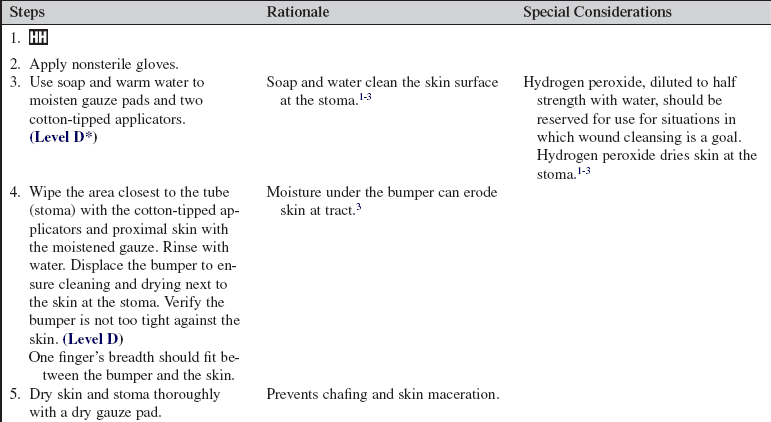
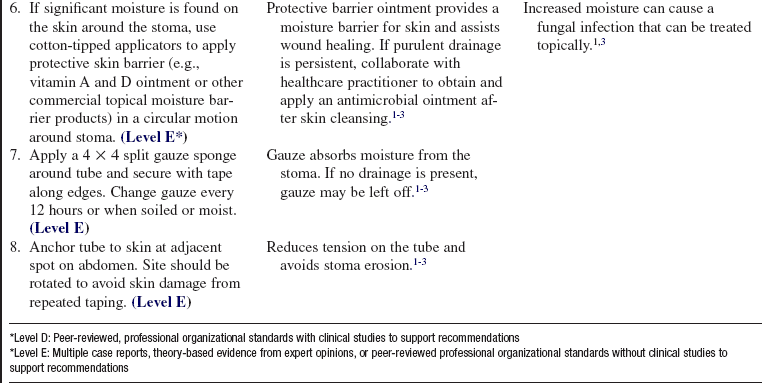
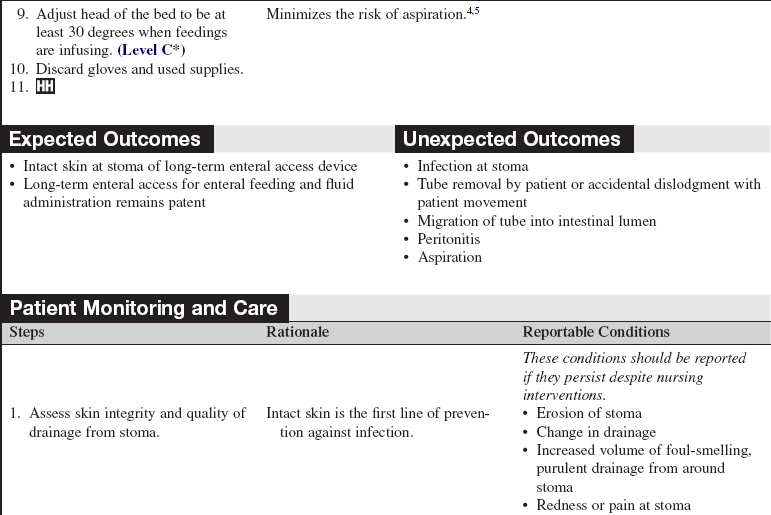
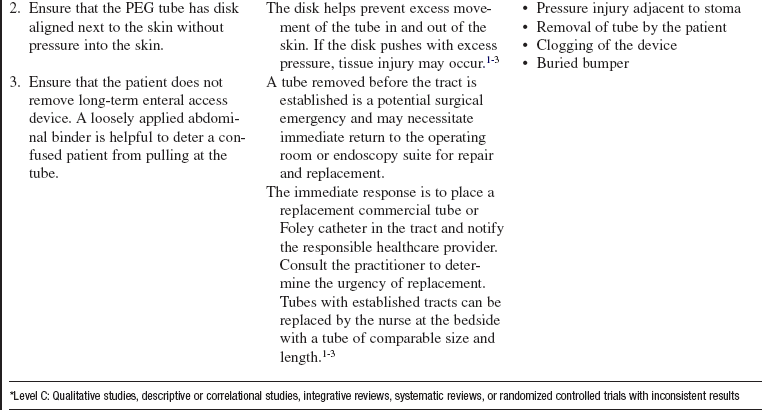
Percutaneous Endoscopic Gastrostomy (PEG), Gastrostomy, and Jejunostomy Tube Care
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the upper and lower gastrointestinal (GI) system is necessary.
• Patients who cannot have enteral tubes passed orally or nasally because of anatomy or surgery and those who need supplemental enteral nutrition support for longer than 4 weeks should be considered as candidates for long-term enteral access.
• The most commonly used long-term enteral access is the percutaneous endoscopic gastrostomy (PEG) tube. The PEG tube is inserted without general anesthesia. The use of a local anesthetic (i.e., 1% lidocaine injection) is used at the abdominal puncture site. A guidewire is threaded via endoscope through the oropharynx, esophagus, and stomach and brought out through the abdominal wall. The tube is then threaded over the guidewire and passed into the stomach. The tapered end of the tube is brought through a stab wound in the abdominal wall until the mushroomed end of the tube is set against the stomach wall. An adapter for infusion is attached to the end of the tube, and a disk on the tube is moved up to the abdominal wall to stabilize the tube in place.
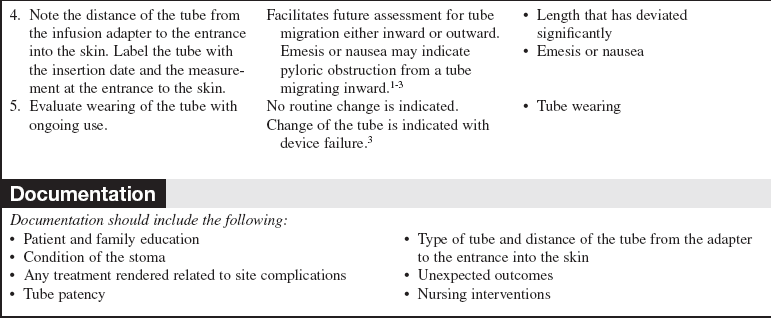
• PEG tubes are large-bore catheters that range from 18 to 22 Fr and have a mushroom-shaped curved end in the stomach and a two-port distal end to instill enteral nutrition, medications, and fluid. Commercial PEG tubes have disks, perpendicular to the tube, to hold the device close to the skin and lessen shift of tube in and out of the skin (Fig. 133-1).
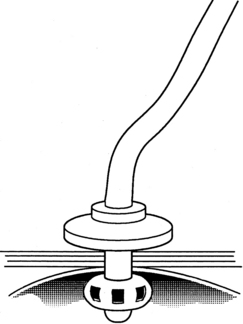
Figure 133-1 Percutaneous endoscopic gastrostomy.
• Relative contraindications for PEG placement include the following:
• Replacement gastrostomy tubes usually have a balloon in the intestinal lumen that is inflated with sterile water. This balloon prevents inadvertent dislocation. The distal end of the tube has an infusion port and a port for the balloon instillation (Fig. 133-2).
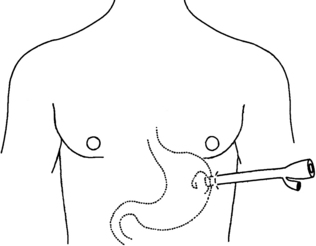
Figure 133-2 Gastrostomy tube.
• A jejunostomy tube, which does not have a balloon, is indicated in those patients at risk for aspiration or who are unable to tolerate enteral feedings into the stomach. These tubes are routinely sutured in place for stability (Fig. 133-3). They are usually smaller bore, less than 14 Fr, and therefore are more prone to occlusion.
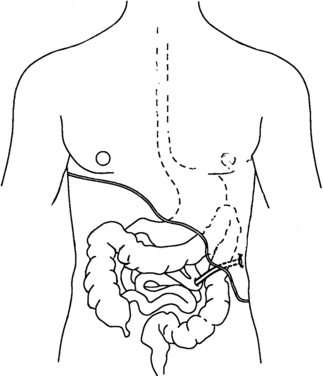
Figure 133-3 Jejunostomy tube placement.
• If the tubes are inadvertently removed, reinsertion of the tubes is a routine procedure after the tunnel and stoma are healed (approximately 2 to 6 weeks after insertion).
• Because these tubes all enter through the abdominal wall, skin care at the site of insertion is important for skin integrity and prevention of infection.
• Consult with the multidisciplinary team to individualize nutrition goals. The nutrition plan is developed on the basis of the collaborative assessment of the nurse, dietitian, and physician or advance practice nurse.
EQUIPMENT
• Protective skin barrier (e.g., vitamin A and D ointment)
• Silk tape (or paper tape if patient has a sensitivity to silk tape)
Additional equipment to have available, as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the purpose for the tube.  Rationale: Knowledge may decrease anxiety and fear of the unknown.
Rationale: Knowledge may decrease anxiety and fear of the unknown.
• Explain reason for skin care assessment and maintenance.  Rationale: Knowledge may decrease anxiety and fear of the unknown.
Rationale: Knowledge may decrease anxiety and fear of the unknown.
• Stress the importance of not pulling at the tube.  Rationale: Unnecessary pain and skin irritation may be avoided.
Rationale: Unnecessary pain and skin irritation may be avoided.
• Oral nutrition is possible with the long-term enteral access catheter.  Rationale: Knowledge may decrease anxiety and fear of the unknown.
Rationale: Knowledge may decrease anxiety and fear of the unknown.
• Long-term enteral access catheters can be removed when oral intake meets the needs of the individual.  Rationale: Knowledge may decrease anxiety and fear of the unknown. This also may be a goal for the patient to consume more via the oral route.
Rationale: Knowledge may decrease anxiety and fear of the unknown. This also may be a goal for the patient to consume more via the oral route.
• Aspiration is a continued risk when the patient is positioned flat.  Rationale: Gastric residual volume can reflux and create a risk for pulmonary aspiration.
Rationale: Gastric residual volume can reflux and create a risk for pulmonary aspiration.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
Patient Preparation
• Ensure that patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Assist patient to position of comfort.  Rationale: Stoma of tube is easily accessible.
Rationale: Stoma of tube is easily accessible.
References
1. Baskin, WN. Acute complications associated with bedside placement of feeding tubes. Nutr Clin Pract. 2006; 21:40–55.
![]() 2. Loser, C, Aschl, G, Hebuterne, et al. ESPEN guidelines on artificial enteral nutrition-percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005; 24:845–861.
2. Loser, C, Aschl, G, Hebuterne, et al. ESPEN guidelines on artificial enteral nutrition-percutaneous endoscopic gastrostomy (PEG). Clin Nutr. 2005; 24:845–861.
![]() 3. McClave, SA, Neff, RL. Care and long term maintenance of percutaneous endoscopic gastrostomy tubes. JPEN. 2006; 30:S27–S38.
3. McClave, SA, Neff, RL. Care and long term maintenance of percutaneous endoscopic gastrostomy tubes. JPEN. 2006; 30:S27–S38.
![]() 4. Metheny, NA, Schallom, ME, Edwards, SJ, Effect of gastrointestinal motility and feeding tube site on aspiration risk in critically ill patients. a review. Heart Lung 2004; 33:131–145.
4. Metheny, NA, Schallom, ME, Edwards, SJ, Effect of gastrointestinal motility and feeding tube site on aspiration risk in critically ill patients. a review. Heart Lung 2004; 33:131–145.
5. Metheny, NA, Preventing respiratory complications of -tube feedings. evidence-based practice. Am J Crit Care 2006; 15:360–369.
Guenter, P, Silkroski, M, Tube feeding. practical guidelines and nursing protocols. Aspen Publishing, Silver Spring, MD, 2001.
Heiser, M, Malaty, H, Balloon type versus nonballoon type replacement percutaneous endoscopic gastrostomy. which is better. Gastroenterol Nurs 2001; 24:58–63.
Lord, LM. Enteral access devices. Nurs Clin North Am. 1997; 32:685–702.







 Rationale: A patient needs a functional gut to receive enteral nutrition.
Rationale: A patient needs a functional gut to receive enteral nutrition.




 Rationale: Intact skin integrity is a defense against infection. Early assessment of signs of infection promotes early, appropriate intervention.
Rationale: Intact skin integrity is a defense against infection. Early assessment of signs of infection promotes early, appropriate intervention.