Procedure 15 Posterior Cervical Laminoplasty
Indications
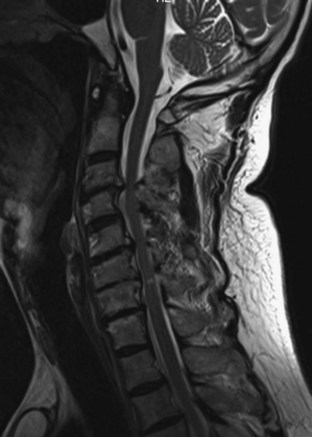
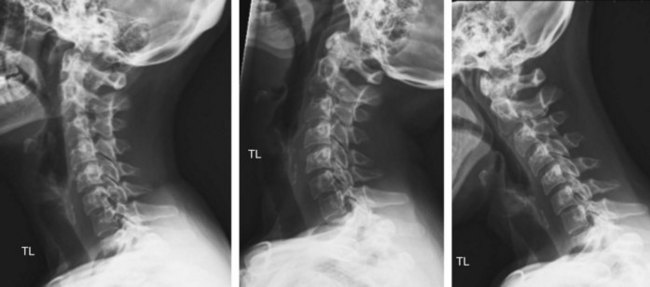
 Multilevel cervical spondylotic myelopathy in three or more motion segments (Figure 15-1)
Multilevel cervical spondylotic myelopathy in three or more motion segments (Figure 15-1)
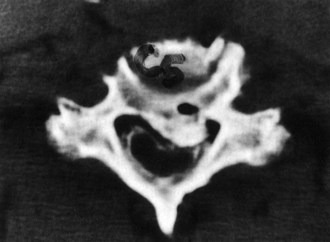
 Ossification of the posterior longitudinal ligament (OPLL) (Figure 15-2)
Ossification of the posterior longitudinal ligament (OPLL) (Figure 15-2)
Examination/Imaging
 Upper motor neuron signs (Hoffmann, clonus, up-going Babinski reflex, and finger escape sign)
Upper motor neuron signs (Hoffmann, clonus, up-going Babinski reflex, and finger escape sign)
 Difficulties with any activities requiring fine motor movements (buttoning shirt, writing)
Difficulties with any activities requiring fine motor movements (buttoning shirt, writing)
 Wasting of hand intrinsic musculature
Wasting of hand intrinsic musculature
 Computed tomography (CT) myelography: useful in patients unable to be evaluated by MRI and may be better for osseous evaluation and previous hardware placement.
Computed tomography (CT) myelography: useful in patients unable to be evaluated by MRI and may be better for osseous evaluation and previous hardware placement.
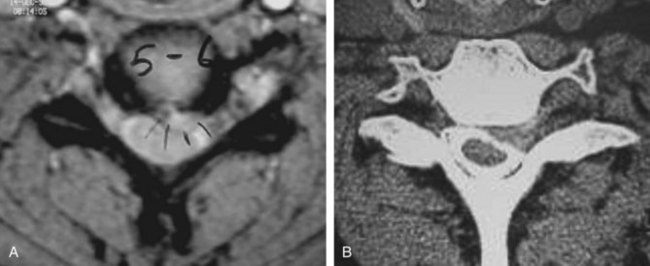
 Figure 15-5 shows axial MRI (A) and CT (B) myelogram demonstrating left-sided compression. The choice of opening side depends on the side of neurologic compression. In this example, the opening side would be the left side.
Figure 15-5 shows axial MRI (A) and CT (B) myelogram demonstrating left-sided compression. The choice of opening side depends on the side of neurologic compression. In this example, the opening side would be the left side.
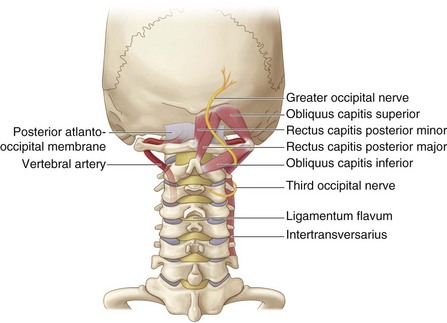
Surgical Anatomy
Positioning
 The patient’s hair is shaved up to the inferior margin of the occiput.
The patient’s hair is shaved up to the inferior margin of the occiput.
 The patient is placed prone with Mayfield tongs onto an operating room table with a Mayfield attachment.
The patient is placed prone with Mayfield tongs onto an operating room table with a Mayfield attachment.
 The head is positioned with the “chin-tucked and slightly forward-flexed” to facilitate exposure.
The head is positioned with the “chin-tucked and slightly forward-flexed” to facilitate exposure.
 Operating room bed positioning
Operating room bed positioning
 After the patient is positioned, the shoulders are taped down.
After the patient is positioned, the shoulders are taped down.
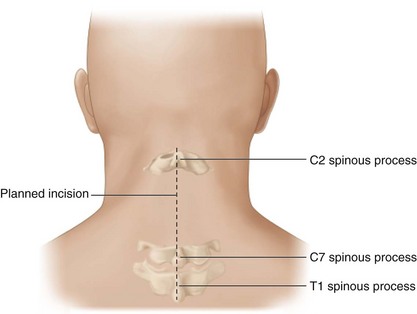
 A radiopaque skin marker may be used to estimate incision length, but C2 and C7 spinous processes are prominent and provide a good estimate of incision length.
A radiopaque skin marker may be used to estimate incision length, but C2 and C7 spinous processes are prominent and provide a good estimate of incision length.
Portals/Exposures
 The spinous processes of C2 and C7serve as superficial landmarks for the surgical incision.
The spinous processes of C2 and C7serve as superficial landmarks for the surgical incision.
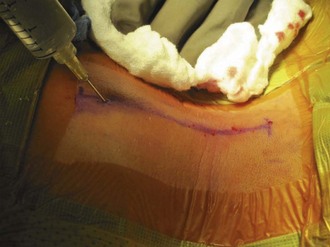
 Injection of local anesthetic with epinephrine into the paraspinal musculature minimizes bleeding (Figure 15-9).
Injection of local anesthetic with epinephrine into the paraspinal musculature minimizes bleeding (Figure 15-9).
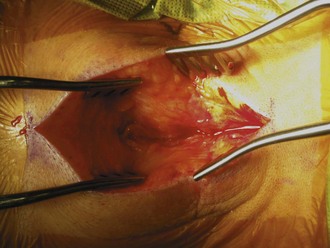
 Follow the nuchal line to the spinous processes (Figure 15-10). A careful midline dissection through the nuchal ligament minimizes muscular bleeding.
Follow the nuchal line to the spinous processes (Figure 15-10). A careful midline dissection through the nuchal ligament minimizes muscular bleeding.
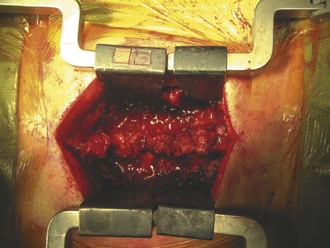
 Use standard exposure to the cervical spine from C2 to T1 (Figure 15-11).
Use standard exposure to the cervical spine from C2 to T1 (Figure 15-11).
 Perform subperiosteal dissection of the paracervical musculature out laterally to the medial edge of the facet joint.
Perform subperiosteal dissection of the paracervical musculature out laterally to the medial edge of the facet joint.
Procedure
 The authors will describe a modified “open-door laminoplasty” technique originally described by Hirabayashi and colleagues. The technique entails variations on laminoplasty types: They can be generally described as unilateral hinge (“open-door”) and bilateral hinge (“French door”) with supplemental procedures. Various supplemental methods are used to keep the laminoplasty door open (laminoplasty plates, suture use, and bone graft).
The authors will describe a modified “open-door laminoplasty” technique originally described by Hirabayashi and colleagues. The technique entails variations on laminoplasty types: They can be generally described as unilateral hinge (“open-door”) and bilateral hinge (“French door”) with supplemental procedures. Various supplemental methods are used to keep the laminoplasty door open (laminoplasty plates, suture use, and bone graft).
Step 1
 C3-7 spinous processes are removed to facilitate exposure and if spinous process sutures are not used.
C3-7 spinous processes are removed to facilitate exposure and if spinous process sutures are not used.
 A high-speed AM-8 burr (Midas Rex Pneumatic Tools, Fort Worth, Texas) is used to make two bony troughs at the medial aspect of the lateral mass or the lamina–facet junction (Figure 15-12).
A high-speed AM-8 burr (Midas Rex Pneumatic Tools, Fort Worth, Texas) is used to make two bony troughs at the medial aspect of the lateral mass or the lamina–facet junction (Figure 15-12).
 The lamina is thicker at the superior margin and thinner inferiorly.
The lamina is thicker at the superior margin and thinner inferiorly.
 On the hinge side, only one cortical layer and cancellous bone is removed with a burr, taking care not to burr through the second cortical layer.
On the hinge side, only one cortical layer and cancellous bone is removed with a burr, taking care not to burr through the second cortical layer.
 The opening side is removed with a burr bicortically (cortical-cancellous-cortical bone layer).
The opening side is removed with a burr bicortically (cortical-cancellous-cortical bone layer).
Step 2
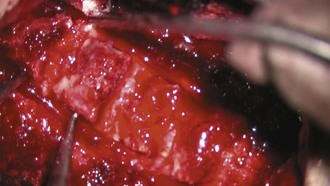
 Ligamentum flavum from the C2-3 interspace and C7-T1 interspace is excised with a Kerrison rongeur (Figure 15-13, A and B). Ligamentum flavum is excised at both interlaminar spaces at the cephalad and caudad levels of the laminoplasty.
Ligamentum flavum from the C2-3 interspace and C7-T1 interspace is excised with a Kerrison rongeur (Figure 15-13, A and B). Ligamentum flavum is excised at both interlaminar spaces at the cephalad and caudad levels of the laminoplasty.
 Any dural adhesions on the opening side are freed with curettes and 2-mm Kerrison rongeurs (Figure 15-14).
Any dural adhesions on the opening side are freed with curettes and 2-mm Kerrison rongeurs (Figure 15-14).
Step 3
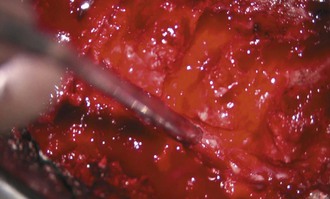
 The hinge side is carefully opened by the operative assistant, using small forward-angled curettes or skin hooks.
The hinge side is carefully opened by the operative assistant, using small forward-angled curettes or skin hooks.
 The lamina is opened slowly to allow gentle creep of the lamina and spinal cord, and it is opened just enough to accommodate a 6- to 8-mm bone graft.
The lamina is opened slowly to allow gentle creep of the lamina and spinal cord, and it is opened just enough to accommodate a 6- to 8-mm bone graft.
Step 3 Pearls
• Be careful not to be overly aggressive. A 6- to 8-mm opening achieves good decompression with less risk of posterior migration of spinal cord and root tension.
• Allograft trial spacers (Figure 15-15) are used to estimate graft size.
• Allograft spacers are applied on the opening side (Figure 15-16).
Step 4
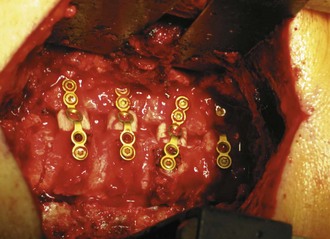
 Laminoplasty plates are sequentially applied, and typically, the lateral mass and laminar screws are 8 and 6 mm deep, respectively (Figures 15-17 and 15-18).
Laminoplasty plates are sequentially applied, and typically, the lateral mass and laminar screws are 8 and 6 mm deep, respectively (Figures 15-17 and 15-18).
 Plates allow immediate postoperative stability and mobilization of cervical spine with no bracing required.
Plates allow immediate postoperative stability and mobilization of cervical spine with no bracing required.
 Alternatively, sutures may be used to keep the laminoplasty open via spinous process sutures tensioned on the facet joint capsule and paraspinal musculature.
Alternatively, sutures may be used to keep the laminoplasty open via spinous process sutures tensioned on the facet joint capsule and paraspinal musculature.
 Hemostasis is achieved with a combination of bone wax, Gelfoam, and thrombin.
Hemostasis is achieved with a combination of bone wax, Gelfoam, and thrombin.
Postoperative Care and Expected Outcomes
Herkowitz HN. A comparison of anterior cervical fusion, cervical laminectomy, and cervical laminoplasty for the surgical management of multiple level spondylotic radiculopathy. Spine. 1988;13:774-780.
Hirabayashi K, Watanabe K, Wakano K, et al. Expansive open-door laminoplasty for cervical spinal stenotic myelopathy. Spine. 1983;8:693-699.
Park AE, Heller JG. Cervical laminoplasty: use of a novel titanium plate to maintain canal expansion–surgical technique. J Spinal Disord Tech. 2004;17:265-271.
Satomi K, Ogawa J, Ishii Y, Hirabayashi K. Short-term complications and long-term results of expansive open-door laminoplasty for cervical stenotic myelopathy. Spine J. 2001;1:26-30.