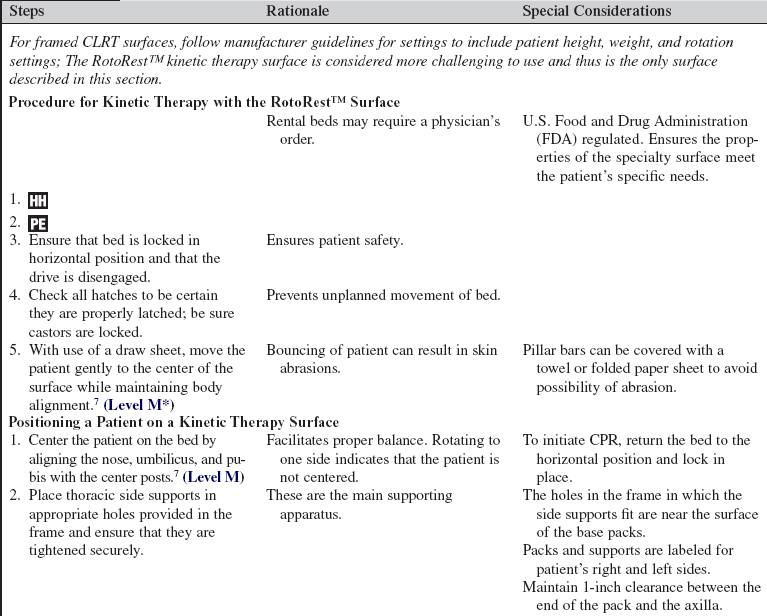
Pressure Redistribution Surfaces: Continual Lateral Rotation Therapy and RotoRest™ Lateral Rotation Surface
The purpose of pressure redistribution surface (i.e., support surface) is to assist in the reduction of pressure over areas of the body and reduce the development of pressure ulcers and other skin breakdown.9 Continual lateral rotation therapy provides dynamic rotation of a support surface to enhance mobilization and removal of pulmonary secretions for pulmonary benefit and to assist in preventing and treating physiologic complications of immobility. The RotoRest™ Lateral Rotation Surface is a unique kinetic therapy surface that can be perceived to be technically challenging to use. This surface is ideal for patients with traumatic injury, unstable spine, and traction and for patients who need aggressive rotation therapy.
PREREQUISITE NURSING KNOWLEDGE
• Principles of prevention of pressure-induced injury should be understood, including high-risk areas for tissue injury in the critically ill patient.12,13 High-risk areas of pressure injury include the occiput, coccyx, and heels.11 Prolonged external pressure over bony prominences, shear and friction forces, and excessive moisture increase the risk of pressure ulcers.
• With use of a validated pressure ulcer risk assessment tool such as the Braden Scale, a patient’s risk for a pressure ulcer should be assessed on admission to the intensive care unit (ICU), and at least every 12 to 24 hours thereafter, or with changes in patient condition. Interventions to prevent pressure ulcer development should target characteristics that put the patient at risk.1,2
• Redistribution of pressure includes frequent repositioning and use of support surfaces.4,6
• A pressure redistribution support surface is defined as a device designed for management of tissue loads, microclimate, or other therapeutic functions.9
 Pressure redistribution support surfaces may be powered or nonpowered.
Pressure redistribution support surfaces may be powered or nonpowered.
 Newer acute care mattresses incorporate pressure reduction technology.
Newer acute care mattresses incorporate pressure reduction technology.
 Preventive interventions, such as turning, monitoring nutrition, containing excessive moisture, and preventing shear and friction, are indicated with the use of a specialty surface.
Preventive interventions, such as turning, monitoring nutrition, containing excessive moisture, and preventing shear and friction, are indicated with the use of a specialty surface.
 Layers of linen placed on the surface should be limited to allow maximal benefit of the surface with the patient’s skin.
Layers of linen placed on the surface should be limited to allow maximal benefit of the surface with the patient’s skin.
• The many types of pressure redistribution surfaces range from the standard acute care foam mattress to air-filled or fluid-filled surfaces. Generally, the more specialized surfaces are indicated for certain wounds or patient conditions that result in excessive moisture, posterior grafts or wounds, flaps, etc. Because the technology in pressure redistribution surfaces changes rapidly, practitioners should investigate the specific properties of available specialty mattresses to choose the correct surface for a patient.
• Bariatric pressure reduction surfaces provide similar properties to all special bed surfaces; however, they are wider, and the frame and surface are designed to accommodate heavier patients.
 For maximal effects from pressure reduction therapy (low air loss, etc.), the weight of the patient must be tolerated by the surface.
For maximal effects from pressure reduction therapy (low air loss, etc.), the weight of the patient must be tolerated by the surface.
 Most ICU bed frames and specialty surfaces can support a patient up to 300 lbs. If the weight is greater than 300 lbs, the patient may need to move to a bariatric pressure reduction surface (refer to manufacturer’s guidelines for maximum weight limit of ICU bed frame and support surface).
Most ICU bed frames and specialty surfaces can support a patient up to 300 lbs. If the weight is greater than 300 lbs, the patient may need to move to a bariatric pressure reduction surface (refer to manufacturer’s guidelines for maximum weight limit of ICU bed frame and support surface).
• Principles of wound healing should be understood and include evaluation of the patient’s:
 Overall risk as assessed with a valid risk assessment tool (i.e., Braden score)2
Overall risk as assessed with a valid risk assessment tool (i.e., Braden score)2
 Nutritional status, including endpoint goals
Nutritional status, including endpoint goals
 The presence of incontinence-associated moisture and effective management of diarrhea and urine
The presence of incontinence-associated moisture and effective management of diarrhea and urine
• Understanding of the pathophysiology of tissue ischemia is an important assessment parameter of the integumentary system in the complex critically ill patient. Tissue ischemia may be caused by direct pressure applied to tissues and by disease processes and medications (i.e., vasoactive medications).
• The terms continual lateral rotation therapy (CLRT) and kinetic therapy are often loosely used in a similar context.5 CLRT is defined as the continuous turning of a patient from side to side with a less than 40-degree rotation; kinetic therapy is a 40-degree or greater rotation.5
• Support surfaces used to provide CLRT should have dynamic features to assist in pressure reduction over bony prominences. Special features may include:
 Low air loss to assist in management of excessive moisture
Low air loss to assist in management of excessive moisture
 Alternating pressure that provides pressure redistribution in a cyclic fashion to offload tissues
Alternating pressure that provides pressure redistribution in a cyclic fashion to offload tissues
 Multizoned surface in which different segments of the surface can have different pressure redistribution capabilities
Multizoned surface in which different segments of the surface can have different pressure redistribution capabilities
• RotoRest™ (KCI Licensing, Inc, San Antonio, TX) lateral rotation surface is a kinetic therapy surface that does not incorporate low air loss into its technology, but if the patient is in continuous motion (rotation), pressure over bony prominences may be relieved during the continuous turning therapy. However, because of the aggressive degree of the turn, possible shear and friction injuries of the skin can occur during rotation.
• Knowledge is needed concerning the physiologic effects of immobility on body systems, including factors that contribute to impaired circulation. Potential complications in the critically ill patient include:
• Principles for successful use of CLRT therapy include clinician appreciation of the goals of therapy. For maximal benefit, the support surface should be in rotation more than 18 hours per day and at optimal rotation.5,6
 The support surface should provide continuous rotation at varying degrees.
The support surface should provide continuous rotation at varying degrees.
 Surface provides continuous, slow, side-to-side turning of the patient with rotation of the therapeutic surface. The degree of rotation, and the time interval for rotation, is set by the clinician. The degree of rotation is set on each side, intermittently or constantly providing unilateral or bilateral rotation.
Surface provides continuous, slow, side-to-side turning of the patient with rotation of the therapeutic surface. The degree of rotation, and the time interval for rotation, is set by the clinician. The degree of rotation is set on each side, intermittently or constantly providing unilateral or bilateral rotation.
 Serial skin assessments per institutional protocols are still required when patients are on rotational therapy surfaces.
Serial skin assessments per institutional protocols are still required when patients are on rotational therapy surfaces.
 The clinician should evaluate the patient’s tolerance of CLRT/kinetic therapy and consider sedation and analgesics as appropriate.
The clinician should evaluate the patient’s tolerance of CLRT/kinetic therapy and consider sedation and analgesics as appropriate.
• Indications for CLRT include critically ill patients who are at a higher risk of pulmonary complications such as:
 Patients with increasing ventilatory support requirements
Patients with increasing ventilatory support requirements
 Patients at risk for ventilator-associated pneumonia (VAP)14
Patients at risk for ventilator-associated pneumonia (VAP)14
 Patients who have clinical indications for acute lung injury or adult respiratory distress syndrome (ARDS)3:
Patients who have clinical indications for acute lung injury or adult respiratory distress syndrome (ARDS)3:
• Trauma diagnosis and spinal cord injury should be understood. Low air-loss surfaces are contraindicated for patients with unstable spine or pelvic injuries until the injury is stabilized. The RotoRest™ surface may be used with spinal injuries; additional care is necessary to place unstable spinal cord injuries or patients with pelvic instability on a RotoRest™ surface that has a firm, flat surface. Cervical traction and skeletal traction may be used with a RotoRest™ therapy surface.
• Patients should be placed on a pressure reduction surface as soon as possible to reduce the risk of pressure-associated tissue injury. Patients should be placed on a lateral rotation support surface as soon as possible to prevent negative effects of immobility and possible pulmonary complications.4,8,13
• When ordering a CLRT or kinetic therapy, the clinician should assess properties of the pressure redistribution surface and evaluate patient skin/tissue redistribution needs (i.e., moisture control, pressure redistribution).
• Regarding the CLRT support surface:
 Several support surfaces are available for CLRT. Refer to hospital policy for types of support surfaces that may be used.
Several support surfaces are available for CLRT. Refer to hospital policy for types of support surfaces that may be used.
 Evaluate the specific needs of the patient to include pulmonary indications for CLRT, including contraindications such as traction, unstable spine, and pelvic injuries.
Evaluate the specific needs of the patient to include pulmonary indications for CLRT, including contraindications such as traction, unstable spine, and pelvic injuries.
 Manufacturer-specific guidelines for implementing CLRT should be reviewed before the patient is placed on the support surface/bed frame.
Manufacturer-specific guidelines for implementing CLRT should be reviewed before the patient is placed on the support surface/bed frame.
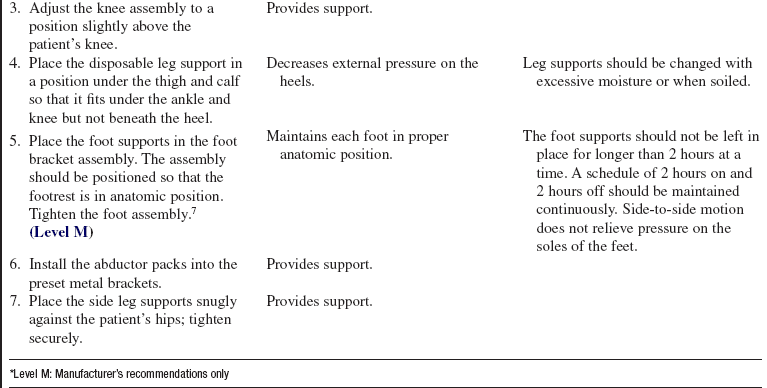
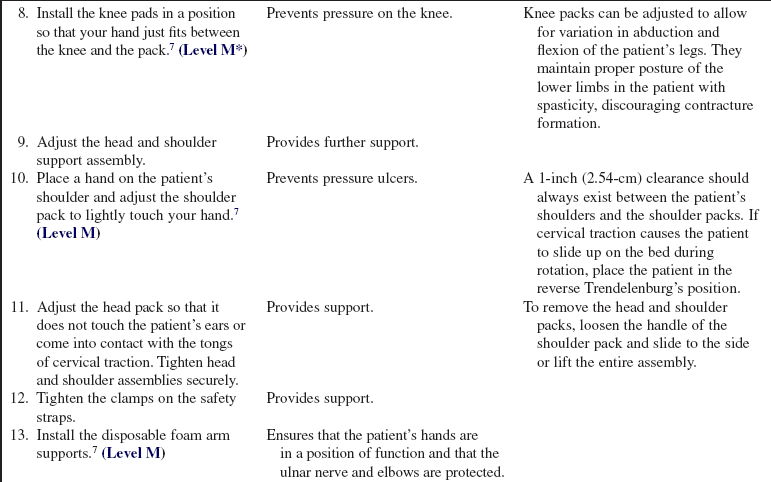
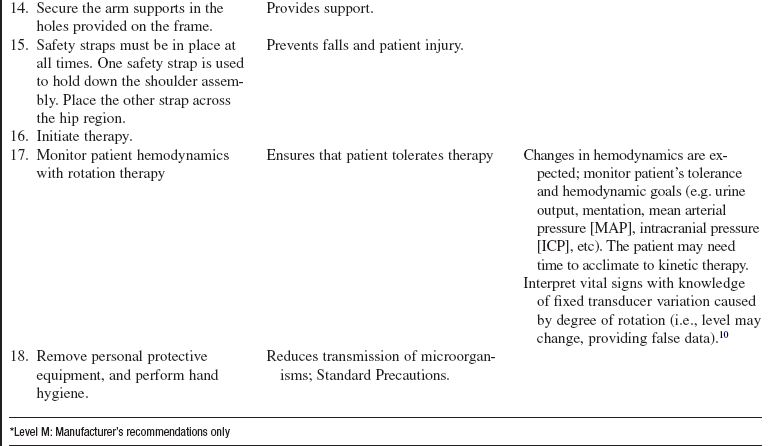
• The RotoRest™ Delta Kinetic™ Therapy bed is shown in Figure 123-1.
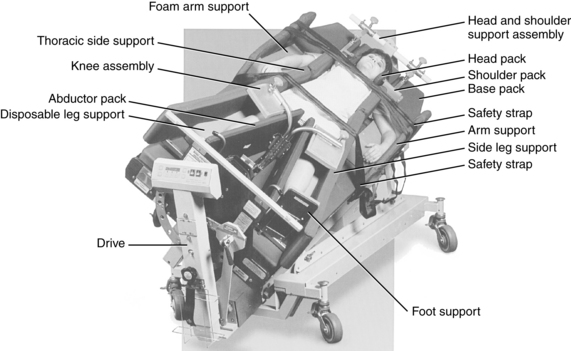
Figure 123-1 KCI RotoRest™ Delta Kinetic™ Therapy bed. (Courtesy KCI Licensing, Inc, San Antonio, TX, 2008.)
• Noted principles in caring for a patient receiving kinetic therapy on a RotoRest™ Delta Kinetic™ Therapy bed include technical and clinical competence in the following:
 The surface below the patient and the positioning packs consist of pressure-redistributing foam and a pad of nonliquid polymer gel with a low-friction, low-shear GORE medical fabric (KCI Licensing, Inc, San Antonio, Texas) cover that does not absorb body fluids.
The surface below the patient and the positioning packs consist of pressure-redistributing foam and a pad of nonliquid polymer gel with a low-friction, low-shear GORE medical fabric (KCI Licensing, Inc, San Antonio, Texas) cover that does not absorb body fluids.
 The gel pads prevent the patient from bottoming out and transfer body heat evenly; they are radiographically transparent.
The gel pads prevent the patient from bottoming out and transfer body heat evenly; they are radiographically transparent.
 The bed provides continuous, slow, side-to-side turning of the patient by rotating the bed frame. Keeping the patient in maximal rotation assists with prevention of skin breakdown and provides the most effective therapy for pulmonary indications. The bed can turn up to 62 degrees on each side, either intermittently or constantly, providing unilateral or bilateral rotation.
The bed provides continuous, slow, side-to-side turning of the patient by rotating the bed frame. Keeping the patient in maximal rotation assists with prevention of skin breakdown and provides the most effective therapy for pulmonary indications. The bed can turn up to 62 degrees on each side, either intermittently or constantly, providing unilateral or bilateral rotation.
 The amount of time the patient is held at the rotation limit before rotating in the opposite direction can be adjusted from 7 seconds to 30 minutes.
The amount of time the patient is held at the rotation limit before rotating in the opposite direction can be adjusted from 7 seconds to 30 minutes.
 Head and shoulder packs provide cervical stability but should not be used as the primary means of stabilizing cervical spine fractures. Cervical traction, halo, and vest or internal fixation may be required. Lateral arm and leg hatches facilitate range of motion.
Head and shoulder packs provide cervical stability but should not be used as the primary means of stabilizing cervical spine fractures. Cervical traction, halo, and vest or internal fixation may be required. Lateral arm and leg hatches facilitate range of motion.
 Hatches underneath the bed (located in the cervical, thoracic, and rectal areas) provide access for skin care, catheter maintenance, and bladder and bowel management. Do not open thoracic and sacral hatches at the same time.
Hatches underneath the bed (located in the cervical, thoracic, and rectal areas) provide access for skin care, catheter maintenance, and bladder and bowel management. Do not open thoracic and sacral hatches at the same time.
 The bed has a built-in scale with a maximal patient weight of 300 lbs.7
The bed has a built-in scale with a maximal patient weight of 300 lbs.7
 An optional vibrator pack is available to provide chest physiotherapy to further mobilize pulmonary secretions.
An optional vibrator pack is available to provide chest physiotherapy to further mobilize pulmonary secretions.
PATIENT AND FAMILY EDUCATION
• Explain to patient and family the adverse effects of pulmonary complications, tissue pressure, excessive moisture of the skin, and complications of immobility.  Rationale: Explanation encourages understanding when a different bed surface is needed based on the risk assessment of patient. The patient and family are able to ask questions.
Rationale: Explanation encourages understanding when a different bed surface is needed based on the risk assessment of patient. The patient and family are able to ask questions.
• Explain how CLRT and properties of the support surface achieve pressure reduction.  Rationale: Understanding and cooperation are increased.
Rationale: Understanding and cooperation are increased.
• Discuss the patient’s need for long-term pressure redistribution strategies to include redistribution of weight while in a chair or bed and management of acute or chronic health problems, chronic pressure ulcers, or both.  Rationale: The family and patient are engaged in the plan of care, and the nurse can anticipate the need for patient discharge with pressure redistribution surface.
Rationale: The family and patient are engaged in the plan of care, and the nurse can anticipate the need for patient discharge with pressure redistribution surface.
• When a support surface is used for the purpose of lateral rotation, explain how lateral rotation therapy is used to reduce the incidence of VAP and atelectasis. An added benefit is reduction of pressure on the skin.  Rationale: Understanding and cooperation are increased.
Rationale: Understanding and cooperation are increased.
• Explain to patient and family the pulmonary benefit of CLRT in promoting dynamic movement of pulmonary secretions.  Rationale: Understanding of the role of pulmonary secretion mobility in the critically ill is encouraged.
Rationale: Understanding of the role of pulmonary secretion mobility in the critically ill is encouraged.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s risk for a pressure ulcer with an evidence-based practice assessment tool (i.e., Braden score).1,2  Rationale: Valid assessment tools assist in identification of patient risk for alterations in skin.
Rationale: Valid assessment tools assist in identification of patient risk for alterations in skin.
• Assess the patient’s skin for evidence of pressure ulcer formation or alterations in skin on admission and throughout care based on institutional policy.  Rationale: Baseline and ongoing skin status data are provided.
Rationale: Baseline and ongoing skin status data are provided.
• Assess the patient’s wounds: location, size, stage of pressure ulcer, description of tissue in wound bed, type and amount of drainage, surrounding skin for maceration and inflammation, and pain on palpation of surrounding skin.  Rationale: Objective and thorough assessment of wounds on admission and throughout course of illness is necessary for measuring effectiveness of therapy and interventions.
Rationale: Objective and thorough assessment of wounds on admission and throughout course of illness is necessary for measuring effectiveness of therapy and interventions.
• Assess the patient’s vascular system: ensure hemodynamic stability is present, and assess for presence of edema in lower extremities and deep vein thrombosis (DVT) potential.14  Rationale: Baseline data are provided to measure and treat the ill effects of immobility.
Rationale: Baseline data are provided to measure and treat the ill effects of immobility.
• Assess the patient’s pulmonary status to include the quality and presence of adventitious breath sounds, the rate and depth of respirations, cough, cyanosis, dyspnea, nasal flaring, arterial blood gas results, chest radiograph, mental status, and restlessness.  Rationale: Initial and ongoing evaluation of effectiveness of CLRT therapy on body systems is provided. Lateral movement provides postural drainage, mobilizes secretions, and enhances air exchange.5
Rationale: Initial and ongoing evaluation of effectiveness of CLRT therapy on body systems is provided. Lateral movement provides postural drainage, mobilizes secretions, and enhances air exchange.5
• Assess the patient’s bladder for complications associated with urinary stasis from immobility to include the presence of bladder distention, incomplete bladder emptying, or urinary infrequency.  Rationale: Baseline data are provided before implementation of lateral movement that decreases urinary stasis and associated complications.14
Rationale: Baseline data are provided before implementation of lateral movement that decreases urinary stasis and associated complications.14
• Discuss goals for pressure redistribution and CLRT therapy with prescribing provider.  Rationale: The properties of the CLRT support surface are evaluated to match patient factors related to type of injury, moisture, and need for redistribution of pressure on skin and wounds.
Rationale: The properties of the CLRT support surface are evaluated to match patient factors related to type of injury, moisture, and need for redistribution of pressure on skin and wounds.
Patient Preparation
• Ensure that the patient and family understand preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught clinical information and rationale is evaluated and reinforced.
Rationale: Understanding of previously taught clinical information and rationale is evaluated and reinforced.
• Evaluate the properties of support surface to meet pulmonary needs, skin factors related to type of injury, moisture, and need for redistribution of pressure on skin and wounds. Order and inspect the bed functions before the patient is placed on the surface  Rationale: Support surface selection should match clinical indication for patient therapy. Relief of external pressure may decrease risk of pressure ulcer formation and facilitates wound healing.
Rationale: Support surface selection should match clinical indication for patient therapy. Relief of external pressure may decrease risk of pressure ulcer formation and facilitates wound healing.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Organize moving the patient to the special surface, ensuring adequate personnel are available. Assist the patient to a supine position with the head of the bed elevated to 30 degrees (if not medically contraindicated) in preparation for move to specialty bed.  Rationale: Transfer of the patient from one bed to another is potentiated. Head of bed at 30 degrees minimizes shearing forces and protects airway.
Rationale: Transfer of the patient from one bed to another is potentiated. Head of bed at 30 degrees minimizes shearing forces and protects airway.
References
1. Ayello, EA, Lyder, CH, Protecting patients from harm. -preventing pressure ulcers in hospital patients. Nursing. 2007; 37(10):36–40.
![]() 2. Braden, BJ, Bergstrom, N. Clinical utility of the Braden scale for predicting pressure sore risk. Decubitus. 1989; 2(3):44–46,50-41.
2. Braden, BJ, Bergstrom, N. Clinical utility of the Braden scale for predicting pressure sore risk. Decubitus. 1989; 2(3):44–46,50-41.
![]() 3. Bernard, GR, Acute Respiratory distress syndrome. a -historical perspective. Am J Respir Crit Care Med 2005; 172:798–802.
3. Bernard, GR, Acute Respiratory distress syndrome. a -historical perspective. Am J Respir Crit Care Med 2005; 172:798–802.
![]() 4. Brienza, DM, Geyer, J. Using support surfaces to manage tissue integrity. Adv Skin Wound Care. 2005; 18(3):151–157.
4. Brienza, DM, Geyer, J. Using support surfaces to manage tissue integrity. Adv Skin Wound Care. 2005; 18(3):151–157.
5. Goldhill, DR, Imhoff, M, McLean, B, et al, Rotational bed therapy to prevent and treat respiratory complications. a -review and meta-analysis. Am J Crit Care. 2007; 16(1):50–62.
![]() 6. Higgens Martin, A. Should continuous lateral rotation therapy replace manual turning. Nurs Manage. 2001; 32(8):41–45.
6. Higgens Martin, A. Should continuous lateral rotation therapy replace manual turning. Nurs Manage. 2001; 32(8):41–45.
![]() 7. Kinetic, Concepts, Roto-Rest Delta. operations and maintenance manual. Kinetic Concepts, San Antonio, 1995.
7. Kinetic, Concepts, Roto-Rest Delta. operations and maintenance manual. Kinetic Concepts, San Antonio, 1995.
![]() 8. Maklebust, J. Choosing the right support surface. Adv Skin Wound Care. 2005; 18(3):158–160.
8. Maklebust, J. Choosing the right support surface. Adv Skin Wound Care. 2005; 18(3):158–160.
9. National Pressure Ulcer Advisory Panel, Support surface standards initiative. terms and definitions related to -support surfaces,. www.npuap.org/npuap_S31_TD, 2007 [retrieved August 28, 2009, from].
10. Rauen, CA, Makic, MB, Bridges, E, Evidence-based practice habits. transforming research into bedside practice. Crit Care Nurse. 2009; 29(2):46–59.
![]() 11. Russell, T, Logsdon, A, Pressure ulcers and lateral rotation beds. a case study. J Wound Ostomy Continence Nurs. 2003; 30(3):143–145.
11. Russell, T, Logsdon, A, Pressure ulcers and lateral rotation beds. a case study. J Wound Ostomy Continence Nurs. 2003; 30(3):143–145.
12. Thompson, P, Anderson, J, Langeo, D, et al, Support surfaces. definitions and utilization for patient care. Adv Skin Wound Care. 2008; 21(6):264–266.
13. Turpin, P, Pemberton, V, Prevention of pressure ulcers in patients being managed on CLRT. is supplemental repositioning needed. J Wound Ostomy Continence Nurs. 2006; 33(4):381–388.
![]() 14. Washington, GT, Macness, CL, Evaluation of outcomes. the effects of continuous lateral rotation therapy. J Nurse Care Qual. 2005; 20(3):273–282.
14. Washington, GT, Macness, CL, Evaluation of outcomes. the effects of continuous lateral rotation therapy. J Nurse Care Qual. 2005; 20(3):273–282.
Anderson, J, Hanson, D, Langeo, D, et al. The evolution of support surfaces. Adv Skin Wound Care. 2006; 19(3):130–132.
Agency for Health Care Policy and Research (AHCPR), Pressure ulcers in adults. prediction and prevention,. US Department of Health and Human Services, Rockville, MD, 1992. [AHCPR Publication 92-0047].
Agency for Health Care Policy and Research (AHCPR). Treatment of pressure ulcers. Rockville, MD: US Department of Health and Human Services; 1994. [AHCPR Publication 95-0652].
National Pressure Ulcer Advisory Panel. www.npuap.org, September 2, 2009 [Accessed].