Peritoneal Dialysis
PREREQUISITE NURSING KNOWLEDGE
• Peritoneal dialysis (PD) works on the principles of diffusion and osmosis; thus, a basic knowledge of these concepts is necessary.
 Diffusion is the passive movement of solutes through a semipermeable membrane from an area of higher concentration to one of lower concentration. When this concept is applied to peritoneal dialysis, diffusion occurs because the patient’s blood contains waste products (solute), which give it a higher osmolarity (concentration) than the dialysate. So, waste products in the blood diffuse across the semipermeable membrane into the dialysate solution.
Diffusion is the passive movement of solutes through a semipermeable membrane from an area of higher concentration to one of lower concentration. When this concept is applied to peritoneal dialysis, diffusion occurs because the patient’s blood contains waste products (solute), which give it a higher osmolarity (concentration) than the dialysate. So, waste products in the blood diffuse across the semipermeable membrane into the dialysate solution.
 Osmosis is the passive movement of solvent through a semipermeable membrane from an area of lower concentration to one of higher concentration. The dextrose added to the dialysate gives it a higher osmotic gradient than that of the patient’s blood. So, excess water in the blood is pulled into the dialysate via osmosis.
Osmosis is the passive movement of solvent through a semipermeable membrane from an area of lower concentration to one of higher concentration. The dextrose added to the dialysate gives it a higher osmotic gradient than that of the patient’s blood. So, excess water in the blood is pulled into the dialysate via osmosis.
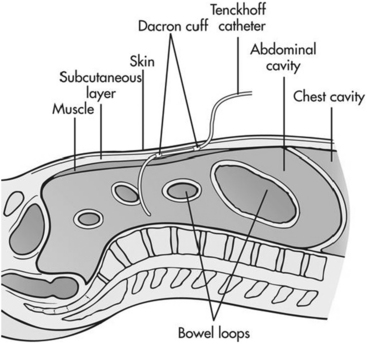
• PD uses the peritoneal membrane as the semipermeable membrane for both fluid and solutes.4,10,14
• Sterile dialysis fluid (dialysate) is infused into the peritoneal cavity of the abdomen through a flexible catheter (Fig. 114-1).
• A small-framed adult can usually tolerate 2 to 2.5 L of dialysate, whereas a large-framed adult may be able to tolerate up to 3 L in the abdominal cavity. The larger the volume of dialysate, the more effective the removal of blood urea nitrogen (BUN) and creatinine6,9,11; however, peritoneal clearance may be improved with more frequent exchange rather than an increase in the exchange volume.5 The most limiting factor of the volume of dialysate is that it may cause direct pressure on the diaphragm and cause a compromise of respiratory excursion.4,14,15 The PD dialysate contains higher concentrations of glucose than normal serum levels. These higher concentrations aid in the removal of water via osmosis and small-to-middle-weight molecules (urea, creatinine) via diffusion. Several concentrations of glucose are available in commercially prepared dialysate solutions. The higher the concentration of glucose in the dialysate, the greater the amount of fluid removal. Icodextrin, a relatively new alternative to glucose solutions, may be used as the osmotic agent. This glucose polymer is metabolized to maltose and is not readily absorbed.6,8,12,13
• PD involves repeated fluid exchanges or cycles. Each cycle has three phases: instillation, dwell, and drain.
 During the instillation phase, the dialysate is infused via gravity into the patient’s peritoneal cavity through a peritoneal catheter.1,2,12
During the instillation phase, the dialysate is infused via gravity into the patient’s peritoneal cavity through a peritoneal catheter.1,2,12
 During the dwell phase, the dialysate remains in the patient’s peritoneal cavity, allowing osmosis and diffusion to occur. Dwell time varies based on the patient’s clinical need.
During the dwell phase, the dialysate remains in the patient’s peritoneal cavity, allowing osmosis and diffusion to occur. Dwell time varies based on the patient’s clinical need.
 During the drain phase, the dialysate and excess extracellular fluid, wastes, and electrolytes are drained via gravity from the peritoneal cavity via the catheter.
During the drain phase, the dialysate and excess extracellular fluid, wastes, and electrolytes are drained via gravity from the peritoneal cavity via the catheter.
• PD can be performed either manually with a dialysis administration set with a drainage bag or with a cycler machine (Fig. 114-2). With a cycler machine, multiple exchanges are programmed into the machine and run automatically. Cycler machines are infrequently found in the hospital setting but are often used by outpatients for evening and night exchanges.
• PD catheters can become clogged with the build-up of fibrin. Heparin is sometimes added to the dialysate or used as a separate flush to prevent occlusion.1,4,9,14,15
• PD dialysate should be warmed to the appropriate temperature in a commercial warmer. Never warm the solution in a standard microwave oven, which heats unevenly and does not regulate the fluid temperature.14,15
• After each cycle of PD, assess the patient’s vital signs, fluid balance, and any signs of infection and communicate abnormal findings to the physician.
• The adequacy of dialysis and assessment of the patient’s residual renal function should be evaluated on a periodic basis. Adequacy of dialysis can be measured with urea kinetic modeling (Kt/V) or urea clearance.6,11 Residual renal functioning can be monitored with urine creatinine clearance. Collaboration with the nephrology team is necessary to monitor these parameters.
EQUIPMENT
• Goggles or fluid shield face masks
• Sterile and nonsterile gloves
Additional equipment, to have available depending on patient need, includes the following:
Additional equipment for initiation of PD includes the following:
Additional equipment for termination of PD includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the purpose of PD.  Rationale: PD is necessary to perform the physiologic functions of the kidneys when renal failure is present. PD uses the lining inside the abdomen, called the peritoneal cavity, as a filter to clean the blood and remove excess fluid.
Rationale: PD is necessary to perform the physiologic functions of the kidneys when renal failure is present. PD uses the lining inside the abdomen, called the peritoneal cavity, as a filter to clean the blood and remove excess fluid.
• Explain the procedure and review any questions.  Rationale: Explanation provides information and may decrease patient anxiety.
Rationale: Explanation provides information and may decrease patient anxiety.
• Explain the need for careful sterile technique when the abdominal catheter is accessed.  Rationale: Sterile technique is used to decrease the chance of peritoneal infection because pathogens can be introduced into the abdominal cavity via the catheter.
Rationale: Sterile technique is used to decrease the chance of peritoneal infection because pathogens can be introduced into the abdominal cavity via the catheter.
• Explain the three phases of PD.  Rationale: Because each phase is different, the patient must be informed of all three phases and the purposes, interventions, and possible complications of each.
Rationale: Because each phase is different, the patient must be informed of all three phases and the purposes, interventions, and possible complications of each.
• Explain the potential for feelings of fullness and possibly shortness of breath during the dwell phase.  Rationale: The pressure of the dialysate fluid on the diaphragm may cause the patient to have these feelings, which are normal for the dwell phase.
Rationale: The pressure of the dialysate fluid on the diaphragm may cause the patient to have these feelings, which are normal for the dwell phase.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
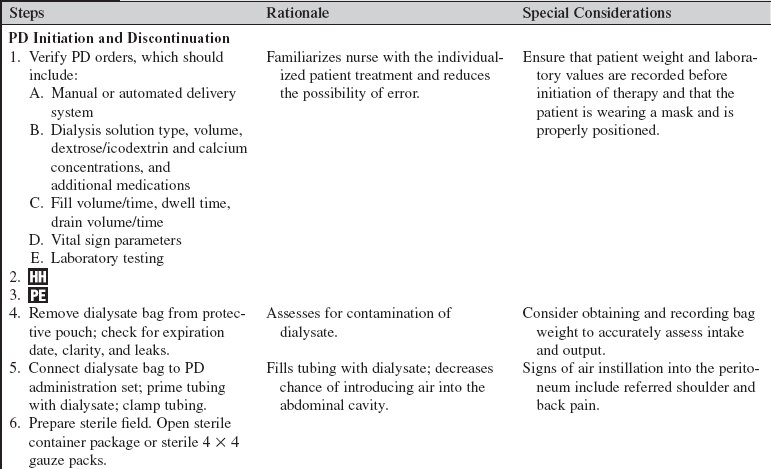
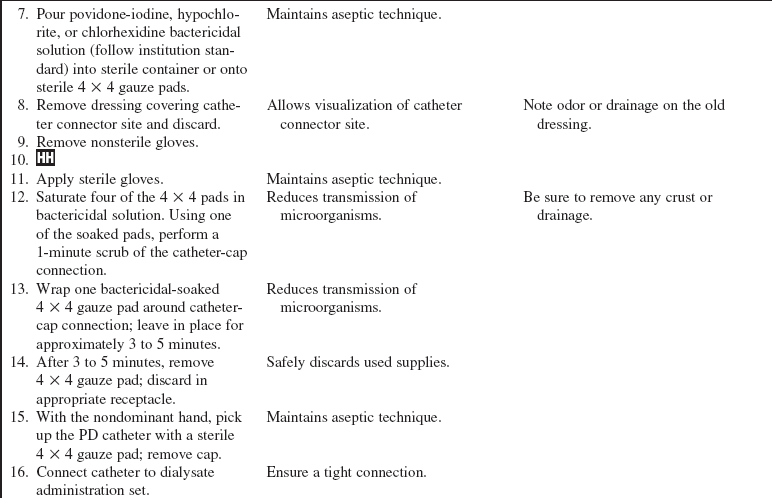
• Obtain baseline vital signs, respiratory status, abdominal assessment, blood glucose level, and pertinent laboratory results (potassium, sodium, calcium, phosphorus, magnesium, renal function tests, complete blood count).  Rationale: Patients in renal failure often have altered baseline assessments, according to both physical assessment and laboratory values. The availability of this information before treatments are started is helpful so that interventions, including the type and amount of dialysate fluid, can be individualized.
Rationale: Patients in renal failure often have altered baseline assessments, according to both physical assessment and laboratory values. The availability of this information before treatments are started is helpful so that interventions, including the type and amount of dialysate fluid, can be individualized.
• Assess volume status, as indicated by the following:
 Rationale: PD is often initiated for the control of hypervolemia.9 Knowledge of a patient’s pretreatment volume status is essential to allow for the individualization of treatment goals and interventions.
Rationale: PD is often initiated for the control of hypervolemia.9 Knowledge of a patient’s pretreatment volume status is essential to allow for the individualization of treatment goals and interventions.
• Assess PD catheter and abdominal exit site for signs and symptoms of infection, leakage or drainage, or signs and symptoms of peritonitis3,6–9,15:
 Cloudy or bloody dialysate solution
Cloudy or bloody dialysate solution
 Subcutaneous fluid in abdomen, groin, or upper thighs
Subcutaneous fluid in abdomen, groin, or upper thighs
 Rationale: The catheter insertion site provides a portal of entry for infection that can result in septicemia or peritonitis. If the insertion site or effluent appears to be infected, further interventions (e.g., site change, culture, antibiotics) may be necessary.
Rationale: The catheter insertion site provides a portal of entry for infection that can result in septicemia or peritonitis. If the insertion site or effluent appears to be infected, further interventions (e.g., site change, culture, antibiotics) may be necessary.
• Check peritoneal catheter and tubing for kinks, puncture sites, and loose connections.  Rationale: Adequate flow is essential for optimal treatment. A dysfunctional catheter can alter outcomes.
Rationale: Adequate flow is essential for optimal treatment. A dysfunctional catheter can alter outcomes.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Assist the patient in applying a mask.  Rationale: The risk for airborne and nasal pathogens is decreased.
Rationale: The risk for airborne and nasal pathogens is decreased.
• Reposition patient to a comfortable position.  Rationale: Proper positioning is important to ensure patient comfort, optimize respiratory status, and facilitate optimal flow through the abdominal catheter.
Rationale: Proper positioning is important to ensure patient comfort, optimize respiratory status, and facilitate optimal flow through the abdominal catheter.
References
![]() 1. Ash, SR, Chronic peritoneal dialysis catheters. procedures for placement, maintenance and removal. Semin Nephrol 2002; 22:221–236.
1. Ash, SR, Chronic peritoneal dialysis catheters. procedures for placement, maintenance and removal. Semin Nephrol 2002; 22:221–236.
2. Ash, SR, Chronic peritoneal dialysis catheters. challenges and design solutions. Int J Artif Organs 2006; 29:85–94.
![]() 3. Bernardini, J, et al. Randomized, double-blind trial of antibiotic exit site cream for prevention of exit site infection in peritoneal dialysis patients. J Am Soc Nephrol. 2005; 16:539–545.
3. Bernardini, J, et al. Randomized, double-blind trial of antibiotic exit site cream for prevention of exit site infection in peritoneal dialysis patients. J Am Soc Nephrol. 2005; 16:539–545.
![]() 4. Burrows-Hudson S, Prowant, B. Nephrology nursing standards of practice and guidelines for care,. Pitman, NJ: American Nephrology Nurses’ Association; 2005.
4. Burrows-Hudson S, Prowant, B. Nephrology nursing standards of practice and guidelines for care,. Pitman, NJ: American Nephrology Nurses’ Association; 2005.
![]() 5. Churchill, DN. Impact of peritoneal dialysis dose guidelines on clinical outcomes. Perit Dial Int. 2005; 25:S95–S98.
5. Churchill, DN. Impact of peritoneal dialysis dose guidelines on clinical outcomes. Perit Dial Int. 2005; 25:S95–S98.
6. Crabtree, JH. Rescue and salvage procedures for mechanical and infectious complications of peritoneal dialysis. Int J Artif Organs. 2006; 29:67–84.
7. Diaz-Buxo JA. Complications of peritoneal catheters: early and late. Int J Artificial Organs. 2006; 29:50–58.
8. Goffin, E. Aseptic peritonitis and icodextrin. Perit Dial Int. 2006; 26:314–316.
9. Luongo, M, Biel, L. Peritoneal dialysis in the acute care setting. In: Counts C, ed. Core curriculum for -nephrology nursing,. ed 5. Pitman, NJ: American Nephrology Nurses’ Association; 2008:215–230.
10. McIntyre, CS. Update on peritoneal dialysis solutions. Kidney Int. 2007; 71:486–490.
11. National Kidney Foundation (NKF), KDOQI clinical practice guidelines for vascular access. update 2006. Am J Kidney Dis 2006; 48:S176–S307.
12. Negoi, D, et al. Current trends in the use of peritoneal dialysis catheters. Adv Perit Dial. 2006; 22:147–152.
13. Piraino, B. Peritoneal Dialysis infections recommendations [review]. Contrib Nephrol. 2006; 150:181–186.
14. Prowant, BF, et al, Peritoneal dialysis Counts CS, ed.. Core curriculum for nephrology nursing. ed 5. American Nephrology Nurses’ Association, Pitman, NJ, 2008:657–681.
15. Wild, J. Peritioneal dialysis. In: Thomas N, ed. Renal nursing. ed 3. Edinburg: Ballierre Tindall; 2008:223–275.
Chin, AI, Yeun, JY, Encapsulating peritoneal sclerosis. an -unpredictable and devastating complication of peritoneal dialysis. Am J Kidney Dis 2006; 47:697–712.
![]() Crabtree, JH, et al, Optimal peritoneal dialysis catheter type and exit site location. an anthropometric analysis. ASAIO J 2005; 51:743–747.
Crabtree, JH, et al, Optimal peritoneal dialysis catheter type and exit site location. an anthropometric analysis. ASAIO J 2005; 51:743–747.
![]() Erixon, M, et al, Take care in how you store your PD fluids. actual temperature determines the balance between -reactive and non-reactive GDPs. Perit Dial Int 2005; 25:583–590.
Erixon, M, et al, Take care in how you store your PD fluids. actual temperature determines the balance between -reactive and non-reactive GDPs. Perit Dial Int 2005; 25:583–590.
Scanziani, R, et al. Imaging work-up for peritoneal access care and peritoneal dialysis complications. Int J Artif Organs. 2006; 29:142–152.