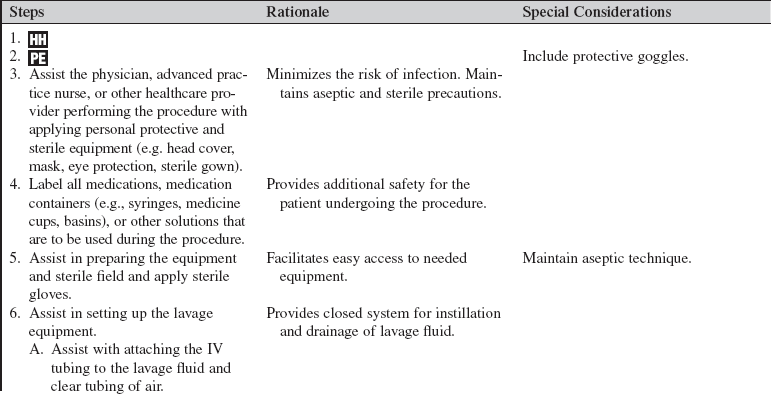
Peritoneal Lavage (Assist)
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the abdomen is needed.
• The Intestines and the bladder lie immediately beneath the abdominal surface. In children, the bladder is an abdominal organ. In adults, a full bladder is raised out of the pelvis.
• The cecum is relatively fixed and is much less mobile than the sigmoid colon; therefore, bowel perforations are more frequent in the right lower quadrant than in the left.
• A distended stomach can extend to the anterior abdominal wall.
• Peritoneal fluid is normally straw-colored, serous fluid secreted by the cells of the peritoneum.
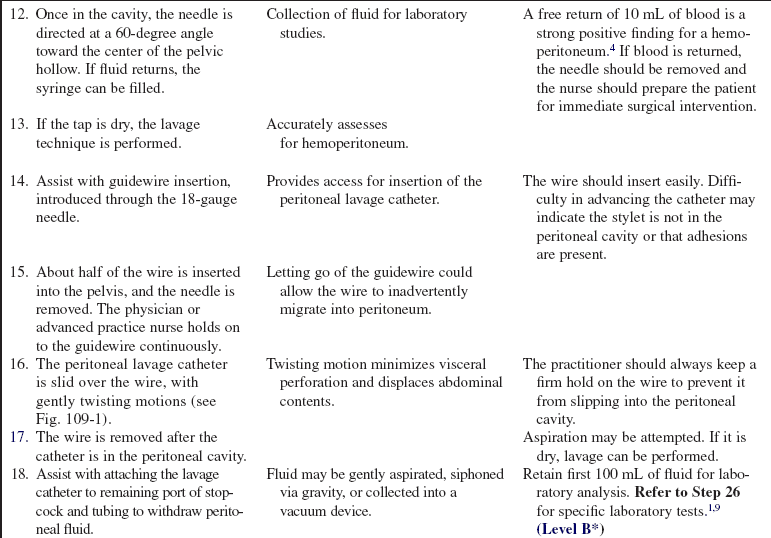
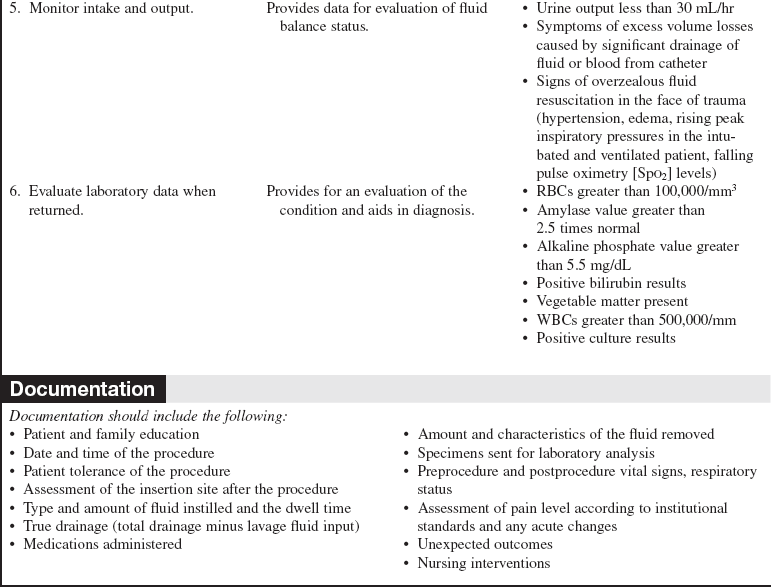
• Grossly bloody fluid, a red blood cell (RBC) count of greater than 100,000/mm3,2,5,9 and the presence of bacteria or bile in the return fluid in the abdomen are abnormal. A white blood cell (WBC) count greater than 500,000/mm and the presence of bile or amylase in the lavage fluid are parameters, in addition to the RBC count, that can lead to operative intervention.2,5,9
• Diagnostic peritoneal lavage is a highly sensitive tool for diagnosis of visceral injuries in the abdominal cavity.1,5,8
• Diagnostic peritoneal lavage is used after blunt abdominal trauma or in trauma patients with head injuries, those who are unconscious, or those with preexisting paraplegia to determine the presence of the following2:
 Hemoperitoneum (blood in lavage returns)
Hemoperitoneum (blood in lavage returns)
 Organ injury (intestinal enzymes or microorganisms in lavage returns)
Organ injury (intestinal enzymes or microorganisms in lavage returns)
• Therapeutic lavage is used to:
 Irrigate and cleanse purulent exudate in patients with peritonitis or intraabdominal abscess
Irrigate and cleanse purulent exudate in patients with peritonitis or intraabdominal abscess
 Warm the abdominal cavity in patients with hypothermia
Warm the abdominal cavity in patients with hypothermia
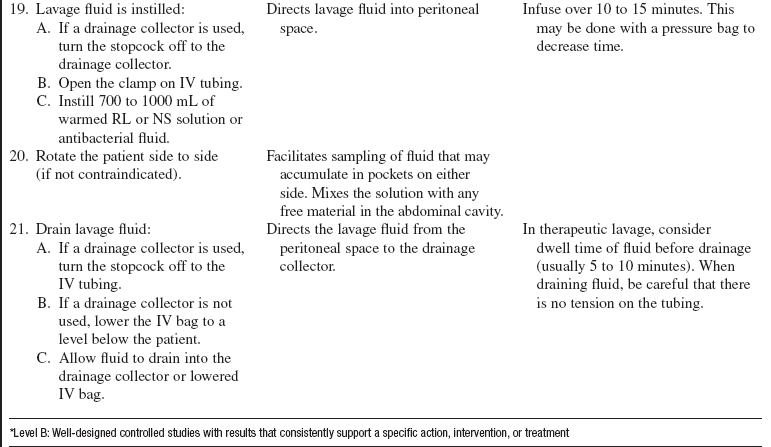
 Remove unwanted or toxic chemicals through peritoneal dialysis
Remove unwanted or toxic chemicals through peritoneal dialysis
• For trauma patients with stab wounds and gunshot wounds to the lower chest or anterior abdomen, diagnostic peritoneal lavage is controversial; most trauma centers operate on patients with gunshot wound injuries to the lower chest or anterior abdomen.1
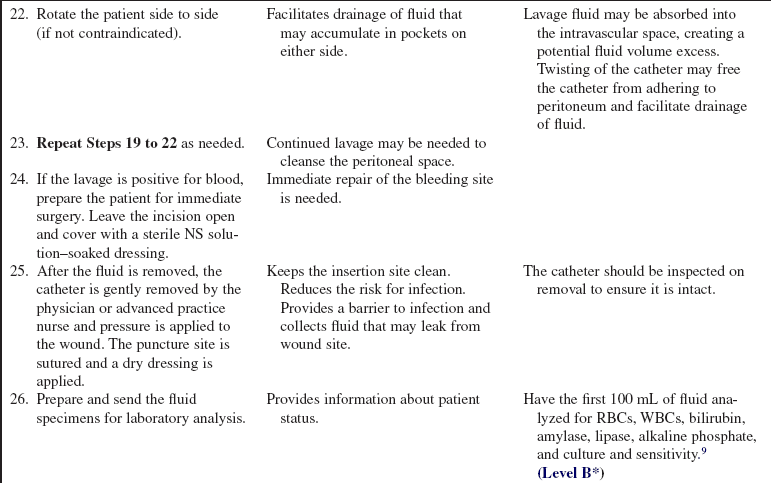
• Diagnostic peritoneal lavage can be used as a tool in patients with hypotension of uncertain etiology, in the presence of trauma.6
• Diagnostic peritoneal lavage is not needed if abdominal surgery is already indicated.7,9
• Because it is an invasive procedure, diagnostic peritoneal lavage does have a small risk of visceral injury (0.6%).5
• Diagnostic peritoneal lavage is 95% sensitive and 99% specific for intraperitoneal blood; however, it cannot exclude retroperitoneal hemorrhage, disruption of the diaphragm, or hollow viscus perforation.5,7
• Computed tomographic (CT) scan frequently is used in hemodynamically stable trauma cases as the diagnostic procedure of choice.5 Also, abdominal ultrasound scan and focused abdominal sonography in trauma (FAST) have been increasingly used to screen blunt abdominal trauma cases for hemoperitoneum.9
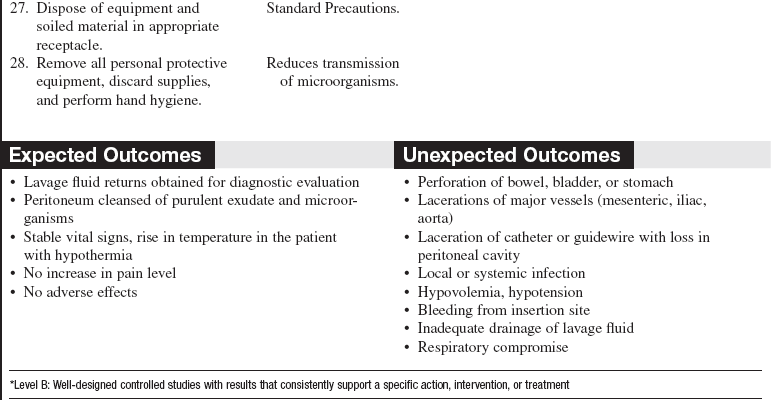
• In patients with hemodynamically unstable conditions, diagnostic peritoneal lavage (DPL) may be preferred by some practitioners because of its high sensitivity.1,2,5,9 DPL is quick, inexpensive, safe, and highly sensitive to the presence of blood in the peritoneal cavity.5 Hemodynamically unstable cases may also go directly to the operating room for laparotomy.
• Complementary CT and DPL decreases nontherapeutic laparotomy rates and allows nonoperative management of those patients with solid-organ injury.9
• Peritoneal lavage is absolutely contraindicated in an acute abdomen that needs immediate surgery as indicated by free air on radiograph or penetrating abdominal trauma.
• Relative contraindications for DPL include the following5,6:
 Previous abdominal surgery, especially pelvic surgery
Previous abdominal surgery, especially pelvic surgery
 Distended bladder that cannot be emptied with a Foley catheter
Distended bladder that cannot be emptied with a Foley catheter
 Obvious infection at intended site of insertion (cellulitis or abscess)
Obvious infection at intended site of insertion (cellulitis or abscess)
• Practitioners should use caution when performing DPL in patients with suspected pelvic fractures (a supraumbilical site may be used) because of false-positive results7; if performed in pregnant patients of more than 12 weeks’ gestation, an open technique, superior to the uterus, is used.7
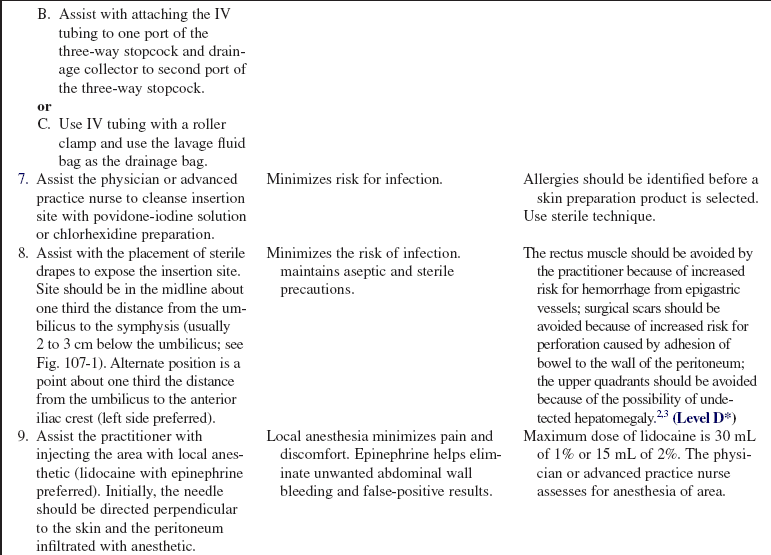
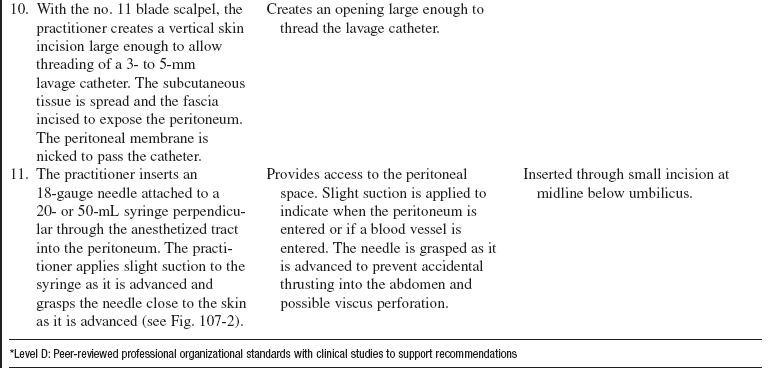
• The practitioner who performs peritoneal lavage should choose an insertion site midline, one third the distance from the umbilicus to the symphysis, or 2 to 3 cm below the umbilicus (see Fig. 107-1). An alternate position is a point one third the distance from the umbilicus to the anterior iliac crest (left side preferred).
• The physician or advanced practice nurse can use ultrasound scan before peritoneal lavage to locate fluid and during the procedure to guide insertion of the catheter.9
EQUIPMENT
• Commercially prepared kit or the following:
 Personal protective equipment, including sterile gloves, mask, goggles, and gown
Personal protective equipment, including sterile gloves, mask, goggles, and gown
 Skin cleansing solution (chlorhexidine or povidone iodine)
Skin cleansing solution (chlorhexidine or povidone iodine)
 Sterile towels or sterile drape
Sterile towels or sterile drape
 Razor to shave area, if necessary
Razor to shave area, if necessary
 Local anesthetic for injection: 1% or 2% lidocaine with epinephrine
Local anesthetic for injection: 1% or 2% lidocaine with epinephrine
 5- or 10-mL syringe with 25- or 27-gauge needle for anesthetic
5- or 10-mL syringe with 25- or 27-gauge needle for anesthetic
 Scalpel and no. 11 knife blade
Scalpel and no. 11 knife blade
 Trocar with stylet; needle (16-, 18-, or 20-gauge) or angiocatheter; depending on abdominal wall thickness may use guidewire with floppy tip and 9 to 18 Fr peritoneal lavage catheter
Trocar with stylet; needle (16-, 18-, or 20-gauge) or angiocatheter; depending on abdominal wall thickness may use guidewire with floppy tip and 9 to 18 Fr peritoneal lavage catheter
 20-mL syringe for diagnostic tap
20-mL syringe for diagnostic tap
 Sterile intravenous (IV) tubing (without valves) with appropriate sterile connectors for lavage catheter and IV bags
Sterile intravenous (IV) tubing (without valves) with appropriate sterile connectors for lavage catheter and IV bags
 Warmed Ringer’s lactate (RL), normal saline (NS), or antibiotic solution for infusion into abdomen
Warmed Ringer’s lactate (RL), normal saline (NS), or antibiotic solution for infusion into abdomen
 Three-way stopcock for therapeutic lavage
Three-way stopcock for therapeutic lavage
 Nylon skin suture material on cutting needle (4-0 or 5-0) and needle holder
Nylon skin suture material on cutting needle (4-0 or 5-0) and needle holder
 Four to six sterile 4 × 4 gauze pads
Four to six sterile 4 × 4 gauze pads
PATIENT AND FAMILY EDUCATION
• Reinforce the indications, the procedure, and the risks to the patient and family.  Rationale: Patient anxiety may be decreased, and patient and family cooperation and understanding of procedure are encouraged.
Rationale: Patient anxiety may be decreased, and patient and family cooperation and understanding of procedure are encouraged.
• Explain the patient’s role in assisting with the procedure and postprocedure care.  Rationale: Patient cooperation during and after the procedure is elicited.
Rationale: Patient cooperation during and after the procedure is elicited.
• Explain the signs and symptoms to report, such as fever, abdominal pain, decreased urine output, bleeding, and leakage of fluid from wound site.  Rationale: Unexpected outcomes may not manifest themselves for a period of time after the procedure.
Rationale: Unexpected outcomes may not manifest themselves for a period of time after the procedure.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Obtain the medical history and perform a review of systems to identify abdominal injury, peritonitis, intraabdominal abscess, or pregnancy.  Rationale: Certain conditions of the gastrointestinal tract may be diagnosed and treated with peritoneal lavage. Contraindications to peritoneal lavage may be identified.6
Rationale: Certain conditions of the gastrointestinal tract may be diagnosed and treated with peritoneal lavage. Contraindications to peritoneal lavage may be identified.6
• Identify the presence of any allergies to medication or other substances.  Rationale: Patients may have allergies to skin preparations or anesthetics used before the invasive procedure is performed. Identification assists the practitioner in choosing the most appropriate skin preparation and anesthetic.
Rationale: Patients may have allergies to skin preparations or anesthetics used before the invasive procedure is performed. Identification assists the practitioner in choosing the most appropriate skin preparation and anesthetic.
• Assess for bowel or bladder distention.  Rationale: Distension increases the risk for bowel or bladder perforation during the procedure.7
Rationale: Distension increases the risk for bowel or bladder perforation during the procedure.7
• Assess coagulation study results (i.e., prothrombin time [PT], partial thromboplastin time [PTT], and platelets).  Rationale: Abnormal clotting study results may increase the risk for bleeding during and after the procedure. Therapy may be necessary to correct clotting abnormalities before the procedure is performed.
Rationale: Abnormal clotting study results may increase the risk for bleeding during and after the procedure. Therapy may be necessary to correct clotting abnormalities before the procedure is performed.
• Plain and upright radiographs of the abdomen should be ordered by the physician or advanced practice nurse, and upright abdominal films if possible (before the procedure).  Rationale: Air is introduced during the procedure and may confound the diagnosis later.7
Rationale: Air is introduced during the procedure and may confound the diagnosis later.7
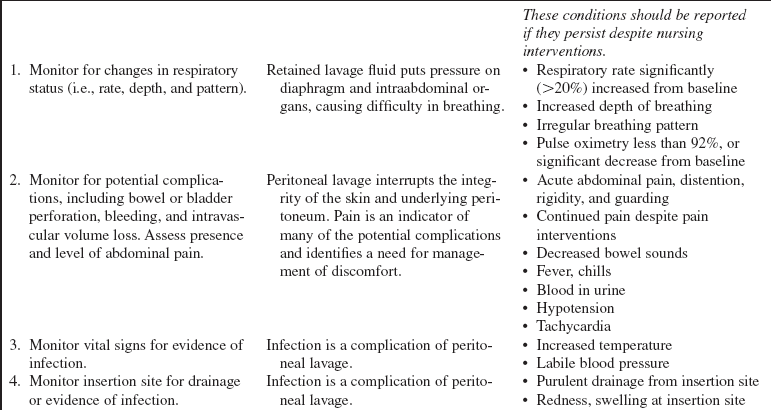
• Obtain baseline vital signs and pain assessment according to institutional standard.  Rationale: The practitioner can identify intraprocedure or postprocedure changes that may be indicative of complications.
Rationale: The practitioner can identify intraprocedure or postprocedure changes that may be indicative of complications.
Patient Preparation
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Ensure that a written informed consent form has been obtained by the practitioner performing the procedure (if possible). The healthcare provider who is assisting may be a witness to the signing of the consent if needed. In a trauma situation or with an unresponsive patient, this consent may be implied.  Rationale: Peritoneal lavage is an invasive procedure that requires a signed consent form.
Rationale: Peritoneal lavage is an invasive procedure that requires a signed consent form.
• Have the patient void or insert a urinary drainage catheter.  Rationale: A distended bladder increases the risk for bladder perforation during the procedure.7
Rationale: A distended bladder increases the risk for bladder perforation during the procedure.7
• Insert a nasogastric tube unless contraindicated (e.g., in significant facial trauma) and attach to low intermittent suction.  Rationale: A distended stomach increases the risk for perforation during the procedure.6
Rationale: A distended stomach increases the risk for perforation during the procedure.6
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the physician or advanced practice nurse and the healthcare provider assisting in the procedure should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the physician or advanced practice nurse and the healthcare provider assisting in the procedure should ensure the correct identification of the patient for the intended intervention.
• Check that all relevant documents and studies are available before starting the procedure.  Rationale: This measure ensures that the correct patient receives the correct procedure.
Rationale: This measure ensures that the correct patient receives the correct procedure.
• Place the patient in the supine position (may tilt to side of collection slightly for improved fluid positioning).  Rationale: Fluid accumulates in the dependent areas.
Rationale: Fluid accumulates in the dependent areas.
• The physician or advanced practice nurse examines the abdomen for landmarks and marks appropriately.  Rationale: Correct placement of the catheter for peritoneal lavage minimizes complications.
Rationale: Correct placement of the catheter for peritoneal lavage minimizes complications.
• For the patient with pain or agitation who is unable to cooperate with the procedure, consider analgesia or sedation. If sedation is needed for the procedure, institution-specific moderate sedation monitoring should be performed.  Rationale: Analgesia or sedation provides for patient comfort and safety during the procedure.
Rationale: Analgesia or sedation provides for patient comfort and safety during the procedure.
• If the patient has altered mental status, soft wrist restraints may be needed.  Rationale: The patient must not move his or her hands into the sterile field once it has been established.
Rationale: The patient must not move his or her hands into the sterile field once it has been established.
References
![]() 1. Brakenridge, SC, et al. Detection of intra-abdominal injury using diagnostic peritoneal lavage after shotgun wound to the abdomen. J Trauma. 2003; 54:329–331.
1. Brakenridge, SC, et al. Detection of intra-abdominal injury using diagnostic peritoneal lavage after shotgun wound to the abdomen. J Trauma. 2003; 54:329–331.
2. Crandall, M, West, MA, Evaluation of the abdomen in the critically ill patient. opening the black box. Curr Opin Crit Care 2006; 12:333–339.
3. Ferri, FF. Paracentesis. In Ferri, ed. : Practical guide to the care of the medical patient, ed 7, Philadelphia: Mosby/Elsevier, 2007.
4. Griffin, XL, Pullinger, R. Are diagnostic peritoneal lavage or focused abdominal sonography for trauma safe screening interventions for hemodynamically stable patients after blunt abdominal trauma? A review of the literature. J Trauma. 2007; 62:779–784.
5. Jansen, JO, Yule, SR, Loudon, MA. Investigation of blunt abdominal trauma. BMJ. 2008; 336:938–942.
![]() 6. Marx, JA. Peritoneal procedures. In: Roberts JR, Hedges JR, eds. Clinical procedures in emergency medicine. ed 4. Philadelphia: Saunders; 2004:733–749.
6. Marx, JA. Peritoneal procedures. In: Roberts JR, Hedges JR, eds. Clinical procedures in emergency medicine. ed 4. Philadelphia: Saunders; 2004:733–749.
![]() 7. Proehl J, ed.. Diagnostic peritoneal lavage. Emergency nursing procedures. ed 4. Elsevier, St Louis, 2008.
7. Proehl J, ed.. Diagnostic peritoneal lavage. Emergency nursing procedures. ed 4. Elsevier, St Louis, 2008.
![]() 8. Sato, T, Hirose, Y, Saito, H, et al, Diagnostic peritoneal lavage for diagnosing blunt hollow visceral injury. the accuracy of two different criteria and their combination. Surg Today . 2005; 35:935–939.
8. Sato, T, Hirose, Y, Saito, H, et al, Diagnostic peritoneal lavage for diagnosing blunt hollow visceral injury. the accuracy of two different criteria and their combination. Surg Today . 2005; 35:935–939.
9. Thacker, LK, Parks, J, Thal, ER, Diagnostic peritoneal lavage. is 100,000 RBC’s a valid figure for penetrating abdominal trauma. J Trauma Injury Infect Crit Care 2007; 62:853–857.
Bode, PJ, van Vugt AB. Ultrasound in the diagnosis of injury. Injury. 1996; 27:379–383.
Brown, MA, et al, Blunt abdominal trauma. screening US in 2,693 patients. Radiology 2001; 218:352–358.
Goletti, O, et al, The role of ultrasonography in blunt abdominal trauma. results in 250 consecutive cases. J Trauma 1994; 36:178–181.
Gonzalez, RP, et al. Complementary roles of diagnostic peritoneal lavage and computed tomography in the evaluation of blunt abdominal trauma. J Trauma. 2001; 51:1128–1134.
Liu, A, Kaufmann, C, Ritchie, R. A computer-based simulator for diagnostic peritoneal lavage. Stud Health Technol Inform. 2001; 81:278–285.
Marx, JA, et al, Limitations of computed tomography in the evaluation of acute abdominal trauma. a prospective comparison with diagnostic peritoneal lavage. J Trauma 1985; 25:933–937.
Maxwell-Armstrong C, et al, Diagnostic peritoneal lavage analysis. should trauma guidelines be revised. Emerg Med J 2002; 19:524–525.
Root, HD, et al. Diagnostic peritoneal lavage. Surgery. 1965; 57:633–637.