The Mediastinum
Spectrum of Mediastinal Anomalies and Abnormalities
Overview
Pneumomediastinum, also known as mediastinal emphysema, is a condition in which air is present within the mediastinum.1 Pneumomediastinum occurs more frequently in infants than in older children.2 Affected pediatric patients typically present with a sensation of retrosternal fullness, dysphagia, sore throat, chest pain, or dyspnea.
Etiology: Pneumomediastinum may be spontaneous or iatrogenic. Spontaneous pneumomediastinum results from a sudden forceful increase in intraalveolar pressure such as forceful inhalation or the Valsalva maneuver. In this instance, an alveolus can rupture, allowing gas under pressure into the low-pressure pulmonary interstitial compartment. The air then travels via the peribronchovascular space medially toward the hilum, which opens into the mediastinum.3,4 Occasionally, the air dissects along the lymphatics as well and extends to the visceral pleura, where a concomitant pneumothorax may occur. Iatrogenic pneumomediastinum may result from abdominal and cardiac surgery, endotracheal intubation, or cardiac catheterization. Additionally, pneumomediastinum also can occur after foreign body ingestion, trauma to the neck or chest, or any disruption of the tracheobronchial tree or esophagus (e.g., Boerhaave syndrome).2
It is not uncommon for pneumomediastinum and pneumothorax to coexist.5 This phenomenon sometimes can be attributed to a common mechanism of injury, or the pneumothorax may arise as a result of a pneumomediastinum. In addition, potential communications between the mediastinum and the peritoneal cavity exist via anatomic diaphragmatic defects, such as the esophageal hiatus. As such, the pneumoperitoneum can dissect superiorly into the mediastinum and vice versa. Retroperitoneal extension of the pneumomediastinum also may be observed.6 Rarely, air within the mediastinum can enter the spinal canal, which is termed pneumorrhachis.7
Imaging: The air within the mediastinum typically displaces the pleura and lung laterally (Fig. 58-1). It may decompress into the superior mediastinum and dissect along fascial planes into the subcutaneous tissues of the neck and retropharynx (e-Fig. 58-2). In infants and younger children, air within the mediastinum may displace the thymus superiorly to produce the “spinnaker sail” sign (see Fig. 58-1).
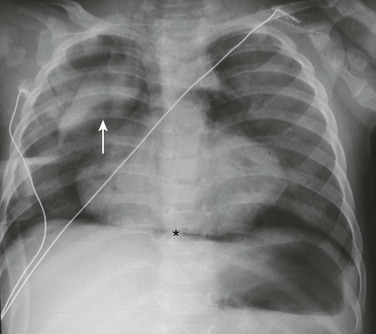
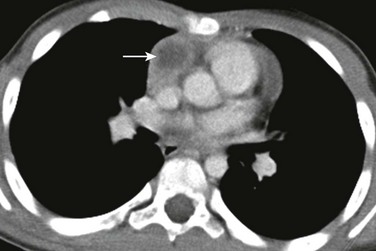
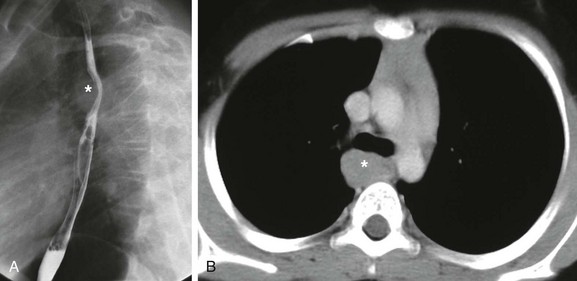
Figure 58-1 Pneumomediastinum in a 6-month-old boy.
A frontal chest radiograph demonstrates a lifted thymic shadow (arrow), the so-called “spinnaker sail sign.” Mediastinal air (asterisk) also is interposed between the central diaphragm and pericardium, and lucency is seen surrounding the heart.
e-Figure 58-2 Pneumomediastinum in a 2-year-old girl.
A, An axial lung window computed tomography (CT) image at the level of the superior mediastinum shows mediastinal air that outlines major vessels and fascial planes. Air has dissected through the soft tissues and is seen bilaterally in the axilla (asterisks). B, An axial lung window CT image at the level of the lower thorax demonstrates further caudal extent of the mediastinal air (asterisk).
With small pneumomediastinum, sometimes only a sliver of curvilinear radiolucency is seen adjacent to the cardiac border, most often on the left. This sliver may sharply outline the aortic arch and descending aorta. When air is adjacent to the pulmonary artery or a branch (typically on the right), the “ring around the artery” sign is seen on the lateral view.6,8 The often-quoted “continuous diaphragm sign” results from air interposed between the pericardium and the diaphragm,8 which effectively erases the normal “silhouetting” of the diaphragm that allows it to be visualized as the single structure that it is.
A large pneumomediastinum may be confused with a pneumothorax, especially when the patient undergoes imaging while in the supine position. In such an equivocal situation, a decubitus radiographic view may be helpful because the mediastinal air does not move, whereas the pneumothorax rises nondependently.5
At times, pneumomediastinum may be difficult to differentiate from pneumopericardium. In contrast to pneumomediastinum, pneumopericardium does not lift the thymus or outline the aortic arch. The air is contained by the pericardium, which can have a dome-shaped superior margin. Pneumopericardium is almost always seen in association with pneumomediastinum except after open-heart surgery.5
Treatment and Follow-up: Treatment of pneumomediastinum is aimed at the underlying cause. For most spontaneous cases of pneumomediastinum, treatment is supportive, including rest, pain control, and avoidance of Valsalva maneuvers.2 If concern exists about the possibility of esophageal rupture, an esophagram using water-soluble contrast may be performed, and a timely surgical consultation should be obtained when the possibility of rupture is present.9,10 Very rarely, pseudotamponade, laryngeal compression, tension pneumomediastinum, tension pneumothorax, or mediastinitis occur and require surgical intervention.
Mediastinal Hemorrhage
Etiology: Mediastinal hemorrhage in pediatric patients usually is due to venous bleeding from blunt trauma.5 Large mediastinal hemorrhage as a result of mediastinal vessel rupture often is due to iatrogenic causes related to central catheter placement or cardiothoracic procedures in pediatric patients. However, mediastinal hemorrhage in children also can occur spontaneously in the context of hemophilia, in which case the hemorrhage may be retropharyngeal and dissect into the mediastinum.5,11 Additionally, rare cases of neonatal thymic hemorrhage have been reported,12 possibly related to vitamin K deficiency.13,14
Imaging: Although imaging findings of mediastinal hemorrhage may be nonspecific, the possibility of mediastinal hemorrhage should be considered when mediastinal widening, blurring of the aortic stripe margin, deviation of a nasoenteric tube, and/or left apical “capping” are present on chest radiographs (Fig. 58-3, A). When evaluating mediastinal widening on chest radiographs, attention must be paid to the technique (i.e., the portable anteroposterior vs. standard posterolateral view). A portable anteroposterior chest radiograph may exaggerate the size of the mediastinum. Therefore in equivocal cases, confirmation with a subsequent posterolateral view or a cross-sectional imaging study such as computed tomography (CT) may be necessary. On CT, mediastinal fluid with a Hounsfield unit greater than water (>20 HU) suggests mediastinal hemorrhage (Fig. 58-3, B).
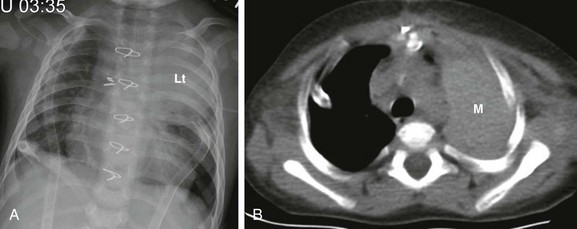
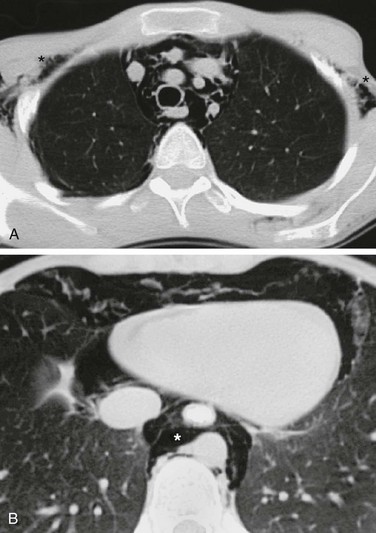
Figure 58-3 A mediastinal hematoma in a 2-year-old girl after open-heart surgery.
A, A frontal chest radiograph shows large left upper lung zone opacity (Lt). No ipsilateral mediastinal shift or other evidence suggestive of atelectasis is present. Also noted are bilateral chest tubes, median sternotomy wires, and surgical clips within the mediastinum. B, An axial unenhanced computed tomography image at the level of the upper thorax reveals a large, left-sided, high-attenuation, masslike area (M) in the left extrapleural (mediastinal) space, indicative of a postprocedural mediastinal hematoma.
Treatment and Follow-up: When mediastinal hemorrhage is considered on chest radiographs, further imaging studies such as echocardiography and/or contrast-enhanced CT using CT angiography protocol with subsequent multiplanar and three-dimensional reconstruction evaluation is warranted. With rapid clinical deterioration, urgent surgical exploration is an option to avoid delaying proper treatment.
Mediastinal Infection
Infections arising de novo in the mediastinum are rare in the pediatric population. Mediastinal infections can be classified into two types: acute and chronic fibrosing mediastinitis. Whereas acute mediastinal infections usually are due to perforation of the esophagus and/or trachea with subsequent cellulitis or abscess formation,15,16 chronic fibrosing mediastinitis typically results from tuberculosis or Histoplasmosis infections.17–19
Acute Mediastinitis
Etiology: Acute superior mediastinal infections typically are due to cervical infection or sternoclavicular osteomyelitis.20–22 The frequent underlying causes for acute anterior and middle mediastinal infections in pediatric patients include the incorrect passage of instruments (e.g., a nasogastric tube or endotracheal tube), impacted foreign bodies, child abuse, or leakage at the sites of surgical anastomoses.23 Posterior acute mediastinal infections usually are due to the extension of osteomyelitis of the vertebrae. Affected pediatric patients typically present with pain, fever, and an elevated white blood cell count.
Imaging: Plain radiographic findings of acute mediastinitis are nonspecific. However, mediastinal widening, obliteration of normal mediastinal contours, and displaced or narrowed trachea should suggest possible underlying acute mediastinitis in the appropriate clinical setting. The more specific radiological imaging finding of acute mediastinitis is the presence of gas within the mediastinum, which can be better evaluated with CT. CT also can show complications from acute mediastinitis such as mediastinal abscess formation or empyema (Fig. 58-4).
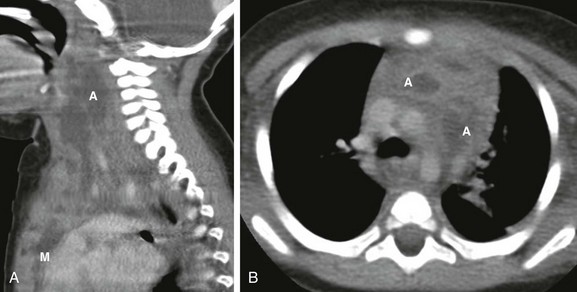
Figure 58-4 Acute mediastinitis resulting from a retropharyngeal abscess in a 1-year-old boy.
A, A sagittal enhanced multiplanar computed tomography (CT) image through the neck shows a large, complex fluid collection (A) extending caudally into the mediastinum (M). B, An axial enhanced CT image obtained at the level of the aortic arch demonstrates two of the better defined abscesses (A) in the anterior mediastinal compartment embedded in an inflamed and heterogenous thymus.
Chronic Fibrosing Mediastinitis
Etiology: Chronic fibrosing mediastinitis, also known as sclerosing mediastinitis, is rare in the pediatric population. It is a condition characterized by abnormal proliferation of dense acellular collagen and fibrous tissue in the mediastinum.26,27 Although it is most frequently attributed to the sequelae of granulomatous infection such as Mycobacterium tuberculosis or Histoplasmosis infection, it also can arise as an idiopathic condition or as the sequelae of autoimmune disease, radiotherapy, or drugs such as methysergide and metoprolol.25,28 Additionally, chronic fibrosing mediastinitis also is associated with retroperitoneal fibrosis, sclerosing cholangitis, Riedel thyroiditis, and pulmonary granuloma.29 Affected pediatric patients often present with respiratory distress related to airway narrowing, dysphagia due to esophageal compromise, and/or facial and neck swelling resulting from obstruction of the superior vena cava.
Imaging: The widening of the mediastinum with a lobular paratracheal and/or subcarinal mass that may be calcified is a typical imaging finding on chest radiographs. CT imaging findings of chronic fibrosing mediastinitis can be categorized into two patterns: focal or diffuse.26,30 Patients affected with focal-type chronic fibrosing mediastinitis typically present with a soft tissue mass, often associated with calcification (63%),30 that is located in the right paratracheal, subcarinal, or hilar regions (Fig. 58-5). On the other hand, pediatric patients affected with diffuse-type chronic fibrosing mediastinitis present with a diffusely infiltrating mass without calcification that often affects entire mediastinal compartments.
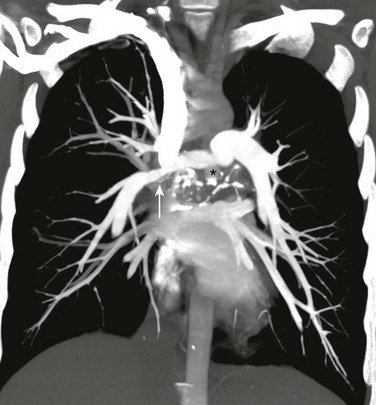
Figure 58-5 Chronic fibrosing mediastinitis in a 17-year-old girl.
A coronal maximum intensity projection computed tomography image of the chest shows a middle mediastinal ill-defined mass that narrows the right pulmonary artery (arrow). Also note the calcifications (asterisk). (From Daltro PA, Santos EN, Gasparetto TD, et al. Pulmonary infections. Pediatr Radiol. 2011;41(Suppl 1):S69-S82.)
Treatment and Follow-up: Treatment of acute mediastinitis consists of the administration of antibiotics that target the offending organisms. Localized mediastinal abscess formation due to acute mediastinitis can be managed with either a surgical or percutaneous abscess drainage procedure. Although no consensus or widely accepted guidelines currently exist for the treatment of chronic fibrosing mediastinitis, systemic antifungal or corticosteroid treatment, surgical resection, and local therapy for complications are the management options currently available. Surgical resection may be necessary for symptomatic pediatric patients who have extensive and aggressive chronic fibrosing mediastinitis that results in either obstruction or compression of mediastinal structures such as central airways, the esophagus, or mediastinal large vessels.
Mediastinal Masses
The mediastinum is the most common location of chest masses in the pediatric population. Mediastinal masses in infants and children can be benign or malignant neoplasms, congenital anomalies, infections, vascular malformations, or pseudomasses. As with adult patients, it is useful to locate the mediastinal mass within one of the three mediastinal compartments (anterior, middle, or posterior) (Fig. 58-6). However, such a system of compartmentalizing the mediastinum may have shortcomings. For example, the borders of the anterior, middle, and posterior mediastinum, which are defined by anatomic landmarks as assessed on a lateral radiograph of the chest, do not have true and definite fascial planes. In addition, several disorders that may present as mediastinal masses cross boundaries or arise in multiple compartments. Nonetheless, the practice of assigning a mediastinal mass to a specific mediastinal compartment is still useful because such a method enables one to formulate a manageable differential diagnosis and effectively direct further imaging workup, and it yields valuable information, particularly for surgical planning.
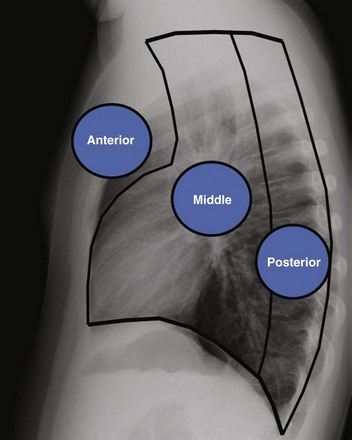
Figure 58-6 Anatomic landmarks demarcating the anterior, middle, and posterior compartments of the mediastinum labeled on a lateral chest radiograph.
Anterior indicates the anterior mediastinal compartment, Middle indicates the middle mediastinal compartment, and Posterior indicates the posterior mediastinal compartment.
Anterior Mediastinal Masses
Congenital Abnormalities of the Thymus:
Etiology: The thymus is a bilobed organ that serves as the site of T-cell maturation. The thymus develops from the third pharyngeal pouch. It begins a process of caudal and ventromedial elongation during the seventh and eighth week of gestation whereby the two sides fuse at about the level of the aortic arch. Partial failure of descent may result in ectopic thymic tissue in the neck or superior mediastinum. Absence of the thymus is a component of DiGeorge syndrome,31 with an incidence of 1 per 2000 to 4000.32–34
Imaging: The appearance of the thymus on frontal chest radiographs is variable and largely dependent on the age of the patient (Fig. 58-7).5,35,36 The thymus is prominent in size with a quadrilateral shape and convex margins during infancy (Fig. 58-8). After approximately the fifth year of life, the thymus becomes more triangular in shape with straight margins (e-Fig. 58-9). By the age of 15 years, the margins of the thymus are either straight or concave (Fig. 58-10). Absent thymic tissue in pediatric patients with DiGeorge syndrome is usually evident on chest radiographs in infants and young children. However, an atrophic thymus due to a stress response may appear similarly.37,38 The clinical context is often helpful in distinguishing these two conditions without the need for cross-sectional studies.
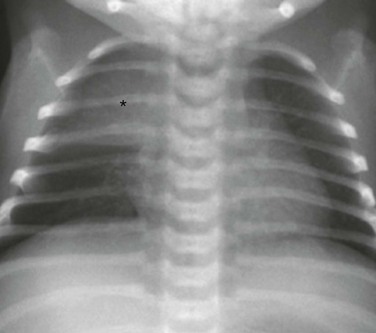
Figure 58-7 A normal thymus in a female neonate.
The frontal chest radiograph shows a thymic sail sign, which is created by the right lobe of the thymus (asterisk) abutting the minor fissure.

Figure 58-8 A normal thymus in a 5-month-old girl.
An axial enhanced computed tomography image at the level of the aortic arch shows the expected appearance of the thymus (asterisk) in the anterior mediastinal compartment at this age. The thymus has a quadrilateral shape and a convex margin. It is homogeneous in attenuation without an associated cystic, calcific, or fat component.
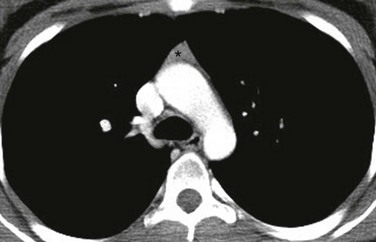
Figure 58-10 A normal thymus in an adolescent boy.
An axial enhanced computed tomography image at the level of the aortic arch shows the expected appearance of the thymus (asterisk) in the anterior mediastinal compartment at this age. The thymus has a triangular shape with a straight margin.
Treatment and Follow-up: Treatment of DiGeorge syndrome is targeted to the associated defects such as hypocalcemia, frequent infections, and conotruncal cardiac defects. Because DiGeorge syndrome is a component of the 22q11 deletion syndrome, many patients with this syndrome also have velocardiofacial syndrome.39
Normal Variants of the Thymus:
Etiology: The two most common anatomic variants of the thymus are either superior or posterior extension of the normal thymus (e-Fig. 58-11 and Fig. 58-12). These variants usually are seen before 2 years of age. The thymus may extent superiorly to the level of the lower neck40,41 or posteriorly to the middle or posterior mediastinal compartment.42,43 The posterior extension of the thymus typically is posterior to the superior vena cava on the right or the aortic arch on the left. After puberty, the thymus undergoes slow involution. During stress, a rapid transient decrease in the size of the gland occurs, and it regains its original size after the offending mechanism (e.g., intubation, surgery, or chemotherapy) is withdrawn—the so-called thymic rebound.38,44
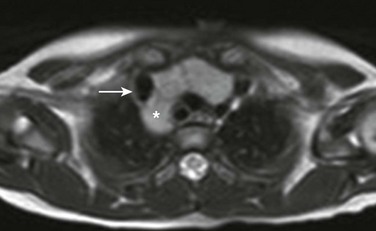
Figure 58-12 Posterior thymic extension as a normal variant in a 1-year-old boy.
An axial T2-weighted magnetic resonance image at the level of the brachiocephalic vein shows posterior extension (asterisk) of the thymus behind the superior vena cava (arrow).
e-Figure 58-11 Normal superior extension of thymic tissue into the neck.
On this gated axial (A), oblique (B), mildly T1-weighted magnetic resonance images, the thymus is clearly distinguished from vessels. It is of intermediate signal intensity—less than fat but greater than muscle. Note how far cephalad to the innominate vein (I) the thymic tissue extends (arrows). C, superior vena cava; T, trachea; LA, left atrium.
Imaging: An ectopic thymus rarely presents as a mass and is most commonly discovered incidentally as thymic tissue extension on cross-sectional imaging with similar signal characteristics and density as the orthotopic thymus on magnetic resonance imaging (MRI) and CT, respectively (see e-Fig. 58-11 and Fig. 58-12). Occasionally, however, retrocaval thymus may be mistaken for a mediastinal mass on radiographs. With superior mediastinal extension, the diagnosis may be made with ultrasound using a high-frequency linear array transducer. The ectopic thymus should exhibit homogenous echotexture with internal bright specular reflections, similar to the orthotopic thymus.45 Further, contiguity with the orthotopic thymus may be demonstrated on ultrasound. The appearance of rebound thymus on chest radiographs may be impressive in terms of degree and rapidity of development. Any displacement or compression of adjacent airway or vessels by the thymus should raise suspicion for a neoplasm.
Etiology: A thymic cyst is a rare, fluid-filled lesion typically representing a cystic remnant of the thymopharyngeal duct.38,46 Although a thymic cyst can occur anywhere from the pyriform sinus to the anterior mediastinum, it is most commonly found in the lateral infrahyoid neck region.47 A fibrous cord may connect the thymic cyst to the mediastinal thymus. When the cyst is large, affected pediatric patients present with a slowly enlarging neck mass that may be associated with respiratory compromise, dysphagia, or vocal cord paralysis. Although most thymic cysts are derived from a remnant of the thymopharyngeal duct, thymic cysts also have been described in patients infected with human immunodeficiency virus and in patients with Langerhans cell histiocytosis involving the thymus.48,49 Cysts in the latter group may feature small calcifications.50
Imaging: Thymic cysts appear as a spherical, fluid-filled lesion or as multilocular cystic spaces with a thin wall. The thymic cyst is usually occult on chest radiographs. In infants and young children, ultrasound may confirm the fluid-filled nature of the mass. On CT and MRI, thymic cysts typically present as a nonenhancing cystic mass (e-Fig. 58-13). The MR signal of a thymic cyst is variable depending on whether the contents are proteinaceous and/or hemorrhagic. The differential diagnosis of a thymic cyst in pediatric patients includes branchial cleft cyst, lymphatic malformation, thyroglossal duct cyst, dermoid cyst, bronchogenic cyst, and teratoma.
Etiology: A thymolipoma is an uncommon benign thymic mass composed of both thymic and mature adipose tissue. Thymolipomas account for approximately 2% to 9% of all thymic neoplasms.38,51 The presumed underlying etiologies include a variant of a thymoma, hyperplasia of mediastinal fat, and a neoplasm of mediastinal fat that encases thymic tissue.51,52 Affected patients typically are asymptomatic because a thymolipoma is very soft and pliable, exerting little mass effect.
Imaging: On chest radiographs, a thymolipoma may present as a low-density lesion because of its underlying fatty component. On cross-sectional imaging studies, thymolipomas are characterized by an enlarged thymus with areas of low attenuation (on CT) and high signal intensity (on T2-weighted MRI) in a whorled pattern representing the underlying fatty component (Fig. 58-14).
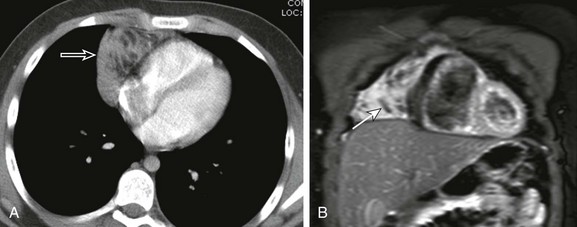
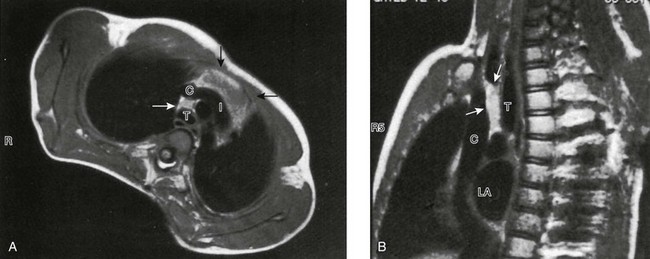
Figure 58-14 A thymolipoma in an 8-year-old girl.
A, An axial enhanced computed tomography image at the level of the mid heart shows an anterior mediastinal mass (arrow) with whorls of low attenuating regions consistent with fat. B, A coronal fluid-sensitive magnetic resonance imaging sequence with fat saturation shows the linear low signal fatty striations (arrow) through the mass.
Etiology: Thymomas arise from the thymic epithelial cells and account for approximately 1% to 2% of anterior mediastinal masses in the pediatric population.47,53 Thymomas traditionally are classified into two types (i.e., noninvasive or invasive thymoma) depending on the presence of well-defined margins without extension through its fibrous capsule. Because thymomas may be locally invasive but typically do not metastasize, many authorities prefer the term “invasive thymoma” rather than “malignant thymoma.” Similar to adult patients with thymoma, about 15% to 30% of affected pediatric patients present with myasthenia gravis.48,54,55 Other associated autoimmune conditions include pure red cell aplasia and hypogammaglobulinemia.54,55
Imaging: On chest radiographs, a thymoma usually appears as an ovoid mass that occasionally is associated with thin peripheral capsular calcification located within the anterior mediastinum. Pleural nodules also may be seen in patients with an invasive thymoma. Cross-sectional imaging studies typically show an enlarged and homogeneous anterior mediastinal soft tissue mass sometimes associated with an area of low attenuation representing underlying cystic necrosis (Fig. 58-15)47 Imaging findings suggestive of invasive-type thymoma include irregular margins, obliterated adjacent mediastinal fat planes, or extension to the pleura or chest wall. A search for these imaging features is particularly important, because the histology between invasive and noninvasive type thymoma is similar, apart from surgical evidence of capsular extension.

Figure 58-15 A thymoma in a 15-year-old girl.
An axial enhanced computed tomography image at the level of the main pulmonary artery shows a large bulky thymus with irregular margins, heterogeneity, and areas of internal low attenuation (asterisk). Although the effect of the mass is seen, including posterior displacement of the bronchus intermedius and right sided atelectasis (Rt), no evidence is seen of vascular or soft tissue invasion.
Etiology: A thymic carcinoma is an aggressive epithelial tumor of the thymus characterized by overt cellular atypia. Thymic carcinomas are rare in the pediatric population; they usually occur in adults during the fifth or sixth decade.56 Affected pediatric patients most often present with chest pain and constitutional symptoms including fatigue, weight loss, and night sweats.47 A paraneoplastic phenomenon such as myasthenia gravis is uncommon with a thymic carcinoma, in contradistinction to a thymoma.57,58 Metastatic disease or invasion is detected in most new diagnoses.58,59 Prognosis is poor.
Imaging: On imaging studies, a thymic carcinoma typically presents as a large anterior mediastinal mass with irregular margins, heterogeneous contrast enhancement, and local invasion of adjacent mediastinal structures (Fig. 58-16). Calcification and areas of necrosis are common.60 Although differentiation from a thymoma is difficult, features such as local invasion of adjacent structures, lymphadenopathy, and metastasis favor the diagnosis of a thymic carcinoma over a thymoma.
Etiology: Lymphoma results from abnormal proliferation of lymphocytes, which are cells that are a component of the immune system. Lymphoma is the most common cause of mediastinal masses in the pediatric population. It also is the third most common group of malignancies after leukemia and central nervous system tumors in the pediatric population.5 Lymphoma accounts for approximately 46% to 56% of all mediastinal masses.5 Lymphoma is traditionally classified into two types: non-Hodgkin lymphoma and Hodgkin lymphoma. These two types of lymphoma have many similarities, including their appearance on imaging, but because of their many important differences, especially in clinical behavior, they are discussed separately in the following sections. Pulmonary involvement by lymphoma is discussed in Chapter 55.
Non-Hodgkin lymphoma typically occurs in pediatric patients who are younger than 5 years. It more frequently affects boys than girls by a ratio of 3 : 1.5 The four main types of non-Hodgkin lymphoma include (1) lymphoblastic or T cell (the most common type); (2) Burkitt; (3) non-Burkitt; and (4) large cell or histiocytic. Pediatric patients with lymphoblastic or T-cell type non-Hodgkin lymphoma commonly present with a mediastinal mass. Although large cell or histiocytic types may involve either the thorax or the abdomen, Burkitt and non-Burkitt types nearly always present in the abdomen. In general, more than one third of patients with non-Hodgkin lymphoma present with a mediastinal mass.62 Pediatric patients often present with clinical symptoms related to obstruction or compression related to adjacent mediastinal airways and vascular structures.
Hodgkin lymphoma is rare in younger children and occurs with increasing frequency in children older than 5 years.5 It more frequently affects boys than girls by a ratio of 2 : 1.5 Hodgkin lymphoma is divided into four main types based on the relative amounts of lymphocytes and Reed-Sternberg cells and the type of connective tissue proliferation: (1) nodular sclerosing; (2) mixed cellularity; (3) lymphocyte depletion; and (4) lymphocyte predominant. Among these four types of Hodgkin lymphoma, the nodular sclerosing type (the most common subtype) accounts for approximately 75%5,63 of mediastinal masses in children. Although affected pediatric patients may present with asymptomatic cervical or axillary lymphadenopathy on physical examination, the majority of them present with chest pain and discomfort. Shortness of breath or wheezing should suggest underlying airway compression. More suggestive clinical symptoms of Hodgkin lymphoma include weight loss, night sweats, and unexplained fevers.
Imaging: Hodgkin lymphoma may present as bulky hilar nodes or an anterior mediastinal mass on chest radiographs (Fig. 58-17, A and B), although the chest radiographs may be entirely normal in the setting of minimal lymphadenopathy. When Hodgkin lymphoma is suspected, a contrast-enhanced CT scan of the chest should be performed to confirm the presence of a mass or enlarged nodes and to characterize its extent for disease staging (Fig. 58-17, C).64,65 Common nodes involved in persons with Hodgkin lymphoma include the superior prevascular and pretracheal nodes. The appearance of affected nodes can range anywhere between small lymph nodes to large, conglomerate nodular masses that fill in the mediastinum and displace adjacent structures. The presence of calcifications before treatment is rare.47 On MRI, signal characteristics of Hodgkin lymphoma are variable but usually are intermediate on T1-weighted images and have an increased signal on T2-weighted images. However, MRI generally plays no additionally useful role in the diagnosis or workup of Hodgkin lymphoma. Positron emission tomography (PET) and/or PET/CT scans are now widely used and have been well validated in the literature for evaluating adult patients with lymphoma.66–68 Although fewer studies have been conducted with pediatric patients, a growing body of evidence suggests very high accuracy of these modalities in children, especially when they are compared with CT used alone.69–71
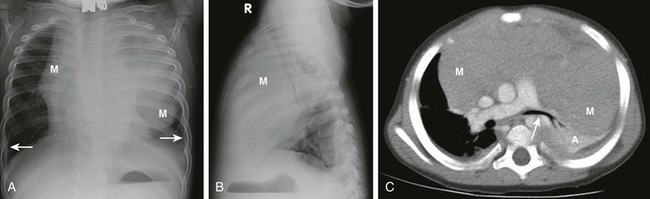
Figure 58-17 Hodgkin lymphoma in a 2-year-old girl.
A, A frontal chest radiograph shows a large mediastinal mass (M) with lobulated and bulky margins. Small pleural effusions (arrows) also are present. B, A lateral chest radiograph confirms that the location of this mass (M) is within the anterior mediastinal compartment. C, An axial enhanced computed tomography image at the level of the right pulmonary artery shows a large anterior mediastinal mass (M) with effect of the mass showing on the left main stem bronchus (arrow). Left-sided atelectasis (A) is present.
Non-Hodgkin lymphoma is more variable than Hodgkin lymphoma with regard to its sites of disease predilection because it often may arise in the abdomen, thorax, or head/neck regions. When non-Hodgkin lymphoma occurs in the thorax (in about 50% of cases47), its most common appearance is that of a large anterior mediastinal mass on chest radiographs (Fig. 58-18, A). As with any anterior mediastinal mass, such imaging findings should prompt a CT scan, which typically shows discrete or conglomerate mediastinal lymph nodes (Fig. 58-18, B). After the administration of contrast, areas of heterogeneity and low-density necrosis are a frequent finding, particularly within the large masses. Because the lesion infiltrates or arises from the thymus, the mass can be confused with an enlarged, normal thymus in young children. Differentiating imaging features include unusually lobular, bulky borders, heterogeneity, and displacement of adjacent structures such as airway or vessels—features that a normal thymus should never have. Hilar, subcarinal, and posterior nodal chain involvement frequently is present. In contradistinction to Hodgkin lymphoma, pleural disease may be present, manifesting as pleural-based masses or effusion.47 MRI may be useful in the evaluation of sites beyond the anterior mediastinum, including the chest wall. As with Hodgkin lymphoma, PET or combined PET/CT can assist in staging. PET is particularly helpful in discriminating between a viable tumor versus a scar, detecting active disease in “normal”-sized nodes on CT, and searching for extranodal disease such as in the liver, spleen, and kidneys. Pitfalls of interpretation include the presence of increased metabolic activity in the thymus and brown fat.72,73
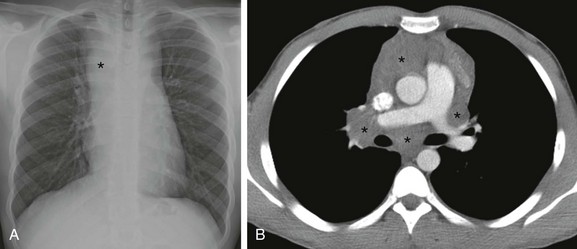
Figure 58-18 Non-Hodgkin lymphoma in an 8-year-old girl.
A, A frontal chest radiograph shows a mediastinal mass (asterisk). B, An axial enhanced computed tomography image at the level of the pulmonary artery shows a mediastinal mass (asterisks) located within the mediastinum. Note both the anterior, subcarinal, and hilar components.
Treatment and Follow-up: The prognosis of lymphoma in pediatric patients depends on the type and stage. The prognosis of Hodgkin lymphoma, which has a cure rate of approximately 90%,47,74 is better than that of non-Hodgkin lymphoma, for which the cure rate among pediatric patients is 80%.75 Currently, multiple chemotherapeutic treatment regimens are used in combination with radiation therapy to treat pediatric patients with lymphoma. In pediatric patients with non-Hodgkin lymphoma, a bone marrow transplant also is an option.
Etiology: Lymphatic malformation represents a congenital malformation of lymphatic channels, lined by single layer endothelium.76 It typically occurs in the cervical region (often posterior to the sternocleidomastoid muscle) but may extend caudally into the superior and/or anterior mediastinum. Lymphatic malformation currently is classified into two types, macrocystic or microcystic, depending on the size of the cysts, although mixed lesions comprising both forms are common. Outdated terms include cystic hygroma and lymphangioma (for the macro and micro forms, respectively); use of these terms should be avoided. The term lymphatic malformation adheres to the currently recommended nomenclature of the International Society for the Study of Vascular Anomalies.77 Lymphatic malformations may “grow” as more lymph fills the sacs. Lymphatic malformations typically present early in life as a palpable, pliable soft tissue mass and grow commensurate with the patient’s growth. Sudden enlargement also may occur if they undergo hemorrhage (from the vascularized intervening septae) or become infected.
Imaging: Plain radiographs have little role in the evaluation of lymphatic malformations. However, a lymphatic malformation may first be noted as a mediastinal opacity and enlargement (Fig. 58-19, A). CT can suggest the diagnosis, but because of proteinaceous debris and/or internal hemorrhage, the density may be higher than would be expected for simple fluid (Fig. 58-19, B). Because associated calcification is rare, the presence of calcification on CT should suggest an alternate diagnosis. MRI is superb for the evaluation of the lymphatic malformations because of its excellent capability for soft tissue characterization and multiplanar imaging assessment. The septa with the lymphatic malformation are particularly well visualized on MRI and may enhance as they are vascularized. The cystic components should not enhance. Because of proteinaceous debris and/or blood products within the lymphatic malformation, variability exists in T1 and T2 signal intensities on MRI. Fluid/fluid levels are common and strongly support the diagnosis of lymphatic malformation.
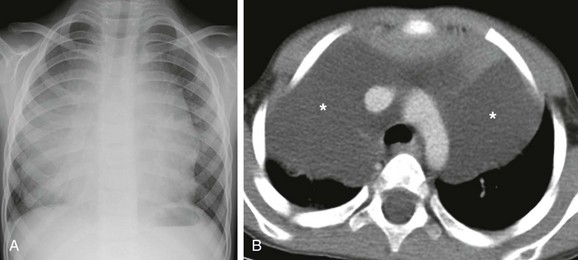
Figure 58-19 Mediastinal lymphatic malformation in a 1-year-old boy.
A, A frontal chest radiograph shows a large mediastinal mass. B, An axial enhanced computed tomography image at the level of the aortic arch shows a large, predominantly anterior mediastinal mass (asterisks) of fluid attenuation that crosses midline and extends laterally, consistent with a macrocystic lymphatic malformation.
Treatment and Follow-up: Because there is no known risk of malignant transformation of lymphatic malformation, some controversy exists with regard to treating smaller asymptomatic lesions. If treatment is elected, both surgery and/or percutaneous sclerotherapy currently are used in management. The macrocystic-type lymphatic malformation is particularly well suited for sclerotherapy. Laser therapy is another option for more superficially accessible lesions (typically of the microcystic-type lymphatic malformation).78
Etiology: Germ cell tumors usually arise from the testes or ovaries. However, primitive germ cell rests may reside in the mediastinum and give rise to neoplasms.79,80 Primary mediastinal germ cell tumors account for 6% to 18% of anterior mediastinal tumors in children,65 and 60% of these tumors are teratomas.47 The teratomas usually are further divided into mature and immature types, with the latter being malignant. Of all mediastinal germ cell tumors, 14% are malignant.81 Infants with teratomas tend to present with airway compression, whereas older children often are asymptomatic.5 Other symptoms include sudden onset of pain, dyspnea, or cough. The tumor can even rupture into the tracheobronchial tree or pleural space with expectoration or deposition of its contents.5
Imaging: On chest radiographs, germ cell tumors typically appear as round, sharply demarcated anterior mediastinal masses. Calcifications occur in approximately 25% to 53% of teratomas5,46,47,82 and may be seen on radiographs. As for most anterior mediastinal masses, CT can better characterize their extent and may allow definitive diagnosis. Typically, teratomas (both mature and immature) demonstrate fat, fluid, and calcifications, which, when seen, allow a confident diagnosis (Fig. 58-20). However, approximately 15% of mature teratomas display no fat or calcium on imaging.5 Although calcifications may be difficult to detect on MRI, the intralesional fat and fluid are seen readily. Invasion of adjacent structures (as opposed to mere displacement) is suggestive of malignant, immature tumors.
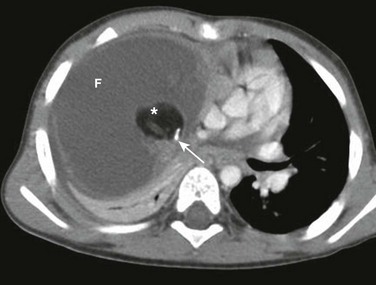
Figure 58-20 A teratoma in a 2-year-old girl.
An axial enhanced computed tomography image at the level of the heart shows a large, right-sided, anterior and middle mediastinal mass, largely of fluid attenuation (F) with a well-defined plug of fat density (asterisk) and internal calcification (arrow). The surgical pathology confirmed the diagnosis of a mediastinal mature and benign teratoma.
Middle Mediastinal Masses
Etiology: Foregut duplication cysts arise from developmental malformations of the embryonic foregut and are of three main types: bronchogenic, esophageal, and neurenteric cysts. Bronchogenic cysts develop from errors in lung budding during development of the ventral foregut during the first trimester. Errors in development of the posterior division of the embryonic foregut may result in an esophageal duplication cyst. Neurenteric cysts arise from a failure of complete separation between the gastrointestinal tract and the primitive neural crest during early embryonic life and represent one form of the split notochord syndrome. The distinction among these three types of foregut duplication cysts can be made histologically by demonstrating either respiratory, gastrointestinal, or mixed neural/gastrointestinal lining, respectively. Together, these three account for 11% of all mediastinal masses in children.65
Imaging: Chest radiographs often show an oval or round-shaped middle mediastinal mass (e-Fig. 58-21, A). In cases of a neurenteric cyst, an accompanying vertebral anomaly also may be present. The position of the cyst in the mediastinum suggests its type. Bronchial duplication cysts typically are located within the middle mediastinum. Esophageal duplication cysts are in the middle or posterior mediastinum. Neurenteric cysts most often are in the posterior mediastinum but are discussed here because they fall into the same differential. Cross-sectional imaging studies typically demonstrate a nonenhancing, fluid-filled cystic mass with well-marginated borders (e-Fig. 58-21, B). Internal proteinaceous material can increase the Hounsfield units on CT and signal intensity on T1-weighted MRI. The high water content usually results in adequate T2 prolongation to reveal its cystic nature on T2-weighted MRI when CT density is equivocal. On both CT and MRI, foregut duplication cysts should lack internal enhancement and appear homogeneous unless superimposed infection is present.
e-Figure 58-21 Esophageal duplication cyst in a 4-year-old boy.
The surgical pathology confirmed the diagnosis of the esophageal duplication cyst. A, A lateral view of the esophagus obtained during a barium esophagram study shows a smooth-bordered focal anterior indentation consistent with an extraluminal mass (asterisk) centered between the trachea and esophagus. B, An axial enhanced computed tomography image at the level of the carina shows a fluid density middle mediastinal mass (asterisk).
Treatment and Follow-up: The current management choice of foregut duplication cyst is complete surgical resection, particularly in symptomatic pediatric patients. In some institutions, endoscopic ultrasound-guided fine-needle aspiration is used to preoperatively confirm the imaging diagnosis.83 This procedure is generally considered safe, although reports have been made of complications such as infection.84
Etiology: Lymphadenopathy may occur in any mediastinal compartment but is most prevalent in the middle mediastinum. Most enlarged mediastinal lymph nodes in children are reactive. Children with cystic fibrosis frequently demonstrate prominent mediastinal nodes. Particularly prominent hilar lymph nodes may be seen in the setting of granulomatous diseases such as Mycobacterium tuberculosis, Mycobacterium avium-intracellulare, Histoplasmosis, or sarcoidosis.
Imaging: Lymphadenopathy often is first detected on chest radiographs. The presence of hilar involvement, bilaterality, and calcification should be investigated carefully. Most commonly, except when acute infection is the suspected cause, a CT scan is subsequently obtained for further evaluation after chest radiographs. Intravenous contrast always should be administered except when it is medically contraindicated, because lymph nodes on CT may be confused with vessels. MRI may be helpful in selected cases but is seldom needed. On T1-weighted MRI sequences, nodes are isointense to muscle and are hyperintense on T2-weighted sequences and are easily distinguished from adjacent vessels.
Calcified lymph nodes suggest a history of treated lymphoma or the presence of granulomatous disease such as Mycobacterium tuberculosis, Histoplasmosis capsulatum, or sarcoidosis. Low-density or centrally necrotic nodes should suggest Mycobacterium tuberculosis (Fig. 58-22)85 or Mycobacterium avium-intracellulare.86,87 Sarcoidosis may occur in children but is rare. Large hilar lymphadenopathy also has been described in persons with lymphoma, infectious mononucleosis, and Castleman disease (angiofollicular lymphoid hyperplasia) (e-Fig. 58-23).

Figure 58-22 Primary Mycobacterium tuberculosis in a 2-year-old boy.
The sputum culture confirmed the diagnosis of Mycobacterium tuberculosis infection. A, A frontal chest radiograph shows right hilar and infrahilar opacity. In addition, the distal trachea has a slight leftward deviation, suggesting an effect of the mass. B, An axial enhanced computed tomography (CT) image demonstrates low attenuation hilar, infrahilar, and subcarinal lymphadenopathy (asterisks). C, A coronal enhanced CT image shows a narrowing of the left main stem bronchus (arrow) as a result of a large mediastinal lymphadenopathy (asterisks).
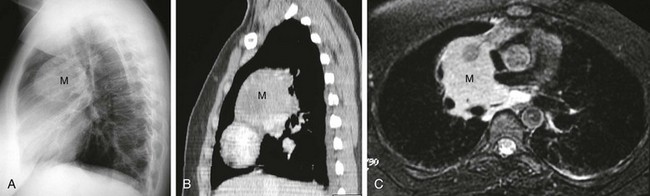
e-Figure 58-23 Castleman disease in a 17-year-old girl.
A, A lateral chest radiograph shows a large middle mediastinal mass (M). B, A sagittal enhanced computed tomography image demonstrates a homogeneously enhancing middle mediastinal mass (M). C, An axial magnetic resonance image with a fluid-sensitive sequence shows a middle mediastinal mass (M) with homogeneously high signal intensity.
Posterior Mediastinal Masses
Etiology: The vast majority (88%) of masses arising in the posterior mediastinum are of neurogenic origin and together account for about 34% of all mediastinal masses in children.65 Ganglion cells in the paravertebral sympathetic chain and peripheral nerve sheaths within the posterior mediastinum are responsible for most of posterior mediastinal neurogenic masses. Sympathetic chain tumors are more common than nerve sheath tumors in the pediatric mediastinum.
Tumors arising from the sympathetic chain include neuroblastomas, ganglioneuroblastomas, and ganglioneuromas, in order of increasing cellular differentiation and increasing age of presentation. These tumors are related by their structure of origin but are distinguished by their underlying histologic cellular differentiation. The least differentiated (and hence most malignant) and most common of these tumors is the neuroblastoma, which usually arises in children younger than 5 years. About 10% to 16% of all neuroblastomas arise in the mediastinum. Clinical manifestations of neuroblastoma include constitutional symptoms and several paraneoplastic syndromes. However, presentations that are unique to the mediastinal location of neuroblastoma include Horner syndrome if the mass involves the superior mediastinum. Still, many children with thoracic neuroblastoma present with incidentally discovered masses on chest or abdominal radiographs. Seventy-six percent of thoracic neuroblastomas are positive for urinary catecholamines.88
Imaging: Most posterior mediastinal neurogenic tumors are first detected on chest radiographs as a soft tissue opacity (Figs. 58-24 and 58-25). Associated adjacent bone destruction or scalloping in addition to silhouetting of posterior mediastinal structures such as the descending aorta also may be seen. Assessment of calcification is of paramount importance because its presence suggests a sympathetic chain tumor such as a neuroblastoma as opposed to a nerve sheath tumor.
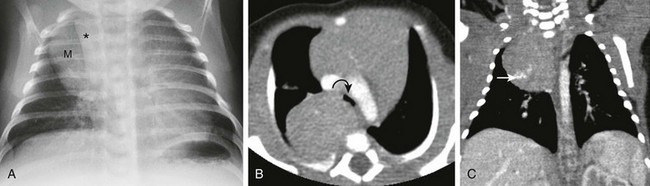
Figure 58-24 A neuroblastoma in a 1-year-old boy.
The surgical pathology confirmed the diagnosis of neuroblastoma. A, A frontal chest radiograph shows a right upper mediastinal mass (M) that does not silhouette the anterior vascular structures such as the superior vena cava (asterisk). No bony changes are evident. B, An axial enhanced computed tomography (CT) image at the level of the aortic arch shows a large, right posterior, mediastinal, paravertebral mass with effect of the mass against the carina (curved arrow). C, A coronal enhanced CT image shows a large right upper paravertebral mass extending into the right apex with calcifications (arrow).
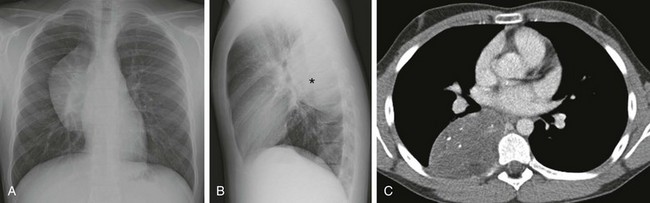
Figure 58-25 A ganglioneuroma in a 13-year-old boy.
The surgical pathology confirmed the diagnosis of ganglioneuroma. A, A frontal chest radiograph shows a mediastinal mass without silhouetting of either the cardiac border or the right hilus, which is seen through the mass. B, A lateral chest radiograph confirms that the mass (asterisk) is centered posteriorly within the posterior mediastinal compartment. C, An axial enhanced computed tomography image at the level of the left atrium/pulmonary veins shows the right paravertebral posterior mediastinal mass with punctate internal calcification.
On CT, posterior mediastinal neurogenic tumors typically present as soft tissue masses with a varying degree of contrast enhancement (see Figs. 58-24 and 58-25). Approximately 40% of neuroblastomas in the posterior mediastinum show speckled or curvilinear calcification.5 Twenty percent of ganglioneuroblastomas have calcification.5 Nerve sheath tumors typically do not calcify. Further characterization and differentiation among different types of posterior mediastinal neurogenic tumors with CT is limited.
In contradistinction to anterior and middle mediastinal masses, MRI is currently the best imaging modality for evaluating posterior mediastinal tumors in pediatric patients because of its high sensitivity for detecting the intraspinal (extradural) extension that often is found with these tumors without ionizing radiation exposure.65 Moreover, MRI offers exquisite soft tissue contrast, which is an advantage when assessing a region such as the posterior mediastinum with similar soft tissue densities and minimal fat. Finally, MRI is sensitive for assessing bone marrow involvement.
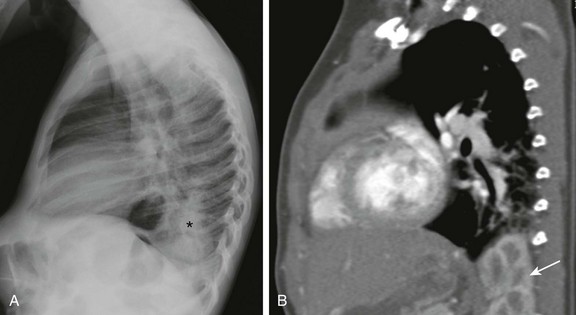
Nerve sheath tumors appear as sharply demarcated, rounded, or elliptic paravertebral masses in the posterior mediastinum. Whereas neuroblastomas course along several vertebral bodies, nerve sheath tumors usually are localized to one or two intervertebral spaces. However, plexiform neurofibromas can involve multiple levels and extend into the middle mediastinum. On T2-weighted imaging, plexiform neurofibromas have a distinct high signal periphery with an intermediate signal centrally—the so-called “target” appearance (Fig. 58-26). Associated findings include thoracic dural ectasia and scalloping of the posterior vertebral bodies.
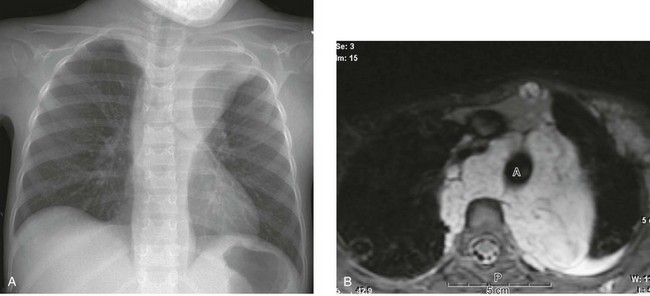
Figure 58-26 Neurofibromatosis type 1 in a 6-year-old boy who presented with cough.
A, A frontal chest radiograph shows a large left apical and paraspinal mass that cascades down each side of the spine. B, An axial T2-weighted image demonstrates the “target sign” and the lobulated shape of the plexiform neurofibromas. The multilayered lobules of the neurofibromas appear as targets. A, Aorta; P, paraspinal muscle.
Treatment and Follow-up: Sympathetic chain neurogenic tumors are treated entirely differently from nerve sheath tumors because the sympathetic chain tumors are considered malignant (although to a varying degree depending on their cellular differentiation). Chemotherapy usually is initiated after a histologic diagnosis is rendered and surgical resection is performed for sympathetic chain neurogenic tumors. Radiation therapy generally has no role in treating sympathetic chain neurogenic tumors.5 The prognosis depends on the patient’s age. Younger patients (particularly infants) have a far better prognosis than older children. Overall, patients with a thoracic neuroblastoma have a better prognosis than patients with retroperitoneal disease.47 Patients with benign nerve sheet tumors such as neurofibromatosis type 1 do not undergo routine resection of their masses. However, imaging surveillance may be used because of risks of malignant transformation and other tumors arising de novo.
Other Posterior Mediastinal Lesions and Lesions Simulating Posterior Mediastinal Masses:
Etiology: Benign masses and even lung parenchymal processes may mimic one of the more sinister posterior mediastinal masses. For example, in a patient with severe, long-standing anemia, extramedullary sites of hematopoiesis include the posterior mediastinal paravertebral space.89 Rarely, the posterior mediastinum may be the site of ectopic structures such as diaphragmatic hernias, both congenital and acquired. These structures may contain not only bowel loops but retroperitoneal structures such as kidneys (e-Fig. 58-27). Ectopic thymic extension into the posterior mediastinal compartment was discussed previously in the section on normal variants of thymus in this chapter. Cystic structures in the posterior mediastinum may be from neuroenteric cysts, esophageal duplication cysts (both of which are discussed in the section on middle mediastinal masses in this chapter), or from meningoceles, which usually are associated with neurofibromatosis type 1. Finally, pulmonary airspace disease, which is seen through the mediastinal structures on chest radiographs, may mimic a mediastinal mass or vice versa.
e-Figure 58-27 Superior herniation of a kidney into the chest in a 1-year-old boy.
A, A lateral chest radiograph shows an opacity (asterisk) with obscuration of the posterior left hemidiaphragm. B, A sagittal enhanced computed tomography image demonstrates that the opacity seen on the lateral chest radiograph (A) is caused by upward herniation of the kidney (arrow) through a Bochdalek hernia.
Imaging: A focus of hematopoietic tissue is most often seen in a paravertebral position as abnormal smooth or lobulated soft tissue. Other clues such as bone marrow reconversion or evidence of sickle cell disease may suggest the diagnosis. An airspace consolidation such as that seen with pneumonia may mimic a posterior mediastinal mass, particularly when it is seen in the lower lobes medially and obscures posterior mediastinal structures such as the descending aorta and/or azygoesophageal fissure on a frontal chest radiograph. Conversely, a posterior mediastinal mass such as a neuroblastoma may be confused with lung consolidation, particularly when it occurs in the upper lobes. Ectopic intraabdominal structures such as the bowel, kidney, pancreas, and spleen may be seen in the posterior mediastinum with a large diaphragmatic hernia. The hernia is usually obvious, particularly if air-filled loops of bowel are present. In confusing cases, reconstructed thin-section CT in the coronal plane is useful.
Lee, EY. Evaluation of non-vascular mediastinal masses in infants and children: an evidence-based practical approach. Pediatr Radiol. 2009;39(suppl 2):S184–S190.
Lee, EY. Imaging evaluation of mediastinal masses in infants and children. In: Medina LS, Applegate KE, Blackmore CC, eds. Evidence-based imaging in pediatrics: optimizing imaging in pediatric patient care. New York: Springer-Verlag, 2010.
Nasseri, F, Effekhari, F. Clinical and radiologic review of the normal and abnormal thymus: pearls and pitfalls. Radiographics. 2010;30(2):413–428.
Toma, P, Granata, C, Rossi, A, et al. Multimodality imaging of Hodgkin disease and non-Hodgkin lymphomas in children. Radiographics. 2007;27(5):1335–1354.
Zylak, CM, Standen, JR, Barnes, GR, et al. Pneumomediastinum revisited. Radiographics. 2000;20(4):1043–1057.
References
1. Bejvan, SM, Godwin, JD. Pneumomediastinum: old signs and new signs. AJR Am J Roentgenol. 1996;166:1041–1048.
2. Johnson, NN, Toledo, A, Endom, EE. Pneumothorax, pneumomediastinum, and pulmonary embolism. Pediatr Clin North Am. 2010;57:1357–1383.
3. Macklin, MT, Macklin, CC. Malignant interstitial emphysema of the lungs and mediatinum as an important occult complication in many respiratory diseases and other conditions: an interpretation of the clinical literature in the light of laboratory experiments. Medicine. 1944;23:281–358.
4. Macklin, CC. Transport of air along sheaths of pulmonic blood vessels from alveoli to mediastinum: clinical implications. Arch Intern Med. 1939;64:913–926.
5. Kuhn, JP, Slovis, TL, Haller, JO, et al. Caffey’s pediatric diagnostic imaging, 10th ed. Philadelphia: Mosby Elsevier; 2004.
6. Zylak, CM, Standen, JR, Barnes, GR, et al. Pneumomediastinum revisited. Radiographics. 2000;20:1043–1057.
7. Eesa, M, Kandpal, H, Sharma, R, et al. Spontaneous pneumorrhachis in bronchial asthma. Acta Radiol. 2006;47:672–674.
8. McLoud, TC. Thoracic radiology. St Louis: Mosby–Year Book; 1998.
9. Gander, JW, Berdon, WE, Cowles, RA. Iatrogenic esophageal perforation in children. Pediatr Surg Int. 2009;25:395–401.
10. Amodio, JB, Berdon, WE, Abramson, SJ, et al. Retrocardiac pneumomediastinum in association with tracheal and esophageal perforations. Pediatr Radiol. 1986;16:380–383.
11. Ylmaz, S, Oren, H, Irken, G, et al. Life-threatening mediastinal-retroperitoneal hemorrhage in a child with moderate hemophilia A and high inhibitor titer: successful management with recombinant activated factor VII. J Pediatr Hematol Oncol. 2005;27:400–402.
12. Bees, NR, Richards, SW, Fearne, C, et al. Neonatal thymic haemorrhage. Br J Radiol. 1997;70:210–212.
13. Woolley, MM, Isaacs, H, Jr., Lindesmith, G, et al. Spontaneous thymic hemorrhage in the neonate: report of two cases. J Pediatr Surg. 1974;9:231–233.
14. Urvoas, E, Pariente, D, Rousset, A, et al. Ultrasound diagnosis of thymic hemorrhage in an infant with late-onset hemorrhagic disease. Pediatr Radiol. 1994;24:96–97.
15. Akman, C, Kantarci, F, Cetinkaya, S. Imaging in mediastinitis: a systematic review based on aetiology. Clin Radiol. 2004;59:573–585.
16. Katabathina, VS, Restrepo, CS, Martinez-Jimenez, S, et al. Nonvascular, nontraumatic mediastinal emergencies in adults: a comprehensive review of imaging findings. Radiographics. 2011;31:1141–1160.
17. Kirchner, SG, Hernanz-Schulman, M, Stein, SM, et al. Imaging of pediatric mediastinal histoplasmosis. Radiographics. 1991;11:365–381.
18. David, RA, Weiner, MA, Rakow, JI. Chronic active mediastinitis in a 7-year-old boy: MRI findings. Pediatr Radiol. 1996;26:669–671.
19. Atasoy, C, Fitoz, S, Erguvan, B, et al. Tuberculous fibrosing mediastinitis: CT and MRI findings. J Thorac Imaging. 2001;16:191–193.
20. Restrepo, CS, Martinez, S, Lemos, DF, et al. Imaging appearances of the sternum and sternoclavicular joints. Radiographics. 2009;29:839–859.
21. Santos Gorjon, P, Blanco Perez, P, Morales Martin, AC, et al. Deep neck infection. Review of 286 cases. Acta Otorrinolaringol Esp. 2012;63:31–41.
22. Kono, T, Kohno, A, Kuwashima, S, et al. CT findings of descending necrotising mediastinitis via the carotid space (“Lincoln Highway”). Pediatr Radiol. 2001;31:84–86.
23. Kumar, S, Kumar, V, Bishnoi, A, et al. Non-traumatic anterior mediastinal abscess in childhood. J Indian Assoc Pediatr Surg. 2011;16:75–77.
24. Argenta, LC, Morykwas, MJ, Marks, MW, et al. Vacuum-assisted closure: state of clinic art. Plast Reconstr Surg. 2006;117:127S–142S.
25. Athanassiadi, KA. Infections of the mediastinum. Thorac Surg Clin. 2009;19:37–45. [vi].
26. Devaraj, A, Griffin, N, Nicholson, AG, et al. Computed tomography findings in fibrosing mediastinitis. Clin Radiol. 2007;62:781–786.
27. Rodriguez, E, Soler, R, Pombo, F, et al. Fibrosing mediastinitis: CT and MR findings. Clin Radiol. 1998;53:907–910.
28. Witschi, M, Gugger, M, Nicod, LP. Treatment of mediastinal fibrosis with mycophenolate mofetil. Respiration. 2009;78:330–333.
29. Mole, TM, Glover, J, Sheppard, MN. Sclerosing mediastinitis: a report on 18 cases. Thorax. 1995;50:280–283.
30. Sherrick, AD, Brown, LR, Harms, GF, et al. The radiographic findings of fibrosing mediastinitis. Chest. 1994;106:484–489.
31. Johnson, JM, Moonis, G, Green, GE, et al. Syndromes of the first and second branchial arches, part 2: syndromes. AJNR Am J Neuroradiol. 2011;32:230–237.
32. Fomin, AB, Pastorino, AC, Kim, CA, et al. DiGeorge syndrome: a not so rare disease. Clinics (Sao Paulo). 2010;65:865–869.
33. Shprintzen, RJ. Velo-cardio-facial syndrome: 30 years of study. Dev Disabil Res Rev. 2008;14:3–10.
34. McDonald-McGinn, DM, Sullivan, KE. Chromosome 22q11.2 deletion syndrome (DiGeorge syndrome/velocardiofacial syndrome). Medicine (Baltimore). 2011;90:1–18.
35. Silverman, FN. A la recherche du temps perdu and the thymus (with apologies to Marcel Proust). Radiology. 1993;186:310–311.
36. Mandell, GA, Bellah, RD, Boulden, ME, et al. Cervical trachea: dynamics in response to herniation of the normal thymus. Radiology. 1993;186:383–386.
37. Caffey, J, Di Liberti, C. Acute atrophy of the thymus induced by adrenocorticosteroids: observed roentgenographically in living infants: a preliminary report. Am J Roentgenol Radium Ther Nucl Med. 1959;82:530–540.
38. Nasseri, F, Eftekhari, F. Clinical and radiologic review of the normal and abnormal thymus: pearls and pitfalls. Radiographics. 2010;30:413–428.
39. Gennery, AR. Immunological aspects of 22q11.2 deletion syndrome. Cell Mol Life Sci. 2012;69:17–27.
40. Castellote, A, Vazquez, E, Vera, J, et al. Cervicothoracic lesions in infants and children. Radiographics. 1999;19:583–600.
41. Spinner, RJ, Moore, KL, Gottfried, MR, et al. Thoracic intrathymic thyroid. Ann Surg. 1994;220:91–96.
42. Kuhn, JP. Re: normal thymus extending between the right brachiocephalic vein and the innominate artery. AJR Am J Roentgenol. 1996;167:1592.
43. Slovis, TL, Meza, M, Kuhn, JP. Aberrant thymus—MR assessment. Pediatr Radiol. 1992;22:490–492.
44. Caffey, J, Silbey, R. Regrowth and overgrowth of the thymus after atrophy induced by the oral administration of adrenocorticosteroids to human infants. Pediatrics. 1960;26:762–770.
45. Song, I, Yoo, SY, Kim, JH, Hong, E, Yoon, HK. Aberrant cervical thymus: imaging and clinical findings in 13 children. Clin Radiol. 2011;66:38–42.
46. Jeung, MY, Gasser, B, Gangi, A, et al. Imaging of cystic masses of the mediastinum. Radiographics. 2002;22:S79–S93.
47. Ranganath, SH, Lee, EY, Restrepo, R, et al. Mediastinal masses in children. AJR Am J Roentgenol. 2012;198:W197–W216.
48. Leonidas, JC. The thymus: from past misconception to present recognition. Pediatr Radiol. 1998;28:275–282.
49. Leonidas, JC, Berdon, WE, Valderrama, E, et al. Human immunodeficiency virus infection and multilocular thymic cysts. Radiology. 1996;198:377–379.
50. Heller, GD, Haller, JO, Berdon, WE, et al. Punctate thymic calcification in infants with untreated Langerhans’ cell histiocytosis: report of four new cases. Pediatr Radiol. 1999;29:813–815.
51. Rosado-de-Christenson, ML, Pugatch, RD, Moran, CA, et al. Thymolipoma: analysis of 27 cases. Radiology. 1994;193:121–126.
52. Hudacko, R, Aviv, H, Langenfeld, J, et al. Thymolipoma: clues to pathogenesis revealed by cytogenetics. Ann Diagn Pathol. 2009;13:185–188.
53. Carretto, E, Inserra, A, Ferrari, A, et al. Epithelial thymic tumours in paediatric age: a report from the TREP project. Orphanet J Rare Dis. 2011;6:28.
54. Liang, X, Lovell, MA, Capocelli, KE, et al. Thymoma in children: report of 2 cases and review of the literature. Pediatr Dev Pathol. 2010;13:202–208.
55. Rocha, MM, Neves, PD, Rodrigues, CC, et al. Invasive thymoma in a child: a rare case report. J Pediatr Surg. 2012;47:e23–e25.
56. Moore, S, Dave-Verma, H, Singh, A. Imaging of mediastinal tumors. Cancer Treat Res. 2008;143:145–175.
57. Truong, LD, Mody, DR, Cagle, PT, et al. Thymic carcinoma. A clinicopathologic study of 13 cases. Am J Surg Pathol. 1990;14:151–166.
58. Jung, KJ, Lee, KS, Han, J, et al. Malignant thymic epithelial tumors: CT-pathologic correlation. AJR Am J Roentgenol. 2001;176:433–439.
59. Ogawa, K, Toita, T, Uno, T, et al. Treatment and prognosis of thymic carcinoma: a retrospective analysis of 40 cases. Cancer. 2002;94:3115–3119.
60. Eng, TY, Fuller, CD, Jagirdar, J, et al. Thymic carcinoma: state of the art review. Int J Radiat Oncol Biol Phys. 2004;59:654–664.
61. Stachowicz-Stencel, T, Bien, E, Balcerska, A, et al. Thymic carcinoma in children: a report from the Polish Pediatric Rare Tumors Study. Pediatr Blood Cancer. 2010;54:916–920.
62. Franco, A, Mody, NS, Meza, MP. Imaging evaluation of pediatric mediastinal masses. Radiol Clin North Am. 2005;43:325–353.
63. Piccaluga, PP, Agostinelli, C, Gazzola, A, et al. Pathobiology of Hodgkin lymphoma. Adv Hematol. 2011;2011:920898.
64. Tomiyama, N, Honda, O, Tsubamoto, M, et al. Anterior mediastinal tumors: diagnostic accuracy of CT and MRI. Eur J Radiol. 2009;69:280–288.
65. Lee, EY. Evaluation of non-vascular mediastinal masses in infants and children: an evidence-based practical approach. Pediatr Radiol. 2009;39(suppl 2):S184–S190.
66. Feeney, J, Horwitz, S, Gonen, M, et al. Characterization of T-cell lymphomas by FDG PET/CT. AJR Am J Roentgenol. 2010;195:333–340.
67. Rankin, S. [(18)F]2-fluoro-2-deoxy-D-glucose PET/CT in mediastinal masses. Cancer Imaging. 2010;10(Spec No A):S156–S160.
68. Hutchings, M. PET imaging in lymphoma. Expert Rev Hematol. 2009;2:261–276.
69. Riad, R, Omar, W, Kotb, M, et al. Role of PET/CT in malignant pediatric lymphoma. Eur J Nucl Med Mol Imaging. 2010;37:319–329.
70. Bakhshi, S, Radhakrishnan, V, Sharma, P, et al. Pediatric nonlymphoblastic non-Hodgkin lymphoma: baseline, interim, and posttreatment PET/CT versus contrast-enhanced CT for evaluation—a prospective study. Radiology. 2012;262:956–968.
71. Hudson, MM, Krasin, MJ, Kaste, SC. PET imaging in pediatric Hodgkin’s lymphoma. Pediatr Radiol. 2004;34:190–198.
72. Hong, TS, Shammas, A, Charron, M, et al. Brown adipose tissue 18F-FDG uptake in pediatric PET/CT imaging. Pediatr Radiol. 2011;41:759–768.
73. Gawande, RS, Khurana, A, Messing, S, et al. Differentiation of normal thymus from anterior mediastinal lymphoma and lymphoma recurrence at pediatric PET/CT. Radiology. 2012;262:613–622.
74. Juweid, ME, Vose, JM. Imaging in early-stage Hodgkin’s lymphoma. N Engl J Med. 2010;362:962.
75. Hamrick-Turner, JE, Saif, MF, Powers, CI, et al. Imaging of childhood non-Hodgkin lymphoma: assessment by histologic subtype. Radiographics. 1994;14:11–28.
76. Puri, P, Höllwarth, ME. Pediatric surgery. Berlin: Springer; 2009.
77. Enjolras, O, Wassef, M, Chapot, R. Color atlas of vascular tumors and vascular malformations. Cambridge: Cambridge University Press; 2007.
78. Greene, AK, Perlyn, CA, Alomari, AI. Management of lymphatic malformations. Clin Plast Surg. 2011;38:75–82.
79. Jaggers, J, Balsara, K. Mediastinal masses in children. Semin Thorac Cardiovasc Surg. 2004;16:201–208.
80. Moran, CA, Suster, S. Primary germ cell tumors of the mediastinum: I. Analysis of 322 cases with special emphasis on teratomatous lesions and a proposal for histopathologic classification and clinical staging. Cancer. 1997;80:681–690.
81. Billmire, D, Vinocur, C, Rescorla, F, et al. Malignant mediastinal germ cell tumors: an intergroup study. J Pediatr Surg. 2001;36:18–24.
82. Totanarungroj, K, Watcharaporn, C, Muangman, N. Helpful CT findings for giving specific diagnosis of anterior mediastinal tumors. J Med Assoc Thai. 2010;93:489–496.
83. Wildi, SM, Hoda, RS, Fickling, W, et al. Diagnosis of benign cysts of the mediastinum: the role and risks of EUS and FNA. Gastrointest Endosc. 2003;58:362–368.
84. Diehl, DL, Cheruvattath, R, Facktor, MA, et al. Infection after endoscopic ultrasound-guided aspiration of mediastinal cysts. Interact Cardiovasc Thorac Surg. 2010;10:338–340.
85. Andreu, J, Caceres, J, Pallisa, E, et al. Radiological manifestations of pulmonary tuberculosis. Eur J Radiol. 2004;51:139–149.
86. Suwatanapongched, T, Gierada, DS. CT of thoracic lymph nodes. Part II: diseases and pitfalls. Br J Radiol. 2006;79:999–1000.
87. Pursner, M, Haller, JO, Berdon, WE. Imaging features of Mycobacterium avium-intracellulare complex (MAC) in children with AIDS. Pediatr Radiol. 2000;30:426–429.
88. Adams, GA, Shochat, SJ, Smith, EI, et al. Thoracic neuroblastoma: a Pediatric Oncology Group study. J Pediatr Surg. 1993;28:372–377. [discussion 7-8].
89. Ejindu, VC, Hine, AL, Mashayekhi, M, et al. Musculoskeletal manifestations of sickle cell disease. Radiographics. 2007;27:1005–1021.