The Pleura
The pleura is a serous membrane consisting of two layers the visceral and the parietal pleura. The parietal pleura covers the inner aspect of the chest wall and the diaphragm. The visceral pleura is strongly adherent to the surface of the lungs and interlobar fissures. In healthy persons, the space between the visceral and parietal pleura is nothing more than two apposed pleural surfaces separated by a trace of glycoprotein-rich fluid. In normal conditions, no imaging study can visualize the pleural space because pleural membranes are only 0.2 to 0.4 mm thick, and the physiologic volume of pleural fluid forms a thin 5- to 10-micron layer. However, in children, various pathologic processes can occur within this space that require imaging evaluation. In this chapter, etiologies, imaging characteristics, treatment, and follow-up of pathologic processes involving the pleura are discussed.1–4
Pleural Effusion
Etiology: The lymphatic system, which is part of the immune system and comprises a network of lymphatic vessels, plays an important role in the homeostasis of pleural fluid. Excess production or decreased absorption of lymphatic fluid can result in an increased volume of pleural fluid.1,5 Pleural effusions may be caused by systemic diseases or local infectious/inflammatory processes.
Pleural effusions traditionally are classified into two types: transudates and exudates. Transudates usually result from underlying systemic diseases that alter the normal balance of formation and absorption of pleural fluid. Transudative pleural effusions commonly are seen in patients with nephrotic syndrome, heart failure, and cirrhosis. Exudates typically are caused by local infectious or inflammatory processes that result in the increased formation of pleural fluid. Exudative pleural effusions usually are seen in patients with pulmonary infections, neoplasms, hemothorax, and collagen vascular diseases.3–5
Causes of pleural effusion in pediatric patients differ substantially from those in adults. Whereas the most frequent cause of effusions in adults is congestive heart failure, pleural effusions in children are most commonly a result of underlying pleuropulmonary infection (Table 60-1).3 Although pediatric patients with small pleural effusions are usually asymptomatic, large pleural effusions can result in symptomatic respiratory distress or inspiratory pleuric chest pain as a result of stretching of the parietal pleura.3 When infection is the underlying cause, the predominant symptoms are cough, dyspnea, fever, and elevated white blood cell counts.1,3
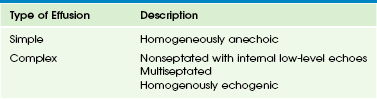
Table 60-1
| Phase | Description |
| Exudative | Pleural inflammation leads to accumulation of free-flowing clear liquid |
| Fibrinopurulent | Deposition of fibrin in the pleural space results in septation/loculations limiting the flow of fluid; pus accumulates in the pleural cavity |
| Organizing phase | Fibroblasts infiltrate the pleura, forming a rigid pleura and preventing lung expansion |
Imaging: The first-line imaging modality, chest radiography, plays an important role in the initial diagnosis of pleural effusions in children. The radiographic appearance of pleural effusions depends on the volume and consistency of the pleural fluid, the patient’s position, and the presence of septations and/or loculations. On chest radiographs, a free-flowing effusion forms an internally concave meniscus paralleling the chest wall that changes in position on lateral decubitus radiographs. On supine radiographs, a mobile fluid may layer over the hemithorax, resulting in a diffuse opacity. The presence of a lentiform-shaped effusion with internal convex margins is suggestive of a loculated pleural effusion.2,6
The most common indication of chest ultrasound in children is to characterize an opaque hemithorax seen on a chest radiograph (Fig. 60-1).6,7 Ultrasound is the best imaging modality in diagnosing and characterizing pleural fluid.7 Ultrasound is more sensitive than radiographs in detecting pleural fluid, particularly when the amount is small (~5 mL).2,8
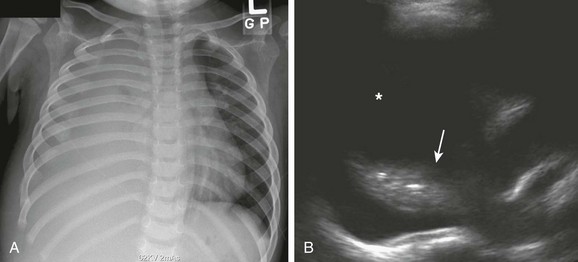
Figure 60-1 Simple effusion in a 2-year-old boy.
A, Complete opacification of the right hemithorax with obliteration of the right side of the mediastinum and hemidiaphragm. The cardiac and tracheal deviations to the left are imaging findings suggestive of a pleural effusion. B, Ultrasound of the right hemithorax confirms the presence of a large simple pleural effusion (asterisk). Consolidation (arrow) of the underlying lung also is seen.
The internal echogenicity of pleural effusions on ultrasound can be categorized into four types (Table 60-2): (1) homogeneously anechoic (see Fig. 60-1, B); (2) nonseptated with internal low-level echoes (Fig. 60-2); (3) septated (Fig. 60-3, A); and (4) homogeneously echogenic (Fig. 60-4, A).7,9 Anechoic and free-flowing effusions are called simple pleural effusions, whereas the remainder are classified as complex pleural effusions.
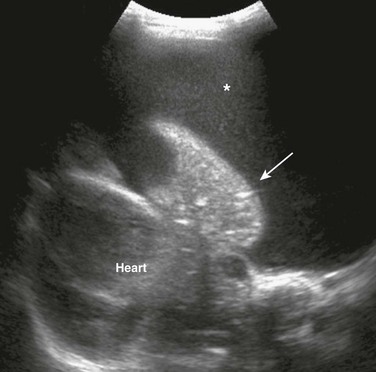
Figure 60-2 Complex effusion with low-level echoes in a 9-year-old girl with bacterial pneumonia.
An ultrasound image of the left hemithorax reveals a large pleural effusion with floating low-level echoes indicating debris (asterisk) and the consolidated underlying lung (arrow).
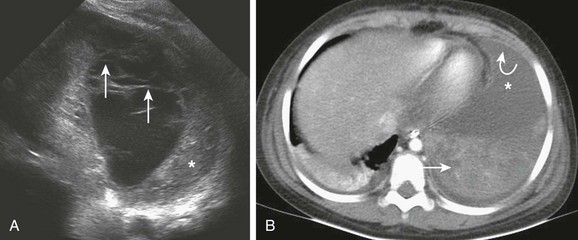
Figure 60-3 Complex septated effusion in a 6-year-old patient with bacterial pneumonia.
A, An ultrasound image of the left hemithorax shows a large parapneumonic effusion with multiple septations (arrows). Consolidation of the adjacent lung also is present (asterisk). B, An axial postcontrast computed tomography (CT) image shows the pleural effusion (asterisk) in the anterior aspect of the left base. The septations seen on the ultrasound are not clearly visualized on CT; however, pleural enhancement is present (curved arrow). The adjacent consolidated lung also is noted (straight arrow).
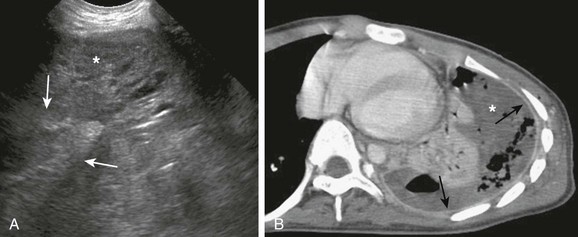
Figure 60-4 Complex effusion in a 6-year-old patient with bacterial pneumonia.
A, An ultrasound image shows a mostly solid-appearing parapneumonic effusion (arrows). The consolidated underlying lung (asterisk) also is seen. B, An axial contrast-enhanced computed tomography image shows the large pleural effusion (asterisk) with pleural enhancement (arrows).
Computed tomography (CT) also is more sensitive than chest radiographs in detecting small pleural effusions. The advantage of CT is that it provides an unobstructed view of the entire underlying lung parenchyma, mediastinum, and chest wall; however, it is associated with ionizing radiation exposure. Intravenous administration of contrast material is necessary to optimally visualize and assess the pleura and lung parenchyma (Fig. 60-4, B). In comparison to ultrasound, CT is limited in characterizing pleural effusions and demonstrating internal septations (see Fig. 60-3).2
Treatment and Follow-up: The main treatment of choice for pleural effusions is thoracentesis, which can be helpful in evaluating the underlying cause of the pleural effusion and also in relieving symptoms. Indications for thoracentesis in children with pleural effusions are persistent fever, respiratory compromise, mediastinal shift, pleuritic pain, and underlying lung disease.3 The management of parapneumonic effusion is discussed in the following section.
Parapneumonic Effusion and Empyema
Etiology: A parapneumonic pleural effusion refers to a pleural fluid collection in association with an underlying pneumonia, whereas empyema is the presence of pus in the pleural space.1,10 Streptococcus pneumoniae is still the main etiological agent in parapneumonic effusions in children, although the number of cases caused by Staphylococcus aureus has increased.1,10 More recently, the Streptococcus milleri group, typically found in the oropharynx and upper respiratory and gastrointestinal tracts, has been recognized as an important pathogen causing purulent pleuropulmonary infections, especially in immunocompromised patients.11
Pleural infection can be classified into three phases based on the progression of infection: exudative, fibrinopurulent, and organizing (Box 60-1). During the exudative phase, the inflammatory process associated with the underlying pneumonia leads to the accumulation of free-flowing clear fluid within the pleural cavity. During the fibrinopurulent phase, deposition of fibrin in the pleural space results in septations and loculations, limiting the flow of pleural fluid. The fibrinopurulent phase may be divided into two stages: (1) early fibrinopurulent stage A and (2) late fibrinopurulent stage B. The early fibrinopurulent stage A is characterized by an increase in white blood cell accumulation, which causes thickening of the pleural fluid consistency. The late fibrinopurulent stage B is defined as the accumulation of pus in the pleural space. The organizing phase begins when fibroblasts infiltrate the pleural cavity, forming a thick rigid pleural rind. This pleural rind prevents lung reexpansion, impairs lung function, and creates a persistent pleural space with ongoing potential for infection. At this stage, spontaneous healing eventually may occur, or a chronic empyema may develop.1,6,12
Imaging: A chest radiograph is the initial imaging modality for assessing the presence of parapneumonic effusions. Ultrasound subsequently can be obtained for characterization of the parapneumonic effusion. In most cases, parapneumonic effusions are exudates and therefore are complex in appearance on ultrasound, although they may be simple in appearance during the early stage.9,13 As the underlying infection progresses, parapneumonic effusions may develop low-level internal echoes and floating debris (see Fig. 60-2) followed by septations and loculations (see Fig. 60-3, A), preventing free motion of the fluid. The internal echoes indicate increased underlying cellularity of fluid; these pleural effusions are usually exudates but not necessarily empyemas.1,6,7,9,13 The parapneumonic effusion eventually may become semi-solid in appearance on ultrasound (see Fig. 60-4, A). The development of pleural thickening indicates the presence of a fibrous capsule.
The routine use of CT is not necessary to evaluate parapneumonic pleural effusions, particularly in pediatric patients, because it entails exposure to ionizing radiation.1,6,14 However, CT with intravenous contrast may aid in the evaluation of the lung parenchyma when a complication such as a bronchopleural fistula is suspected (Fig. 60-5) or in the differentiation of a parapneumonic effusion from a lung abscess.2 An imaging finding suggestive of empyema on CT is a lentiform-shaped fluid collection with pleural thickening and/or enhancement.15 In contrast, lung abscesses tend to be round and are embedded within the lung parenchyma rather than displacing it.2 Loculations in parapneumonic effusions, which are best visualized by ultrasound, can be suggested on CT indirectly when the surface of the underlying lung shows smooth indentations due to fibrin strands that produce intrapleural adhesions, or in the presence of a lentiform-shaped pleural fluid collection.2 The presence of air or gas in the dependant portion of the effusion also is an imaging finding that suggests loculation (see Fig. 60-4, B). In the absence of a previous thoracentesis or thoracostomy tube placement, the presence of air/gas or an air-fluid level in the pleural cavity in a patient with pneumonia is diagnostic of a bronchopleural fistula (see Fig. 60-5).1,2,6,16,17 If a bronchopleural fistula is peripheral in location, the direct communication between the lung and the pleural space occasionally can be visualized on CT.16,17
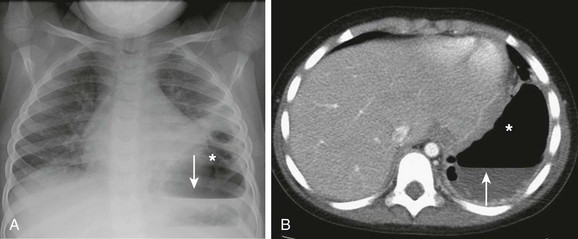
Figure 60-5 A bronchopleural fistula in a 4-year-old boy with necrotizing pneumonia.
A, A frontal chest radiograph shows a collection of air in the left pleural space superior to the gastric bubble (asterisk), with an air-fluid level (arrow) indicating a hydropneumothorax. B, An axial contrast-enhanced computed tomography image of the same patient confirms the presence of air in the pleural space (asterisk) and the air-fluid level (arrow).
Treatment and Follow-up: Anechoic simple pleural effusions can be managed by thoracentesis or percutaneous placement of a chest tube. Because 50% of parapneumonic effusions recur after aspiration in children, the routine placement of a drainage catheter currently is recommended after aspiration.7 Distinction between parapneumonic pleural effusions and empyema in children is less important than in adults because diagnostic thoracentesis is rarely performed before definitive treatment in children with clinically suspected pleuropulmonary infection.1,6 However, the optimal management of parapneumonic effusions and empyemas in children currently is not clearly established.
The management choice for complex pleural effusions in children, particularly in the presence of septations, is currently somewhat controversial. Some investigators advocate the use of percutaneous insertion of a chest tube combined with instillation of a fibrinolytic agent, whereas others support the use of video-assisted thoracoscopy (VATS).1,18–22 The presence of septations or complex effusions is not necessarily a contraindication for percutaneous drainage. However, concomitant fibrinolytic therapy typically is required and should be started promptly to maximize the benefit of the procedure.23,24 In a retrospective study consisting of 54 pediatric patients with parapneumonic effusions, chest tube insertion with intrapleural instillation of a fibrinolytic agent was successful, safe, and less costly as the first therapeutic option compared with VATS.25 A recent cost-effective analysis study of the management of empyema in children that was conducted with a Bayesian tree approach showed that chest tube insertion with instillation of a fibrinolytic agent was the most cost-effective strategy for treating pediatric empyema based on the length of hospital stay.26 The management of bronchopleural fistulas is initially medical, including pleural space decompression with a thoracotomy tube and nutritional support. When conservative management is ineffective, closure of the fistula must be considered through VATS for peripheral fistulas and through an open thoracotomy for central fistulas.16,27
In children with parapneumonic effusions or empyema that is successfully treated, most chest radiographs return to the baseline between 3 and 6 months. The British Thoracic Society currently recommends follow-up chest radiographs in 4 to 6 weeks after treatment of parapneumonic effusion or empyema.1 In cases of no improvement on follow-up chest radiographs, either a subsequent ultrasound or a CT scan may be beneficial to exclude underlying complications.1,6,28
Pneumothorax
Etiology: Pneumothorax is the presence of air in the potential space between the parietal and visceral pleura. Pneumothorax can be classified into two categories based on the underlying etiology: spontaneous and traumatic. Spontaneous pneumothorax can be further subdivided into primary and secondary. Primary spontaneous pneumothorax occurs in an otherwise healthy child and often is attributed to a ruptured preexisting apical bleb or bulla. Secondary spontaneous pneumothorax occurs as a complication of an underlying pulmonary disease, most commonly asthma and cystic fibrosis in children.29,30 In the United States, the incidence of spontaneous pneumothorax is approximately 1.8 to 7.4 per 100,000 in boys and 1.2 to 6 per 100,000 in girls. The mean age at presentation is 14 to 15.9 years.29,31 The classic phenotype is a thin, tall male with a low body mass index. Children with primary spontaneous pneumothorax typically present with a sudden onset of unilateral chest pain and dyspnea at rest. Patients with secondary spontaneous pneumothorax often present with cardiopulmonary distress.29,31 Traumatic pneumothorax occurs as a result of blunt or penetrating mechanisms, with iatrogenic pneumothorax being a subset resulting from medical procedures. The outcome of traumatic pneumothorax that causes the most concern is progression to tension pneumothorax. Tension phenomenon occurs when the lung or airway defect acts as a check-valve mechanism, allowing flow of air into, but not out from, the pleural cavity. The diagnosis of tension pneumothorax is based on both radiologic and clinical findings. Hemodynamic and ventilatory compromise may be present with rapid cardiorespiratory collapse. On physical examination, signs of tension include neck vein distension, tracheal deviation away from the affected side, and cyanosis.29 Tension pneumothorax in the absence of trauma is rare in pediatric patients, occurring in 1% to 3% of cases.32
Imaging: Chest radiography is the initial test in the diagnosis of a pneumothorax by visualizing the visceral pleural with absence of pulmonary markings beyond the pleural margin (Fig. 60-6, A). For evaluation of pneumothorax, an upright chest radiograph is the procedure of choice, with a lateral decubitus as an alternative.29,31 Inspiratory and expiratory views are reported to be equally sensitive in the detection of pneumothorax, and thus the expiratory view does not need to be obtained routinely.33 On chest radiographs, a tension pneumothorax is characterized by a large pneumothorax, resulting in collapse of the ipsilateral lung and shifting of the mediastinum, including the trachea, to the contralateral side.29 Widened ipsilateral rib spaces and flattening of the diaphragm are also often seen in patients with a tension pneumothorax.
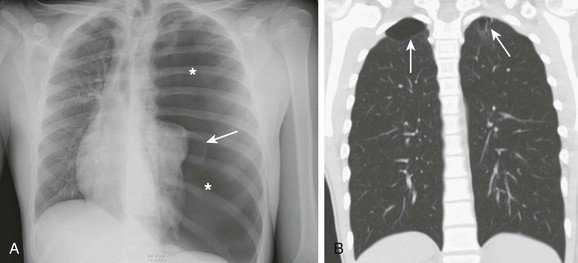
Figure 60-6 Spontaneous pneumothorax in a tall, thin teenager presenting with tachypnea and tachycardia but a normal blood pressure reading.
A, A frontal chest radiograph shows a large pneumothorax occupying the entire left hemithorax (asterisks), with a mild cardiomediastinal shift to the right. A bleb is noted along the surface of the collapsed left lung (arrow). B, A coronal computed tomography image using a lung window obtained 1 month after thoracotomy tube removal shows biapical blebs (arrows), which are larger on the right. The right apical bleb was not seen on the chest radiographs.
Although ultrasound is rarely used for evaluating pneumothorax, it is important to recognize the sonographic finding of a pneumothorax, because it may be encountered during ultrasound evaluation of the pediatric chest performed for other reasons. Without a pneumothorax, the strong acoustic interface between the pleura and aerated lung produces posterior reverberations. The normal sliding motion of the lung during respiration also is visualized. When air is introduced into the pleural space, the normal tension between the pleural layers is lost and a gap is created between the parietal and visceral pleura, disrupting the normal acoustic interface. The sliding of the underlying lung no longer can be seen, and the normal reverberation is replaced by a static homogeneous acoustic shadowing.7,29 A recent literature review reported a sensitivity between 86% and 98% and a specificity between 97% and 100% for ultrasound compared with a sensitivity between 28% and 75% for supine chest radiographs in detecting pneumothorax.34
In cases of primary spontaneous pneumothorax, a CT scan may play a role in identifying pre-existing subpleural blebs and bullae (Fig. 60-6, B). The exact relationship between blebs and primary spontaneous pneumothorax is not clear. However, with CT, there is an increased recognition of subpleural blebs in patients with primary spontaneous pneumothorax and, in particular, in patients presenting with recurrent pneumothoraces.35–40
Treatment and Follow-up: No pediatric-specific management guidelines for primary spontaneous pneumothorax have been developed to date. Pediatric patients have not been addressed separately in the available international guidelines.30,31 In the setting of primary spontaneous pneumothorax, observation should be the initial management of choice for small closed pneumothoraces separated less than 2 cm from the chest wall in asymptomatic patients. Administration of oxygen should be considered because it may increase the rate of reabsorption of the pneumothorax. Symptomatic pneumothoraces, whether primary or secondary, require active intervention with a simple aspiration or placement of a thoracostomy tube in cases of a large pneumothorax.29,30 When a tension pneumothorax is present, a large-bore needle or angiocatheter should be inserted in the affected side at the second intercostal space to decompress the tension pneumothorax in a timely fashion.29
The risk of recurrence after a single episode of spontaneous pneumothorax with conservative treatment ranges from 16% to 52%.40 Patients with a primary spontaneous pneumothorax that is treated successfully by a simple aspiration should be observed before discharge. Patients with a spontaneous pneumothorax who are discharged without intervention should have a follow-up chest radiograph after 2 weeks. Patients who have a secondary pneumothorax that is treated with simple aspiration should be admitted for 24 hours for a repeat chest radiograph to ensure no recurrence.30 The exact indications for CT in the pediatric population in the setting of spontaneous pneumothorax currently are not well established. It has been advocated that a limited CT scan of the lung apices with coronal reconstruction may suffice in children because most blebs and bullae occur in this location, thus allowing a decrease in radiation exposure.31,38
Pleural Neoplasms
Etiology: Pleural tumors in children are rare and much less common than in adults. Secondary neoplasms (i.e., metastasis or direct invasion) are more common than are primary tumors.7 Metastatic neoplasms involving the pleura include lymphoma, neuroblastoma, Wilms tumors, rhabdomyosarcoma, and other sarcomas.7 A metastatic Wilms tumor may involve the peritoneal, pleural, and pericardial cavities and is one of the most common causes of malignant effusions in children.41
Primary malignant tumors of the pleura include desmoplastic small round cell tumors and mesotheliomas. The former more commonly occur in the peritoneal cavity but may arise primarily from the pleura.42,43 Mesotheliomas are regarded as an adult-type neoplasm that rarely occur in children in the second decade. Clinicopathologic features of mesothelioma are similar to those in adults, with a predilection for the pleura, a male predominance, and a poor prognosis.44 Malignant pleural tumors typically present with chest pain and respiratory distress, especially in the presence of a large pleural effusion.
The most common benign lesions of the pleura include a calcifying fibrous tumor, myofibromatosis, and lipomas.42 Calcifying fibrous tumors usually are found in subcutaneous and deep soft tissues, but on rare occasions have been reported in the pleura.42
Imaging: Malignant pleural neoplasms, whether primary or secondary, usually manifest with pleural effusions that initially are identified on chest radiographs. Ultrasound subsequently can be used for the confirmation and characterization of pleural neoplasms. Pleural metastases tend to produce large effusions with hemorrhage presenting as increased cellularity and low-level echoes on ultrasound. The presence of pleural fluid aids in the detection of nodules or masses adherent to the parietal or visceral pleura on ultrasound (Fig. 60-7).7 CT and magnetic resonance imaging are helpful imaging modalities for evaluating the tumor, its extent, and its relationship with adjacent organs. Because of the markedly overlapping imaging findings among different types of primary and secondary pleural neoplasms, definitive diagnosis is based on histopathologic analysis. If the neoplasm is visible on ultrasound, biopsy under ultrasound guidance can be performed for the diagnosis.7
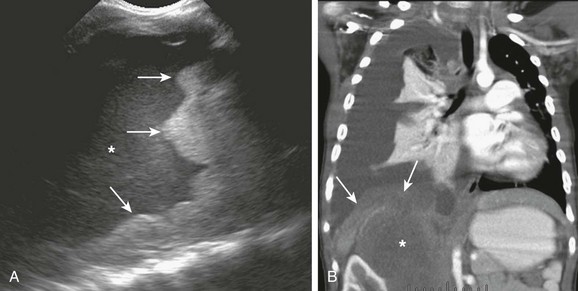
Figure 60-7 A primary retroperitoneal rhabdomyosarcoma with metastasis to the pleura in a 3-year-old girl.
A, Ultrasound of the right hemithorax shows a large complex effusion with low-level echoes (asterisk) and nodularity of the pleura (arrows). B, A coronal contrast-enhanced computed tomography image shows the large right suprarenal rhabdomyosarcoma (asterisk). The soft tissue along the right diaphragm and pleura indicate metastasis (arrows). A secondary large right pleural effusion causing collapse of the right lung also is seen.
Treatment and Follow-up: The current treatment of primary malignant pleural neoplasms is surgical resection, often combined with chemotherapy. When pleural metastasis is discovered, it usually indicates advanced disease, and the treatment is aimed at treating the primary tumor. In cases of recurrent intractable pleural effusions, pleurodesis as a palliative treatment can be performed.45
Balfour-Lynn, IM, Abrahamson, E, Cohen, G, et al. BTS guidelines for the management of pleural infection in children. Thorax. 2005;60:i1–i21.
Calder, A, Owens, CM. Imaging of parapneumonic effusions and empyema in children. Pediatr Radiol. 2009;39:527–537.
Chen, HJ, Tu, CY, Ling, SJ, et al. Sonographic appearances in transudative pleural effusions: not always an anechoic pattern. Ultrasound Med Biol. 2008;34:362–369.
Coley, BD. Chest sonography in children: current indications, techniques, and imaging findings. Radiol Clin N Am. 2011;49(5):825–849.
Johnson, NN, Toledo, A, Endon, EE. Pneumothorax, pneumomediastinum and pulmonary embolism. Pediatr Clin N Am. 2010;57:1357–1383.
References
1. Balfour-Lynn, IM, Abrahamson, E, Cohen, G, et al. BTS guidelines for the management of pleural infection in children. Thorax. 2005;60:i1–i21.
2. Heffner, JE, Klein, JS, Hampson, C. Diagnostic utility and clinical application of imaging for pleural space infections. Chest. 2010;137:467–479.
3. Efrati, O, Barak, A. Pleural effusions in the pediatric population. Pediatr Rev. 2002;23:417–426.
4. Beers, SL, Abramo, TJ. Pleural effusions. Pediatr Emerg Care. 2007;23:330–334.
5. English, JC, Leslie, KO. Pathology of the pleura. Clin Chest Med. 2006;27:157–180.
6. Calder, A, Owens, CM. Imaging of parapneumonic effusions and empyema in children. Pediatr Radiol. 2009;39:527–537.
7. Coley, BD. Pediatric chest ultrasound. Radiol Clin N Am. 2005;43:405–418.
8. Kocijancic, I, Vidmar, K, Ivanovi-Herceg, Z. Chest sonography versus lateral decubitus radiography in the diagnosis of small pleural effusions. J Clin Ultrasound. 2003;31:69–74.
9. Chen, HJ, Tu, CY, Ling, SJ, et al. Sonographic appearances in transudative pleural effusions: not always an anechoic pattern. Ultrasound Med Biol. 2008;34:362–369.
10. Hernandez-Bou, S, Garcia-Garcia, JJ, Esteva, C, et al. Pediatric parapneumonic effusion: epidemiology, clinical characteristics and microbiological diagnosis. Pediatr Pulmonol. 2009;44:1192–1200.
11. Lee, EY, Khatwa, U, McAdam, AJ, et al. Streptococcus milleri group pleuropulmonary infection in children: computed tomographic findings and clinical features. J Comput Assist Tomogr. 2010;34(6):927–932.
12. Hamm, H, Light, RW. Parapneumonic effusion and empyema. Eur Respir J. 1997;10:1150–1156.
13. Yang, PC, Luh, KY, Chang, DB, et al. Value of sonography in determining the nature of pleural effusion: analysis of 320 cases. AJR Am J Roentgenol. 1992;159:29–33.
14. Kurian, J, Levin, TL, Han, BK, et al. Comparison of ultrasound and CT in the evaluation of pneumonia complicated by parapneumonic effusion in children. AJR Am J Roentgenol. 2009;193:648–654.
15. Stark, DD, Federle, MP, Goodman, PC, et al. Differentiating lung abscess and empyema: radiography and computed tomography. AJR Am J Roentgenol. 1983;141:163–167.
16. Sarkar, P, Patel, N, Chusid, J, et al. The role of computed tomography bronchography in the management of bronchopleural fistulas. J Thorac Imaging. 2010;25:W10–W13.
17. Seo, H, Kim, TJ, Jin, KN, et al. Multi-detector row computed tomographic evaluation of bronchopleural fistula: correlation with clinical, bronchoscopic and surgical findings. J Comput Assist Tomogr. 2010;34:13–18.
18. Levinson, GM, Pennington, DW. Intrapleural fibrinolytics with image-guided chest tube drainage for pleural infection. Mayo Clin Proc. 2007;82:407–413.
19. Ampofo, K, Byington, C. Management of parapneumonic empyema. Pediatr Infect Dis J. 2007;26:445–446.
20. Kurt, BA, Winterhalter, KM, Connors, RH, et al. Therapy of parapneumonic effusions in children: video-assisted thoracoscopic surgery versus conventional thoracostomy drainage. Pediatrics. 2006;118:e547–e553.
21. St Peter, SD, Tsao, K, Harrison, C, et al. Thoracoscopic decortication vs tube thoracostomy with fibrinolysis for empyema. Am J Resp Crit Care Med. 2006;174:221–227.
22. Sonnappa, S, Cohen, G, Owens, CM, et al. Comparison of urokinase and video-assisted thoracoscopic surgery for treatment of childhood empyema. Am J Resp Crit Care Med. 2006;174:221–227.
23. Wells, R, Havens, P. Intrapleural fibrinolysis for parapneumonic effusion and empyema in children. Radiology. 2003;228:370–378.
24. Weinstein, M, Restrepo, R, Chait, PG, et al. Effectiveness and safety of tissue plasminogen activator in the management of complicated parapneumonic effusions. Pediatrics. 2004;113:e182–e185.
25. Gates, RL, Hogan, M, Weinstein, S, et al. Drainage, fibrinolytics, or surgery: a comparison of treatment options in pediatric empyema. J Pediatr Surg. 2004;39:1638–1642.
26. Cohen, E, Weinstein, M, Fisman, DN. Cost-effectiveness of competing strategies for the treatment of pediatric empyema. Pediatrics. 2008;121:e1250–e1257.
27. Sakar, P, Chandak, T, Shah, R, et al. Diagnosis and management of bronchopleural fistula. Indian J Chest Dis Allied Sci. 2010;52:97–104.
28. Chan, PW, Crawford, O, Wallis, C, et al. Treatment of pleural empyema. J Pediatr Child Health. 2000;36:375–377.
29. Johnson, NN, Toledo, A, Endom, EE. Pneumothorax, pneumomediastinum and pulmonary embolism. Pediatr Clin N Am. 2010;57:1357–1383.
30. Henry, M, Arnold, T, Harvey, J. BTS guidelines for the management of spontaneous pneumothorax. Thorax. 2003;58(suppl 2):ii39–ii52.
31. Robinson, PD, Cooper, P, Ranganathan, SC. Evidence-based management of paediatric primary spontaneous pneumothorax. Paediatr Respir Rev. 2009;10:110–117.
32. Weissberg, D, Rafaely, Y. Pneumothorax: experience with 1,199 patients. Chest. 2000;117:1279–1285.
33. Seow, A, Kazerooni, EA, Pernicano, PG, et al. Comparison of upright inspiratory and expiratory chest radiographs for detecting pneumothoraces. Am J Roentgenol. 1996;166:313–316.
34. Wilkerson, RG, Stone, MB. Sensitivity of bedside ultrasound and supine antero-posterior chest radiographs for the identification of pneumothorax after blunt trauma. Acad Emerg Med. 2010;17:11–17.
35. Mitlehner, W, Friedrich, M, Dissmann, W. Value of computer tomography in the detection of bullae and blebs in patients with primary spontaneous pneumothorax. Respiration. 1992;59:221–227.
36. Smit, HJ, Wienk, MA, Schreurs, AJ, et al. Do bullae indicate a predisposition to recurrent pneumothorax? Br J Radiol. 2000;73:356–359.
37. Warner, BW, Bailey, WW, Shipley, RT. Value of computed tomography in the lung in the management of primary spontaneous pneumothorax. Am J Surg. 1991;162:39–42.
38. Guimaraes, CV, Donnelly, LF, Warner, BW. CT findings for blebs and bullae in children with spontaneous pneumothorax and comparison with findings in normal age-matched controls. Pediatr Radiol. 2007;37:879–884.
39. Choudhary, AK, Sellars, MEK, Wallis, C, et al. Primary spontaneous pneumothorax in children: the role of CT in guiding management. Clin Radiol. 2005;60:508–511.
40. Shihoe, ADL, Yim, APC, Lee, TW, et al. Can CT scanning be used to select patients with unilateral primary spontaneous pneumothorax for bilateral surgery? Chest. 2000;118:380–383.
41. Schinstine, M, Abati, A, Tsokos, M, et al. Cytological identification of metastatic epithelial nephroblastoma in pleural fluid: report of a case and review of literature. Diagn Cytopathol. 2006;34:621–624.
42. Granville, L, Laga, AC, Allen, TC, et al. Review and update of uncommon primary pleural tumors: a practical approach to diagnosis. Arch Pathol Lab Med. 2005;129:1428–1443.
43. Karavitakis, EM, Moschovi, M, Stefanaki, K, et al. Desmoplastic small round cell tumor of the pleura. Pediatr Blood Cancer. 2007;49:335–338.
44. Coffin, CM, Dehner, LP. Mesothelial and related neoplasms in children and adolescents: a clinicopathologic and immunohistochemical analysis of eight cases. Pediatr Pathol. 1992;12:333–347.
45. Hoffer, FA, Hancock, ML, Hinds, PS, et al. Pleurodesis for effusions in pediatric oncology patients at the end of life. Pediatr Radiol. 2007;37:269–273.