Drain Removal
PREREQUISITE NURSING KNOWLEDGE
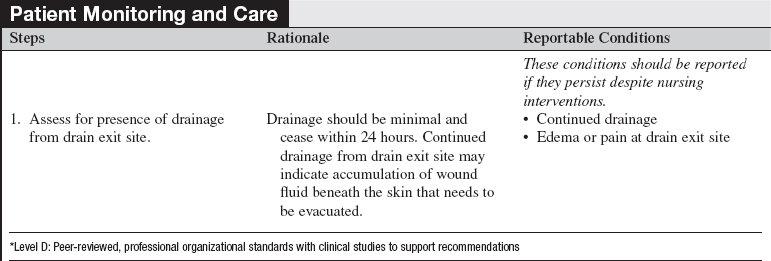
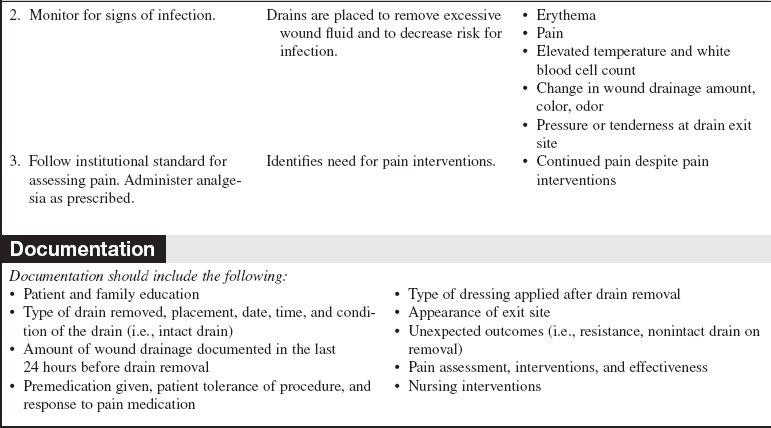
• Goals of wound care should be clearly outlined so that proper wound care products are used after drain removal. The wound care products selected are based on the size, location, and care of the wound bed needs and include continued moisture management.
• Continue to monitor the wound bed after drain removal; mark dressing for presence of leakage after drain removal and continue to monitor.
• Apply appropriate dressing after drain removal. Coarse gauze absorbs wound fluid but may adhere to wound bed; calcium alginates, foams, and hydrofiber dressings enhance wound absorption; hydrogels provide moisture to nondraining wounds; hydrocolloids provide wound moisture with minimal absorption; and film dressings are for nonexudating wounds.3–7
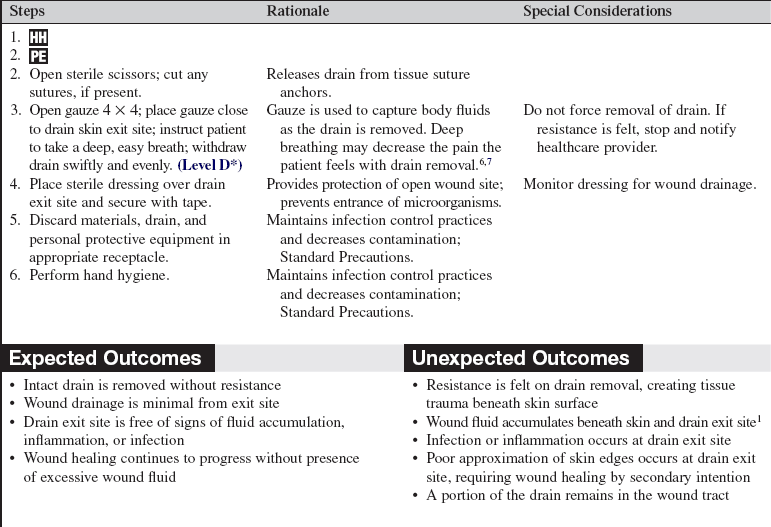
• Drains are placed in wounds to facilitate healing by providing an exit for excessive fluid accumulation in or near the wound bed. Drains may be removed when drainage is considered to be minimal.1,7
• Type of drain, location, and how the drain is secured should be known before drain removal. Competence should be demonstrated by the clinician performing drain removal because significant tissue injury may result from an improperly removed drain.1 With drain removal, never force removal of the drain. If resistance is felt, stop and notify healthcare provider.
• Common surgically placed wound drains include Hemovac (Zimmer Inc., Warsaw, IN), bulb suction drain (e.g. Jackson-Pratt or JP drain), and Penrose. Negative-pressure wound therapy devices may also be placed to assist with wound drainage.2
PATIENT AND FAMILY EDUCATION
• Explain the procedure and reason for drain removal.  Rationale: Patient anxiety and discomfort are decreased.
Rationale: Patient anxiety and discomfort are decreased.
• Discuss patient’s role in drain removal.  Rationale: Patient cooperation is elicited; patient is prepared for wound management on discharge.
Rationale: Patient cooperation is elicited; patient is prepared for wound management on discharge.
• Provide patient education regarding monitoring wound for drainage.  Rationale: Patient is engaged in care of the wound site in preparation of discharge.
Rationale: Patient is engaged in care of the wound site in preparation of discharge.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Signs of wound infection at drain site include:
 Change in the amount, odor, or characteristics of wound drainage
Change in the amount, odor, or characteristics of wound drainage
 Pressure or tenderness at drain exit site
Pressure or tenderness at drain exit site
 Rationale: Drains are placed to remove excessive wound fluid and decrease the risk for infection. Changes in wound drainage may indicate presence of infection; early detection of infection facilitates prompt and appropriate interventions.
Rationale: Drains are placed to remove excessive wound fluid and decrease the risk for infection. Changes in wound drainage may indicate presence of infection; early detection of infection facilitates prompt and appropriate interventions.
Patient Preparation
• Ensure that patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Premedicate patient with prescribed analgesic, if needed.  Rationale: Patients may not need premedication for drain removal; however, the patient’s pain and need for analgesia should be assessed before the procedure and treated appropriately.
Rationale: Patients may not need premedication for drain removal; however, the patient’s pain and need for analgesia should be assessed before the procedure and treated appropriately.
• Optimize lighting in room and provide privacy for patient.  Rationale: These measures allow for optimal assessment and patient comfort.
Rationale: These measures allow for optimal assessment and patient comfort.
References
1. Bates-Jensen B, Woolfolk, N, Acute surgical wound management Sussman C, Bates-Jensen B, eds.. Wound care: a collaborative practice manual for health professional. ed 3. Lippincott -Williams & Wilkins, Philadelphia, 2007:323–335.
2. Bovill, E, Banwell, PE, Teot, L, et al, Topical negative pressure wound therapy. a review of its role and guidelines for its use in the management of acute wounds. Int Wound J 2008; 10:1–19.
3. Fleck, CA. Wound assessment parameters and dressing selection. Adv Skin Wound Care. 2006; 19:364–370.
4. Gray, M, Wier, D, Prevention and treatment of moisture-associated skin damage (maceration) in the periwound skin . JWOCN 2007; 43:153–157.
5. Sussman, G, Management of the wound environment with dressings and topical agentsSussman C, Bates-Jensen B, eds.. Wound care . a collaborative practice manual for health professionals. ed 3. Lippincott Williams & Wilkins, Philadelphia, 2007:250–267.
6. Vuolo, JC. Assessment and management of surgical wounds in clinical practice. Nurs Stand. 2006; 20:46–56.
7. Walker, J. Patient preparation for safe removal of surgical drains. Nurs Stand. 2007; 21:39–41.