, Vigilance. continuous cardiac output and Svo2 monitoring system. Operations manual. Edwards Lifesciences: Irvine, CA, 2003.
5. Edwards Lifesciences LLC, Vigilance. continuous cardiac output and Svo2 monitoring system. Operations manual. Edwards Lifesciences: Irvine, CA, 2003.
![]() 6. Headley, JM. Strategies to optimize the cardiorespiratory status of the critically ill. AACN Clin Issues Crit Care Nurs. 1995; 6:121–134.
6. Headley, JM. Strategies to optimize the cardiorespiratory status of the critically ill. AACN Clin Issues Crit Care Nurs. 1995; 6:121–134.
![]() 7. Hospira, Inc. Q2Plus SO2/CO computer (system operating manual. North Chicago: Hospira; 2004.
7. Hospira, Inc. Q2Plus SO2/CO computer (system operating manual. North Chicago: Hospira; 2004.
![]() 8. Jesurum, JT, Svo2 monitoring. AACN protocols for practice . hemodynamic monitoring. American Association of Critical-Care Nurses: Aliso Viejo, CA, 1998.
8. Jesurum, JT, Svo2 monitoring. AACN protocols for practice . hemodynamic monitoring. American Association of Critical-Care Nurses: Aliso Viejo, CA, 1998.
9. Liakopoulos, OJ, Ho, JK, Yezbick, A, et al. An experimental and clinical evaluation of a novel central venous catheter with integrated oximetry for pediatric patients undergoing cardiac surgery. Anesth Analg. 2007; I105(6):1598–1604.
![]() 10. Reinhart, K, Kuhn H-J, Hartog, C, et al, Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004; 30:1572–1578.
10. Reinhart, K, Kuhn H-J, Hartog, C, et al, Continuous central venous and pulmonary artery oxygen saturation monitoring in the critically ill. Intensive Care Med. 2004; 30:1572–1578.
11. Rivers, EP, Cobra, V, Whitmill, M, Early goal-directed therapy in severe sepsis and septic shock. a contempory review of the literature. Curr Opin Anesthesiol 2008; 21:128–140.
![]() 12. Vedrinne, C, et al. Predictive factors for usefulness of fiberoptic pulmonary artery catheter for continuous oxygen saturation in mixed venous blood monitoring in cardiac surgery. Anesth Analg. 1997; 85:2–10.
12. Vedrinne, C, et al. Predictive factors for usefulness of fiberoptic pulmonary artery catheter for continuous oxygen saturation in mixed venous blood monitoring in cardiac surgery. Anesth Analg. 1997; 85:2–10.
![]() 13. White, KM. Using continuous Svo2 to assess oxygen supply/demand balance in the critically ill patient. AACN Clin Issues Crit Care Nurs. 1993; 4:134–147.
13. White, KM. Using continuous Svo2 to assess oxygen supply/demand balance in the critically ill patient. AACN Clin Issues Crit Care Nurs. 1993; 4:134–147.
AACN. Severe sepsis. from www.aacn.org/WD/Practice/Docs/Severe_Sepsis_04-2006.pdf. [accessed].
AACN. Pulmonary artery pressure measurement. www.aacn.org/WD/Practice/Docs/PAP_Measurement_05-2004.pdf. [accessed].
Antonelli M, Levy, M, Andrews, PJD, et al. Hemodynamic monitoring in shock and implication for management, International Consensus Conference, Paris, France 27-28 April 2006. Intensive Care Med. 2007; 33(4):1–16.
Carcillo, JA, Fields, AI, American College of Critical Care Medicine Task Force Committee Members. Clinical -practice parameters for hemodynamic support of paediatric and neonatal patients in septic shock. Crit Care Med 2002; 30:1365–1378.
De Oliveira, CF, de Oliveira, DSF, Moura, JDGet al. ACCM/PALS haemodynamic support guidelines for paediatric septic shock. an outcomes comparison with and without monitoring central venous oxygen saturation. Intensive Care Med. 2008; 34(6):1065–1075.
Edwards Lifesciences LLC. Understanding continuous mixed venous oxygen saturation (Svo2) monitoring with the Swan-Ganz oximetry TD system. ed 2, Irvine, CA: Edwards Lifesciences; 2002.
Goodrich, C. Continuous central venous oximetry monitoring. Crit Care Nurs Clin North Am. 2006; 18:203–209.
Keckeisen, M Pulmonary artery pressure monitoring. In AACN protocols for practice. hemodynamic monitoring. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1998.
Rivers, EP, Ander, DS, Powell, D. Central venous oxygen saturation monitoring in the critically ill. Curr Opin Care. 2001; 7(3):204–211.