Procedure 12 Cervical Spine
Lateral Mass Screw Fixation
Indications
 Destruction of bony anatomy secondary to neoplasm
Destruction of bony anatomy secondary to neoplasm
 Stabilization after multisegment anterior decompression and fusion (long anterior fusions for tumor, infection, ankylosing spondylitis, diffuse cervical spondylosis)
Stabilization after multisegment anterior decompression and fusion (long anterior fusions for tumor, infection, ankylosing spondylitis, diffuse cervical spondylosis)
Examination/Imaging
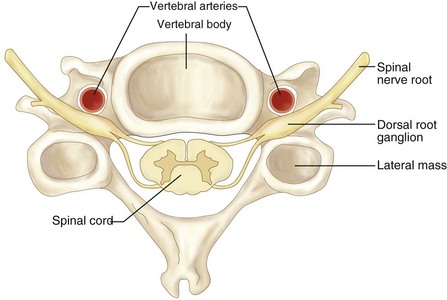
Surgical Anatomy (Figure 12-2)
 Nerve root injury may occur if the screw trajectory is incorrect, if the screw penetration is too deep (bicortical screw purchase), or if there is significant past pointing of the drill.
Nerve root injury may occur if the screw trajectory is incorrect, if the screw penetration is too deep (bicortical screw purchase), or if there is significant past pointing of the drill.
 Vertebral artery injury is an exceedingly rare complication that may occur if the trajectory is medial and the screw penetration is too deep.
Vertebral artery injury is an exceedingly rare complication that may occur if the trajectory is medial and the screw penetration is too deep.
 If brisk, pulsatile arterial bleeding is encountered from the drill hole, hemostasis should be obtained using bone wax, thrombogenic agents, and, potentially, placement of a screw in the hole. Postoperative angiography should be obtained to determine the status of the injured vertebral artery.
If brisk, pulsatile arterial bleeding is encountered from the drill hole, hemostasis should be obtained using bone wax, thrombogenic agents, and, potentially, placement of a screw in the hole. Postoperative angiography should be obtained to determine the status of the injured vertebral artery.
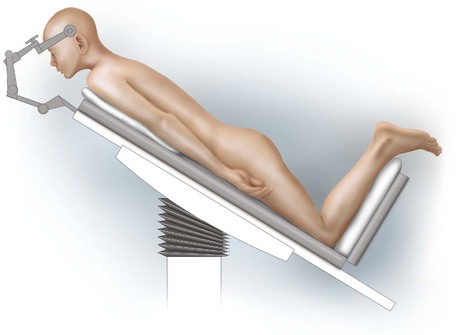
Positioning
 Mayfield tongs are applied, rigidly fixing the head to the table in the prone position (Figures 12-3 and 12-4).
Mayfield tongs are applied, rigidly fixing the head to the table in the prone position (Figures 12-3 and 12-4).
 The neck is slightly extended. If this compromises spinal canal patency to a detrimental degree, lordosis may be obtained following decompression by having an unscrubbed assistant readjust the head holder to improve cervical lordosis.
The neck is slightly extended. If this compromises spinal canal patency to a detrimental degree, lordosis may be obtained following decompression by having an unscrubbed assistant readjust the head holder to improve cervical lordosis.
 The arms and elbows are placed adjacent to the torso and are well padded to prevent pressure ulcers.
The arms and elbows are placed adjacent to the torso and are well padded to prevent pressure ulcers.
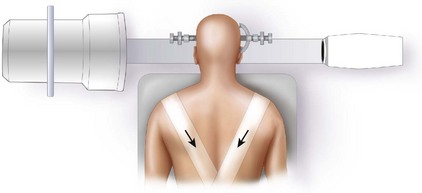
 The shoulders are gently pulled caudad by adhesive tape.
The shoulders are gently pulled caudad by adhesive tape.
 The knees are flexed to prevent distal migration of patient.
The knees are flexed to prevent distal migration of patient.
Portals/Exposures
 A midline vertical skin incision can be made (as necessary) extending from the occipital protuberance past the spinous process of the seventh cervical vertebra (typically the most superficially prominent vertebra).
A midline vertical skin incision can be made (as necessary) extending from the occipital protuberance past the spinous process of the seventh cervical vertebra (typically the most superficially prominent vertebra).
 The nuchal ligament is divided in the midline and incised as far as the tips of the spinous processes.
The nuchal ligament is divided in the midline and incised as far as the tips of the spinous processes.
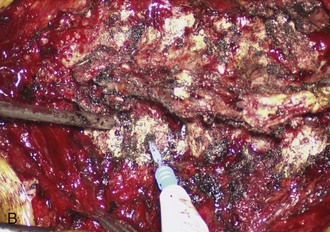
 The deep muscle layer is stripped off the spinous processes close to the bone with the aid of electrocautery (Figure 12-5, A and B).
The deep muscle layer is stripped off the spinous processes close to the bone with the aid of electrocautery (Figure 12-5, A and B).
 Subperiosteal dissection is carried to the lateral boundary of the articular masses.
Subperiosteal dissection is carried to the lateral boundary of the articular masses.
Procedure
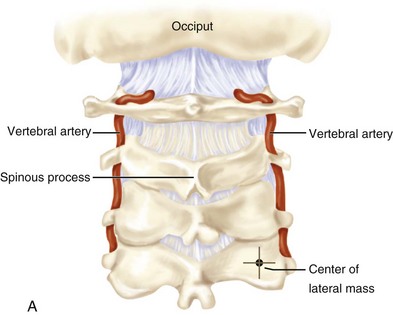
Step 1: Determining the Entry Point
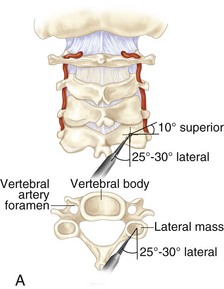
 The entry point for screw insertion is located 1 mm medial to the midpoint of the lateral mass. The direction of the screw is 15 degrees cephalad and 30 degrees lateral for C3-6 (Figure 12-6, A).
The entry point for screw insertion is located 1 mm medial to the midpoint of the lateral mass. The direction of the screw is 15 degrees cephalad and 30 degrees lateral for C3-6 (Figure 12-6, A).
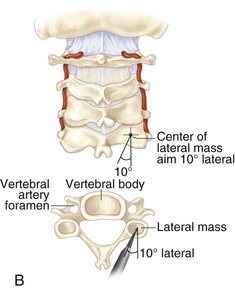
Step 1 Controversies
• The Roy-Camille technique may be used for screw entry point (see Figure 12-6, B). The starting point for the screw insertion is located at the midpoint of the lateral mass. The screw is directed 10 degrees lateral with no cranial-caudal inclination. This technique may lead to cephalad articular joint violation.
Step 2: Drilling the Screw Hole
 Holes are drilled with a 2.4-mm drill bit using the drill guide.
Holes are drilled with a 2.4-mm drill bit using the drill guide.
 The drill depth can be increased in 2-mm increments.
The drill depth can be increased in 2-mm increments.
 A depth gauge is used to confirm the appropriate screw length.
A depth gauge is used to confirm the appropriate screw length.
Step 2 Pitfalls
• Past pointing of the drill may result in nerve root irritation.
• Improper drill trajectory may result in injury to the spinal cord or vertebral artery.
• Drill trajectories in the sagittal plane that are too low may violate the facet joint.
• Drill trajectories that are too medial may encroach upon the vertebral artery.
Step 3: Tapping and Screw Insertion
 The tap size may equal the outer screw diameter or be slightly undersized. A self-tapping screw may avoid the need for additional tapping.
The tap size may equal the outer screw diameter or be slightly undersized. A self-tapping screw may avoid the need for additional tapping.
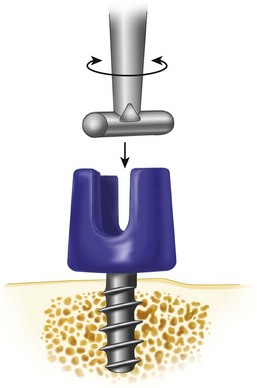
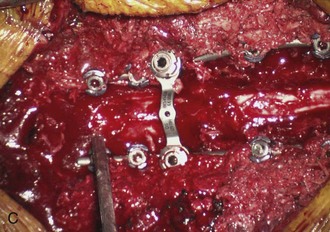
 An appropriate-size screw is then placed in the same trajectory as the tap (Figure 12-7).
An appropriate-size screw is then placed in the same trajectory as the tap (Figure 12-7).
Step 4: Rod Insertion
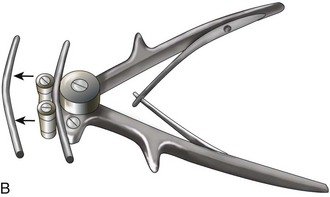
 The determined length of rod is cut using the rod cutter (Figure 12-8, A) and bent utilizing the rod bender (Figure 12-8, B).
The determined length of rod is cut using the rod cutter (Figure 12-8, A) and bent utilizing the rod bender (Figure 12-8, B).
 Contouring of the rod is performed in gentle, limited steps until the desired shape is achieved (Figure 12-8, C).
Contouring of the rod is performed in gentle, limited steps until the desired shape is achieved (Figure 12-8, C).
Step 4 Pearls
• In extended and complex instrumented fusions, additional stability can be achieved by linking cross connectors to the longitudinal rods.
• In patients with poor bone quality unsuitable for placement of lateral mass screws, sublaminar wires can be secured to open cable connectors attached to the rods for additional fixation.
Step 5: Placement of Screw Caps
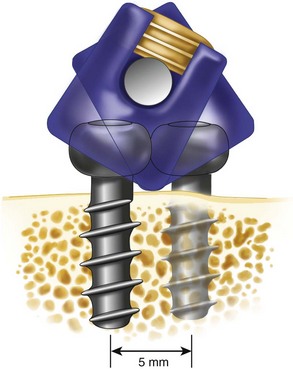
 Screw tightening (once the inner nut is placed in the polyaxial screw head) should be performed in a gentle and systematic fashion to facilitate rod seating, allow controlled manipulation of the spinal segments, and to avoid screw torque, which may result in screw loosening (Figure 12-9).
Screw tightening (once the inner nut is placed in the polyaxial screw head) should be performed in a gentle and systematic fashion to facilitate rod seating, allow controlled manipulation of the spinal segments, and to avoid screw torque, which may result in screw loosening (Figure 12-9).
 Final nut tightening is performed utilizing the torque driver and antitorque device to guarantee optimal tightening of the nuts and to avoid late rod loosening.
Final nut tightening is performed utilizing the torque driver and antitorque device to guarantee optimal tightening of the nuts and to avoid late rod loosening.
Postoperative Care and Expected Outcomes
 Depending on the length and extent of the entire surgical procedure, the pathology, and bone quality, the required postoperative care may differ significantly (Figure 12-10).
Depending on the length and extent of the entire surgical procedure, the pathology, and bone quality, the required postoperative care may differ significantly (Figure 12-10).
 Patients are routinely monitored in the hospital overnight.
Patients are routinely monitored in the hospital overnight.
 A soft collar orthosis may be used in the setting of short segment reconstructions in degenerative disease. A hard collar is may be applied in the postoperative period for approximately 6 weeks, depending upon the pathology and length of the instrumented construct. Rigid external fixation with a halo-vest orthosis is rarely indicated, except in severe osteoporosis, questionable compliance, neoplasms, and certain traumatic lesions.
A soft collar orthosis may be used in the setting of short segment reconstructions in degenerative disease. A hard collar is may be applied in the postoperative period for approximately 6 weeks, depending upon the pathology and length of the instrumented construct. Rigid external fixation with a halo-vest orthosis is rarely indicated, except in severe osteoporosis, questionable compliance, neoplasms, and certain traumatic lesions.
 Deep or superficial wound infections should be addressed at an early stage. Extensive infections may require hardware removal and rigid external immobilization.
Deep or superficial wound infections should be addressed at an early stage. Extensive infections may require hardware removal and rigid external immobilization.
 Postoperative neurologic deterioration resulting from hardware malpositioning requires hardware revision or removal.
Postoperative neurologic deterioration resulting from hardware malpositioning requires hardware revision or removal.
 Failure of bony fusion may result in instrumentation failure, necessitating hardware revision.
Failure of bony fusion may result in instrumentation failure, necessitating hardware revision.
Bayley E, Zia Z, Kerslake R, Klezl Z, Boszczyk BM. Lamina-guided lateral mass screw placement in the sub-axial cervical spine. Eur Spine J. 2010;19:660-664.
Deen GH, Birch BD, Wharen RE, Reimer R. Lateral mass screw-rod fixation of the cervical spine: a prospective clinical series with 1-year follow-up. Spine J. 2003;3:489-495.
Merrola AA, Castro BA, Alongi PR. Anatomic consideration for standard and modified techniques of cervical lateral mass screw placement. Spine J. 2002;2:430-435.
Wang MY, Levi AD. Minimally invasive lateral mass screw fixation in the cervical spine; initial clinical experience with long-term follow-up. Neurosurgery. 2006;58:907-912.
Xu R, Haman SP, Ebraheim NA, Yeasting RA. The anatomic relation of lateral mass screws to the spinal nerves: a comparison of the Magerl, Anderson, and An techniques. Spine. 1999;24:2057-2061.