Procedure 14 Posterior Cervical Osteotomy Techniques
Indications
Indications Pitfalls
• Anterior neural compression—may require anterior decompression before deformity correction
• Ossification of the posterior longitudinal ligament—may be adherent to or penetrate ventral dura
• Osteoporosis—may require longer fixation construct
• Chronic steroid dependency—may require use of bone morphogenetic protein in addition to local autograft
Treatment Options
• Pedicle subtraction osteotomy (PSO)—single, posterior-only approach, and focal deformity correction
• Combined procedures—posterior only: thoracic osteotomies (Ponte or Smith-Petersen with or without C7 or T1 PSO); combined anteroposterior (AP) deformity correction: one or more anterior cervical diskectomy and fusion combined with posterior thoracic osteotomies (Ponte, Smith-Petersen, PSO)
Procedure Notes
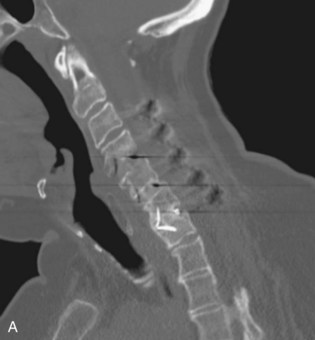
 The cervical-thoracic PSO can be performed following a lumbar PSO in a patient with global spinal kyphosis—C7 plumb line anterior to the L5-S1 disk space—that still displays forward cervical decompensation. Figure 14-1, A is a preoperative lateral radiograph showing cervical-thoracic and thoracic-lumbar kyphosis in this patient with advanced ankylosing spondylitis. Figure 14-1, B shows a preoperative computed tomography (CT) scan in this patient with ankylosing spondylitis having cervical-thoracic kyphosis and forward decompensation. Figure 14-1, C is a lateral radiograph showing cervical-thoracic kyphosis. Figure 14-1, D is a lateral radiograph showing L2 PSO and T1 PSO with achievement of good sagittal balance.
The cervical-thoracic PSO can be performed following a lumbar PSO in a patient with global spinal kyphosis—C7 plumb line anterior to the L5-S1 disk space—that still displays forward cervical decompensation. Figure 14-1, A is a preoperative lateral radiograph showing cervical-thoracic and thoracic-lumbar kyphosis in this patient with advanced ankylosing spondylitis. Figure 14-1, B shows a preoperative computed tomography (CT) scan in this patient with ankylosing spondylitis having cervical-thoracic kyphosis and forward decompensation. Figure 14-1, C is a lateral radiograph showing cervical-thoracic kyphosis. Figure 14-1, D is a lateral radiograph showing L2 PSO and T1 PSO with achievement of good sagittal balance.
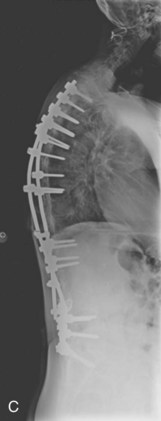
 Figure 14-2, A and B show a patient with a history of advanced rheumatoid arthritis and scoliosis with hardware failure after a Luque sublaminar wiring scoliosis correction with bilateral rods removal. The patient developed progressive cervical-thoracic and thoracic kyphosis and underwent an initial revision thoracic-to-sacral posterior spinal fusion (Figure 14-2, C). The cervical-thoracic kyphosis worsened, causing sagittal imbalance and fatigue-related pain. Figure 14-2, D is a full-length scoliosis radiograph showing the sagittal correction following a cervical-thoracic PSO. Figure 14-2, E and F show the preoperative and postoperative PSO, respectively.
Figure 14-2, A and B show a patient with a history of advanced rheumatoid arthritis and scoliosis with hardware failure after a Luque sublaminar wiring scoliosis correction with bilateral rods removal. The patient developed progressive cervical-thoracic and thoracic kyphosis and underwent an initial revision thoracic-to-sacral posterior spinal fusion (Figure 14-2, C). The cervical-thoracic kyphosis worsened, causing sagittal imbalance and fatigue-related pain. Figure 14-2, D is a full-length scoliosis radiograph showing the sagittal correction following a cervical-thoracic PSO. Figure 14-2, E and F show the preoperative and postoperative PSO, respectively.
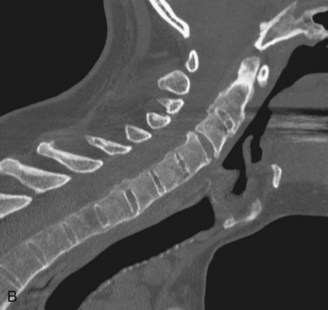
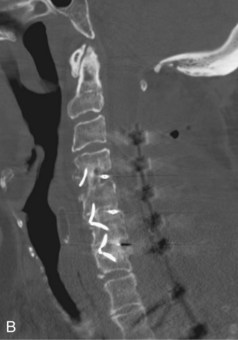
 A progression of surgical osteotomies can be performed to the extent needed to obtain adequate kyphosis correction, beginning with upper thoracic Ponte osteotomies, one or more Smith-Petersen osteotomies, and cervical-thoracic PSO. Preoperative (Figure 14-3, A) and postoperative (Figure 14-3, B) show midsagittal CT scans following Ponte and Smith-Petersen osteotomies for cervical-thoracic kyphosis correction in an achondroplastic dwarf who developed progressive cervical-thoracic kyphosis after C1-T12 laminectomy for central spinal stenosis (25 years earlier), and after a C3-C7 fusion (2 years earlier). Note that a PSO was not necessary in this patient. Note the preoperative (Figure 14-3, C) versus postoperative (Figure 14-3, D) paraspinal CT scan showing the anterior column lengthening at C7-T1 that occurs following Smith-Petersen osteotomies. This is in contrast to posterior column shortening that occurs following a PSO (see Figure 14-2, F).
A progression of surgical osteotomies can be performed to the extent needed to obtain adequate kyphosis correction, beginning with upper thoracic Ponte osteotomies, one or more Smith-Petersen osteotomies, and cervical-thoracic PSO. Preoperative (Figure 14-3, A) and postoperative (Figure 14-3, B) show midsagittal CT scans following Ponte and Smith-Petersen osteotomies for cervical-thoracic kyphosis correction in an achondroplastic dwarf who developed progressive cervical-thoracic kyphosis after C1-T12 laminectomy for central spinal stenosis (25 years earlier), and after a C3-C7 fusion (2 years earlier). Note that a PSO was not necessary in this patient. Note the preoperative (Figure 14-3, C) versus postoperative (Figure 14-3, D) paraspinal CT scan showing the anterior column lengthening at C7-T1 that occurs following Smith-Petersen osteotomies. This is in contrast to posterior column shortening that occurs following a PSO (see Figure 14-2, F).
Examination/Imaging
 Full-length standing scoliosis radiographs: AP and lateral radiographs with hips and knees in full extension
Full-length standing scoliosis radiographs: AP and lateral radiographs with hips and knees in full extension
 Cervical AP and lateral neutral, flexion, and extension radiographs
Cervical AP and lateral neutral, flexion, and extension radiographs
 Magnetic resonance imaging (MRI) is used to delineate cord compression and the course of the vertebral artery (verify entry into transverse foramen of C6 versus anomalous C7 entry point; rule out commonly encountered aberrant course if performing C2 pedicle instrumentation).
Magnetic resonance imaging (MRI) is used to delineate cord compression and the course of the vertebral artery (verify entry into transverse foramen of C6 versus anomalous C7 entry point; rule out commonly encountered aberrant course if performing C2 pedicle instrumentation).
Examination/Imaging Pearls
• Intraoperative correction of deformity can be performed by controlled repositioning in the Mayfield headholder. The spine surgeon or assistant should scrub out and carefully adjust the Mayfield to enable a gradual spinal correction under both direct visualization and fluoroscopic imaging for coronal and sagittal alignment. Check the spinal cord to ensure that only minimal wrinkling of dural occurs.
Surgical Anatomy
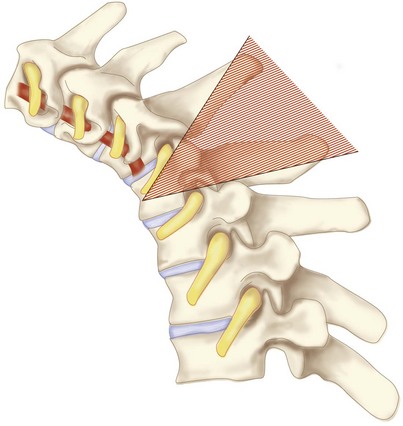
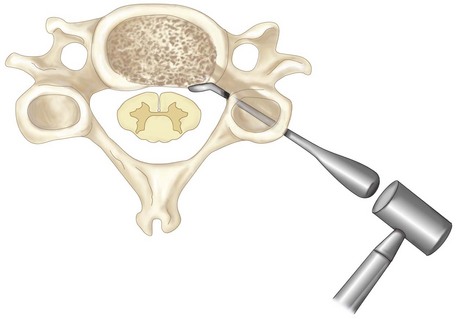
 PSO bone resection includes bilateral lamina, facets, and pedicles with wedge resection of anterior vertebral body (Figure 14-4).
PSO bone resection includes bilateral lamina, facets, and pedicles with wedge resection of anterior vertebral body (Figure 14-4).
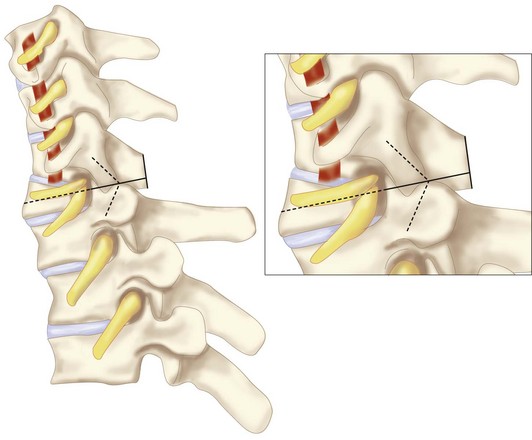
 Bony apposition of the posterior elements occurs once the osteotomy is closed. Two nerve roots will exit one foraminal opening (C7 and C8 if the PSO is at C7; C8 and T1 if the PSO is at T1) (Figure 14-5).
Bony apposition of the posterior elements occurs once the osteotomy is closed. Two nerve roots will exit one foraminal opening (C7 and C8 if the PSO is at C7; C8 and T1 if the PSO is at T1) (Figure 14-5).
Positioning
Positioning Equipment
• Intraoperative somatosensory evoked potentials and continuous electromyography are used to monitor cord and nerve root function, with special attention given at the time of deformity correction.
• A Cell Saver instrument is used to salvage blood loss from the osteotomy.
• Minimize use of bone wax during vertebral osteotomy, because this may interfere with bone fusion.
• Use thrombin-soaked Gelfoam or Floseal with cotton pledgets to control bleeding.
Procedure
Step 1
 A midline incision is made for the approach from C2 (or C3 if there is good bone quality, dysplastic C2 pedicles, or an anomalous vertebral artery) to T2 (or T3 if the PSO is performed at T1).
A midline incision is made for the approach from C2 (or C3 if there is good bone quality, dysplastic C2 pedicles, or an anomalous vertebral artery) to T2 (or T3 if the PSO is performed at T1).
 For a C7 PSO, place polyaxial facet screws from C3 to C6 and polyaxial pedicle screws at C2, T1, and T2.
For a C7 PSO, place polyaxial facet screws from C3 to C6 and polyaxial pedicle screws at C2, T1, and T2.
 For a T1 PSO, place polyaxial facet screws from C3 to C7 and polyaxial pedicle screws at C2, T2, and T3.
For a T1 PSO, place polyaxial facet screws from C3 to C7 and polyaxial pedicle screws at C2, T2, and T3.
Step 1 Pearls
• An anterior cervical diskectomy at one or more levels and lordotic implant(s) can be performed for neural decompression and to obtain direct correction of the kyphotic deformity.
• An anterior cervical plate can be used to augment to the anterior cervical fusion if needed.
• Uncovertebral joint resection can also be performed with anterior cervical decompression and fusion to obtain additional correction of deformity.
Step 2
 Bilateral laminectomy and facetectomy is completed at the PSO level, exposing the dura and bilateral nerve roots.
Bilateral laminectomy and facetectomy is completed at the PSO level, exposing the dura and bilateral nerve roots.
 Bilateral laminectomy is completed two levels above and two levels below the PSO level. This provides room for the spinal cord shortening after the deformity correction without experiencing compression from posterior bony elements.
Bilateral laminectomy is completed two levels above and two levels below the PSO level. This provides room for the spinal cord shortening after the deformity correction without experiencing compression from posterior bony elements.
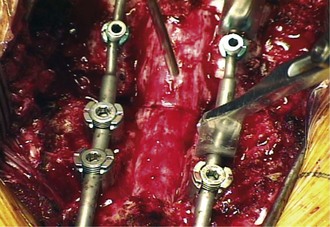
 Bilateral pedicles at the PSO level are sounded and drilled down to the vertebral body. In Figure 14-6, bilateral laminectomies have been completed at the PSO level and two levels above and below. Bilateral C7 and T1 facet joints have been resected for this T1 PSO. The pedicles are drilled bilaterally, and the cortical margins are thinned and then removed.
Bilateral pedicles at the PSO level are sounded and drilled down to the vertebral body. In Figure 14-6, bilateral laminectomies have been completed at the PSO level and two levels above and below. Bilateral C7 and T1 facet joints have been resected for this T1 PSO. The pedicles are drilled bilaterally, and the cortical margins are thinned and then removed.
 Cortical margins are resected with a combination of thin-lipped rongeur, pituitary rongeur, and curettes.
Cortical margins are resected with a combination of thin-lipped rongeur, pituitary rongeur, and curettes.
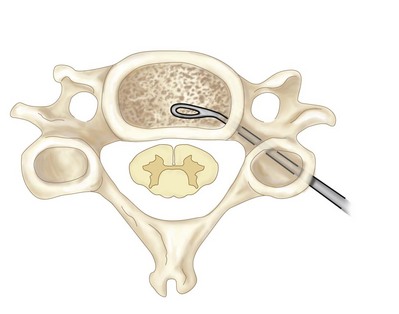
 A V-shaped wedge of cancellous bone is resected from the vertebral body with straight and curved curettes carried down through the pedicles and into the vertebral body (Figure 14-7). Resection of cancellous bone should be carried out to the anterior cortex. The cancellous osteotomy is carefully performed, staying within the margins of the vertebral body. Fluoroscopy is used to verify that the depth of the osteotomy is carried to the cortical margins of the vertebrae. The transverse processes of T1 can be vertically resected, and a careful cortical resection can be performed around the posterior lateral portion of the vertebral body bilaterally to complete the wedge osteotomy of the vertebrae. This is performed by subperiosteal dissection using a curved curette, followed by use of a 2-mm Kerrison rongeur. The segmental artery can be cauterized if necessary. This lateral cortical bone resection can help mobilize and close the wedged osteotomy.
A V-shaped wedge of cancellous bone is resected from the vertebral body with straight and curved curettes carried down through the pedicles and into the vertebral body (Figure 14-7). Resection of cancellous bone should be carried out to the anterior cortex. The cancellous osteotomy is carefully performed, staying within the margins of the vertebral body. Fluoroscopy is used to verify that the depth of the osteotomy is carried to the cortical margins of the vertebrae. The transverse processes of T1 can be vertically resected, and a careful cortical resection can be performed around the posterior lateral portion of the vertebral body bilaterally to complete the wedge osteotomy of the vertebrae. This is performed by subperiosteal dissection using a curved curette, followed by use of a 2-mm Kerrison rongeur. The segmental artery can be cauterized if necessary. This lateral cortical bone resection can help mobilize and close the wedged osteotomy.
 A temporary malleable rod can be attached to the pedicle screws and lateral mass screws to prevent anterior translation or sudden movement of the spinal cord before the posterior vertebral cortex is resected.
A temporary malleable rod can be attached to the pedicle screws and lateral mass screws to prevent anterior translation or sudden movement of the spinal cord before the posterior vertebral cortex is resected.
 Down-pushing Epstein curettes are used to depress the posterior and lateral vertebral cortices into the void of the vertebral body (Figure 14-8). This should be performed bilaterally and as the last step in the osteotomy. Following this step, the posterior osteotomy wedge will close down, and access to the osteotomy region is limited. A unilateral, temporary, malleable rod should be in place before performing this step. This rod will prevent complete collapse of the osteotomy.
Down-pushing Epstein curettes are used to depress the posterior and lateral vertebral cortices into the void of the vertebral body (Figure 14-8). This should be performed bilaterally and as the last step in the osteotomy. Following this step, the posterior osteotomy wedge will close down, and access to the osteotomy region is limited. A unilateral, temporary, malleable rod should be in place before performing this step. This rod will prevent complete collapse of the osteotomy.
Step 2 Pearls
• Remove the posterior vertebral cortical bone to complete the osteotomy. Resection of this bone bridge, just ventral to the dural sac, is the last step of the vertebral body osteotomy. This segment of bone maintains an open posterior vertebral window for completion of the vertebral wedge osteotomy. Once the posterior cortex is broken, the posterior vertebral body closes down and access to the vertebral body is decreased.
• Lateral intraoperative fluoroscopy is used to verify the depth of the vertebral osteotomy. Sequential images can be taken as the instruments employed for osteotomy are advanced anteriorly. A small curette can be placed anteriorly within the apex of the V-shaped osteotomy and imaged to verify depth, for example.
• Asymmetric osteotomy may be performed to correct for both sagittal and coronal deformity.
Step 2 Pitfalls
• Preoperative MRI and/or CT are necessary to evaluate the course of the vertebral artery. Aberrant coursing of the vertebral artery can occur such that it enters the transverse foramen of C7 or takes an anomalous course, endangering pedicle screw placement in C2.
• Failure to place a temporary rod may lead to translational instability and consequent neurologic deficit.
• Inadequate laminectomy, especially proximal and distal to the PSO level, may place the spinal cord at risk as reduction is obtained.
• Failure to maintain the posterior and lateral wall until the very end will cause premature instability and difficulty in controlling reduction.
• Hemostasis is critical throughout the procedure. Blood loss, which can be rapid and excessive during the osteotomy, especially from the cancellous vertebral bone, must be controlled.
Step 3
 The osteotomy is closed by releasing the Mayfield clamps, followed by controlled, manual elevation of the Mayfield headholder, then reclamping of the headholder. Watch the thecal sac and nerve roots to avoid compression injury.
The osteotomy is closed by releasing the Mayfield clamps, followed by controlled, manual elevation of the Mayfield headholder, then reclamping of the headholder. Watch the thecal sac and nerve roots to avoid compression injury.
 Obtain a lateral radiograph to check sagittal alignment.
Obtain a lateral radiograph to check sagittal alignment.
 An appropriately contoured rod is fixed to the pedicle/lateral mass screws on the side opposite the malleable temporary rod.
An appropriately contoured rod is fixed to the pedicle/lateral mass screws on the side opposite the malleable temporary rod.
 The malleable rod is removed, and a second contoured rod is attached.
The malleable rod is removed, and a second contoured rod is attached.
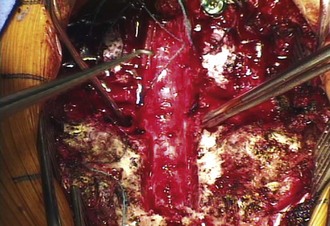
 Further reduction and compression across the osteotomy site is performed with the compression instrumentation (Figure 14-9). An infolding of the dura occurs following reduction of the kyphotic deformity.
Further reduction and compression across the osteotomy site is performed with the compression instrumentation (Figure 14-9). An infolding of the dura occurs following reduction of the kyphotic deformity.
 Cross-linked attachments can be used to increase stability of fixation.
Cross-linked attachments can be used to increase stability of fixation.
Postoperative Care and Expected Outcomes
 A closing-wedge osteotomy creates cervical lordosis.
A closing-wedge osteotomy creates cervical lordosis.
 Posterior elements are removed at the level of the osteotomy, and laminectomies two levels above and below are performed.
Posterior elements are removed at the level of the osteotomy, and laminectomies two levels above and below are performed.
 Bony apposition of anterior, middle, and posterior columns is established.
Bony apposition of anterior, middle, and posterior columns is established.
 Posterior instrumentation stabilizes the spine and maintains compression across the osteotomy site to increase fusion rate and success. A postoperative halo may be used if the patient is osteoporotic.
Posterior instrumentation stabilizes the spine and maintains compression across the osteotomy site to increase fusion rate and success. A postoperative halo may be used if the patient is osteoporotic.
 Postoperatively, the spinal column is shortened.
Postoperatively, the spinal column is shortened.
 The fulcrum for PSO is the anterior column; so, there is less risk for spinal cord injury versus a Smith-Petersen osteotomy, in which the fulcrum is the middle column.
The fulcrum for PSO is the anterior column; so, there is less risk for spinal cord injury versus a Smith-Petersen osteotomy, in which the fulcrum is the middle column.
Mummaneni PV, Mummaneni VP, Haid RW, Rodts GEJr, Sasso RC. Cervical osteotomy for the correction of chin-on-chest deformity in ankylosing spondylitis. Neurosurg Focus. 2003;14:e9.
Webb JK, Sengupta DK. Posterior cervicothoracic osteotomy. In: Vaccaro AR, Albert TJ, editors. Spine Surgery: Tricks of the Trade. New York: Thieme; 2003:35-37.