Small-Bore Feeding Tube Insertion and Care
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the upper and lower gastrointestinal (GI) tract is needed.
• The GI tract should be functioning for gastric feedings to be digested and absorbed. Bowel sounds may not be audible, yet the GI tract is functional and enteral nutrition can be instituted safely and effectively and be well tolerated. Gastrointestinal findings that may affect the normal functioning of the tract and preclude gastric feeding are bowel obstruction, paralytic ileus, and some fistulas.
• Small-bore feeding tubes are preferable over larger-bore nasogastric tubes during the course of critical illness because the risk for tissue necrosis at the nares and sinusitis is lower. When small-bore feeding tubes are placed postpylorically, there is a reduced risk of aspiration.
• The small diameter of the tube allows simultaneous oral intake if the patient is able to consume orally without aspiration.
• Both weighted (tubes with an enlarged tip, filled with tungsten) and unweighted (bolus tip) small-bore nasogastric tubes are available. They typically are packaged with guidewires already in the lumen to assist passage of the tube. After successful placement, the guidewire is removed and discarded. The size of tubes range from 7 to 12 Fr.
• Unweighted-tip tubes migrate postpylorically into the duodenum more often than tubes with weighted tips. Weighted-tip tubes are harder for the patient with a compromised condition to swallow; ultimately, the unweighted tube may be a more comfortable choice for the patient.
• Absolute contraindications for insertion of a nasogastric feeding tube are basilar skull fracture, transsphenoidal surgical approaches, and esophageal varices. Oral insertions are usually appropriate in these situations. Esophageal varices are a contraindication for any tube that transgresses the esophagus.
• Small-bore feeding tubes are not designed for drainage of gastric contents. If gastric decompression is desired, the small-bore nasogastric feeding tube should be replaced with a larger-bore nasogastric sump tube.
• It is important to review institutional standards regarding insertion of small-bore feeding tubes and complete competency for tube insertion.
• Some institutions restrict insertion to physicians and advanced practice nurses.
EQUIPMENT
PATIENT AND FAMILY EDUCATION
• Explain reason for insertion of tube and need for support of enteral nutrition.  Rationale: Knowledge may decrease anxiety and fear of the unknown.
Rationale: Knowledge may decrease anxiety and fear of the unknown.
• Explain how patient can assist with passage of the tube by positioning (e.g., sitting upright, head tipped forward and swallowing) when cued.  Rationale: Tube may pass more easily with patient cooperation.
Rationale: Tube may pass more easily with patient cooperation.
• Explain the risk for gag reflex stimulation during insertion.  Rationale: Knowledge may decrease anxiety and fear of the unknown.
Rationale: Knowledge may decrease anxiety and fear of the unknown.
• Explain the reason for the radiograph after insertion.  Rationale: Knowledge may decrease anxiety and fear of the unknown.
Rationale: Knowledge may decrease anxiety and fear of the unknown.
• Discuss reasons for not pulling at the tube once it has been placed and secured.  Rationale: Leaving the tube in place avoids the need for reinsertion and another radiograph for verification. Reinsertion increases risk for trauma to nasopharyngeal passages. Dislodgment of the tube can increase the risk of aspiration.
Rationale: Leaving the tube in place avoids the need for reinsertion and another radiograph for verification. Reinsertion increases risk for trauma to nasopharyngeal passages. Dislodgment of the tube can increase the risk of aspiration.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess for medical history of head and neck cancer and surgery, basilar skull fracture, esophageal cancer, decreased pharyngeal reflexes, or transsphenoidal pituitary resection.  Rationale: These conditions prohibit safe passage of a tube nasally through the pharynx. Inadvertent intracranial placement of the small-bore feeding tube is possible with a basilar skull fracture.
Rationale: These conditions prohibit safe passage of a tube nasally through the pharynx. Inadvertent intracranial placement of the small-bore feeding tube is possible with a basilar skull fracture.
• Assess patency of the nares for potential obstructions to feeding tube passage.  Rationale: A tube cannot pass through occlusion.
Rationale: A tube cannot pass through occlusion.
• Assess Gl function.  Rationale: A functional gut is needed for administration of enteral feedings.
Rationale: A functional gut is needed for administration of enteral feedings.
Patient Preparation
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• If the patient has a large-bore nasogastric tube, it needs to be removed before placement of the small-bore nasogastric tube.  Rationale: Passing a small-bore tube is extremely difficult with an oral or nasal tube already in place. Removal of the large-bore tube after placement of the small-bore tube will likely cause displacement of the newly placed small tube.
Rationale: Passing a small-bore tube is extremely difficult with an oral or nasal tube already in place. Removal of the large-bore tube after placement of the small-bore tube will likely cause displacement of the newly placed small tube.
• Perform oral care to moisten mucosa. Suction oropharyngeal area of excess secretions.1  Rationale: A moist, cleared oropharyngeal area facilitates patient comfort and passage of the tube.
Rationale: A moist, cleared oropharyngeal area facilitates patient comfort and passage of the tube.
References
1. AACN Practice Alert. Oral care in the critically ill,. www.aacn.org, 2007. [accessed 01/03/10].
2. AACN Practice Alert. Verification of feeding tube placement,. www.aacn.org, 2006. [accessed 01/03/10].
3. Baskin, WN. Acute complications associated with bedside placement of feeding tubes. Nutr Clin Pract. 2006; 21:40–55.
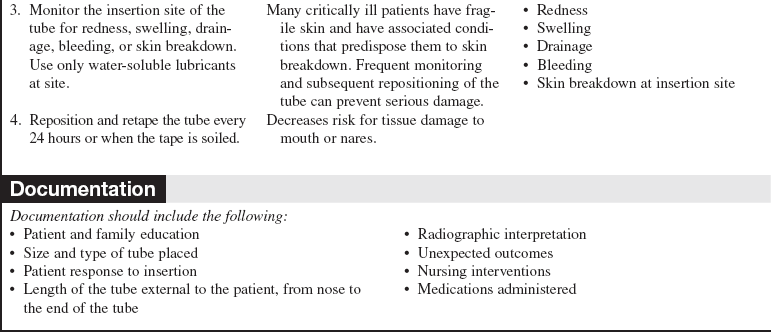
![]() 4. Burns, SM, et al. Comparison of nasogastric tube securing methods and tube types in medical intensive care patients. AJCC. 1995; 4:198–203.
4. Burns, SM, et al. Comparison of nasogastric tube securing methods and tube types in medical intensive care patients. AJCC. 1995; 4:198–203.
Metheny, NA, Schallom, ME, Edwards, SJ, Effect of gastrointestional motility and feeding tube site on aspiration risk in critically ill patients. a review. Heart Lung 2004; 33:131–145.
6. Metheny, NA, Preventing respiratory complications of tube feedings. evidence-based practice. Am J Crit Care 2006; 15:360–369.
7. Sorokin, R, Gottleib, JE, Enhancing patient safety during feeding tube insertion. a review of more than 2000 insertions. JPEN 2006; 30:440–445.
Guenter, P, Silkroski, M, Tube feeding. practical guidelines and nursing protocols,. Aspen Publishers, Silver Spring, MD, 2001.
Lord, LM, et al. Comparison of weighted vs unweighted enteral feeding tubes for efficacy of transpyloric intubation. JPEN. 1993; 17:271–273.
Metheny, N. Assessing placement of feeding tubes. AJN. 2002; 101:36–45.