6 Orbit / Lids / Adnexa
Anatomy
Dimensions
Orbit
pear-shaped (widest diameter is 1 cm posterior to orbital rim); 40 mm wide, 35 mm high, 45 mm deep, volume = 30 cc (Table 6-1)
| Orbit | Bones | Related structures/miscellaneous |
|---|---|---|
| Roof | Sphenoid (lesser wing) | Lacrimal gland fossa |
| Frontal | Trochlea | |
| Supraorbital notch (medial) | ||
| Lateral wall | Sphenoid (greater wing) | Lateral orbital tubercle of Whitnall |
| Zygomatic | Strongest orbital wall | |
| Lateral orbital rim at equator of globe | ||
| Floor | Maxilla | Contains infraorbital nerve and canal |
| Palatine | Forms roof of maxillary sinus | |
| Zygomatic | ||
| Medial wall | Sphenoid | Lacrimal sac fossa |
| Maxilla | Adjacent to ethmoid and sphenoid sinuses | |
| Ethmoid | Posterior ethmoidal foramen | |
| Lacrimal | Weakest orbital wall |
Optic nerve
orbital length = 25–30 mm; length from globe to optic foramen = 18 mm; width = 1.5 mm in globe, 3.5 mm posterior to lamina cribrosa (due to myelin), 5.0 mm with the addition of the optic nerve sheath (see Figure 4-2)
Proptosis
| Mean (mm) | Upper Limit of Normal (mm) | |
|---|---|---|
| Caucasian male | 16.5 | 21.7 |
| Caucasian female | 15.4 | 20 |
| African American male | 18.5 | 24.7 |
| African American female | 17.8 | 23.0 |
Apertures
(Figures 6-1 to 6-3)
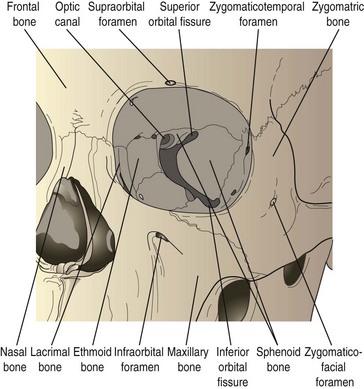
Figure 6-1 Bony anatomy of the orbit in frontal view.
(From Dutton JJ: Atlas of Clinical and Surgical Orbital Anatomy, Philadelphia, WB Saunders, 1994.)
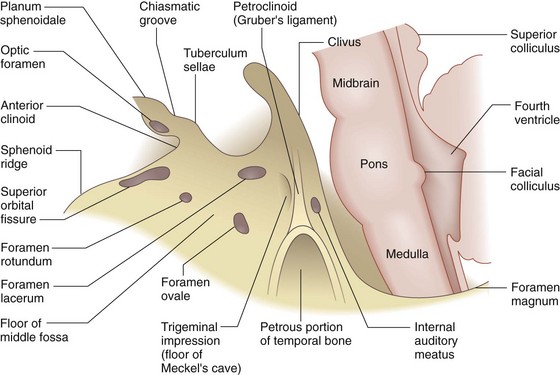
Figure 6-3 Schematic representation of the landmarks, temporal view.
(From Bajandas FJ, Kline BK: Neuro-Ophthalmology Review Manual, Thorofare, NJ, Slack, 1988.)
Inferior orbital fissure
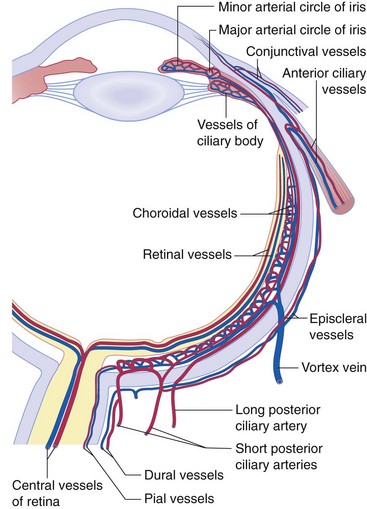
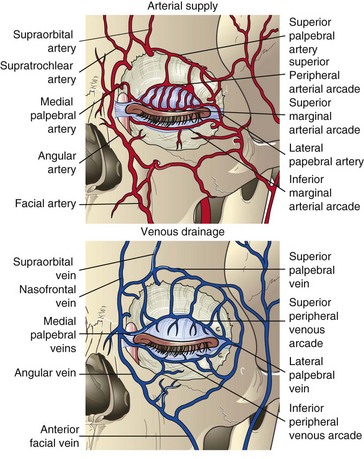
Vascular Supply to Eye
(Figures 6-4 to 6-6)
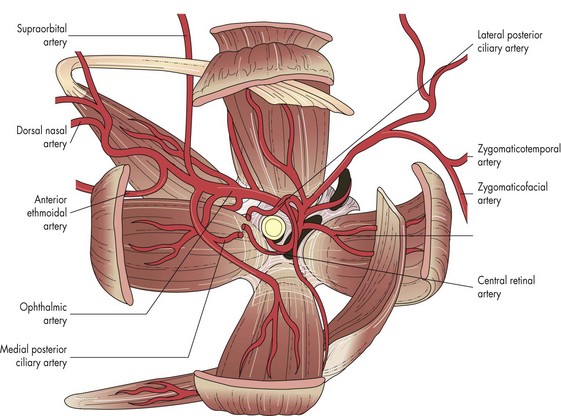
Figure 6-4 Arterial supply to the orbit, in coronal view.
(From Dutton JJ: Atlas of Clinical and Surgical Orbital Anatomy, Philadelphia, WB Saunders, 1994.)
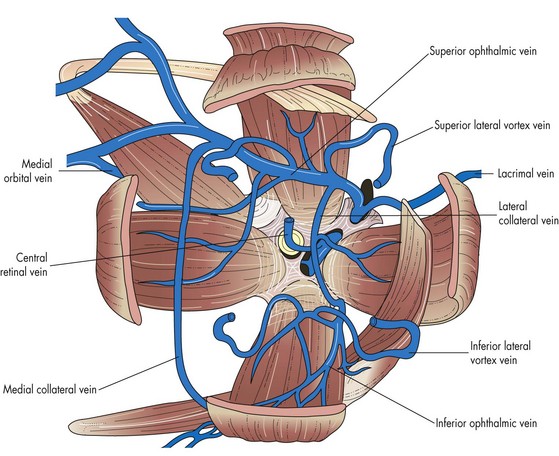
Figure 6-5 Orbital veins. Venous drainage from the orbit, in coronal view.
(From Dutton JJ: Atlas of Clinical and Surgical Orbital Anatomy, Philadelphia, WB Saunders, 1994.)
Ophthalmic artery
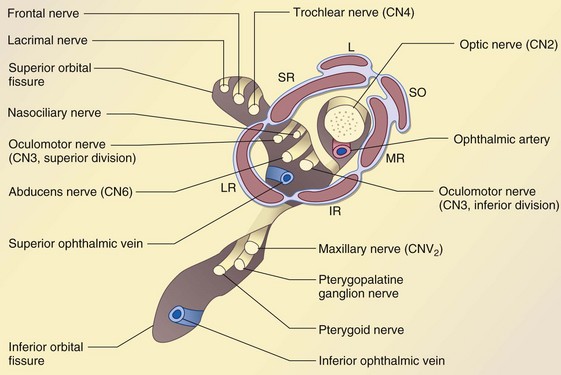
Innervation of Eye
Sensory innervation provided by ophthalmic and maxillary division of trigeminal nerve (CN 5) (Figure 6-7)
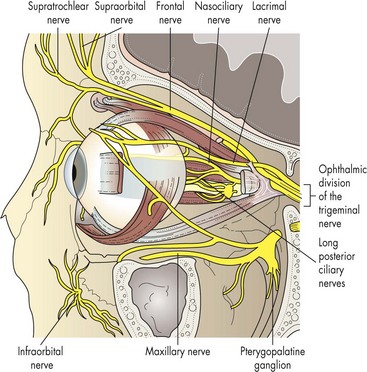
Figure 6-7 Sensory nerves of the orbit, in lateral view.
(From Dutton JJ: Atlas of Clinical and Surgical Orbital Anatomy, Philadelphia, WB Saunders, 1994.)
Sinuses
Soft Tissues
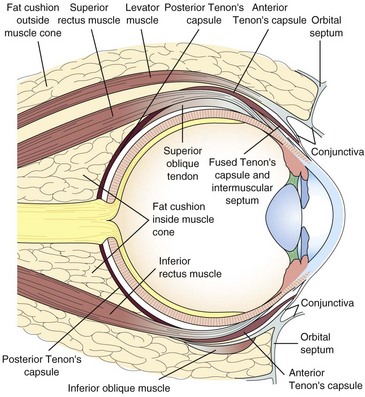
Figure 6-9 Sagittal section of orbital tissues through the vertical recti.
(Adapted from Parks MM: Extraocular muscles. In Duane TD Clinical Ophthalmology, Philadelphia, Harper and Row, 1982.)
Adipose tissue
Eyelid
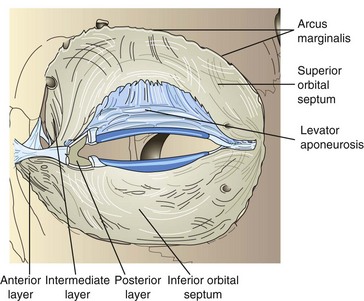
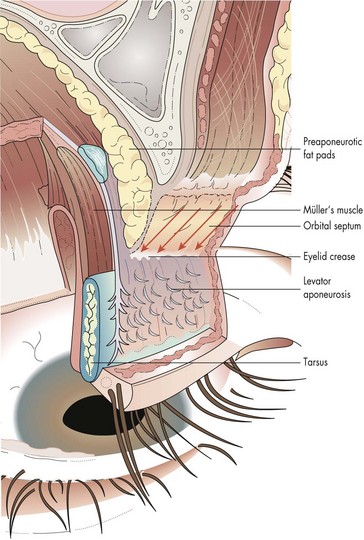
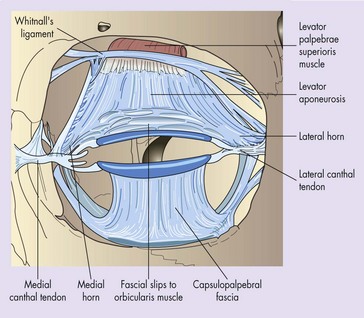
Lamellae of upper eyelid: (Figure 6-10)
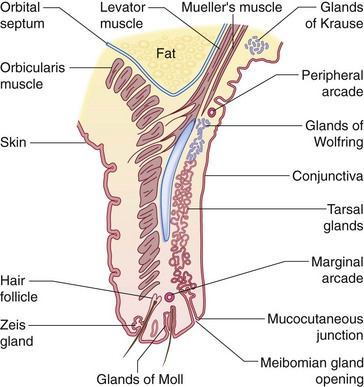
Figure 6-10 Cross section of upper eyelid. Note position of cilia, tarsal gland orifices, and mucocutaneous junction.
(Reprinted with permission from Grand MG: Basic and Clinical Science Course, Section 2: Fundamentals and Principles of Ophthalmology. American Academy of Ophthalmology, San Francisco, 1993.)
Skin
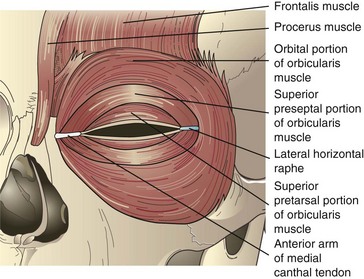
Orbicularis oculi: (Figure 6-11)
Other muscles of forehead and eyebrow
Orbital septum
Upper eyelid retractors
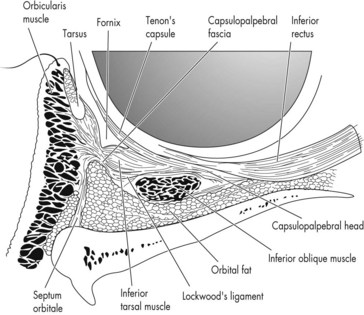
Lower eyelid retractors
Medial canthal tendon
Eyelid margin
Vascular supply
Nasolacrimal System
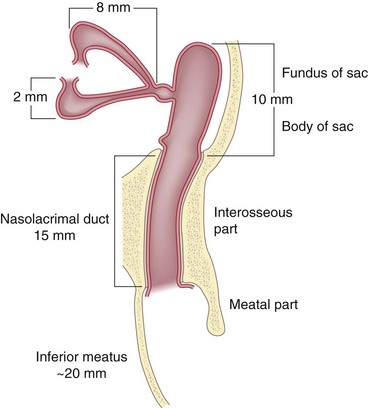
Figure 6-17 Excretory lacrimal system.
(From Grand MG: Basic and Clinical Science Course, Section 2, Fundamentals and Principles of Ophthalmology, San Francisco, American Academy of Ophthalmology, 1993.)
Imaging
Ultrasound
Optimal sound wave frequency is 10 MHz
Higher frequencies give better resolution; lower frequencies provide better penetration (Table 6-4)
| Good sound transmission | Poor sound transmission |
|---|---|
| Cavernous hemangioma | Metastatic cancer |
| Lymphangioma | Orbital pseudotumor |
| Mucocele | Glioma |
| Dermoid | Neurofibroma |
| High Reflectivity | Low Reflectivity |
| Neurofibroma | Metastatic cancer |
| Fresh hemorrhage | Orbital pseudotumor |
| Hemangioma | Cyst |
| Thyroid eye disease | Mucocele |
| Varix | |
| Dermoid | |
| Lymphoma |
MRI
Radiofrequency pulse disturbs the alignment by energizing protons or neutrons
Can provide axial, coronal, and sagittal views
Relaxation times
CT Scan
Disadvantages
poor posterior fossa detail; no sagittal sections, ionizing radiation
| Most common orbital lesions with well-circumscribed appearance on CT and MRI | Most common orbital lesions with Ill-defined appearance on CT and MRI |
|---|---|
| Children: | Children: |
| Dermoid cyst | Capillary hemangioma |
| Lymphangioma | Orbital pseudotumor |
| Rhabdomyosarcoma | Plexiform neurofibroma |
| ON glioma | Leukemic infiltrate |
| Eosinophilic granuloma | |
| Adults: | Adults: |
| Cavernous hemangioma | Orbital pseudotumor |
| Neurofibroma | Metastasis |
| Neurilemmoma | Leukemic infiltrate |
| Fibrous histiocytoma | Primary malignant tumor |
| (Lymphoproliferative disorders) | Lymphoproliferative disorders |
Orbital Disorders
Trauma
Orbital Fractures
Fractures of orbital bones, often associated with ocular or intracranial injuries
Orbital floor (blow-out)
Zygomatic (tripod)
Intraorbital Foreign Bodies
Commonly associated with intraocular and / or optic nerve injury
Inert material can be well tolerated and may be observed
Copper and organic material are poorly tolerated and must be removed
Often asymptomatic, but may have pain or decreased vision
CT scan (MRI is contraindicated for metallic foreign bodies)
Degeneration
Infections
Fungal
Mucormycosis
Inflammation
Idiopathic Orbital Inflammation (Orbital Pseudotumor)
Idiopathic inflammatory disease of orbital tissues
Children
bilateral in 33%; commonly have headache, fever, vomiting, and lethargy; may have associated papillitis or iritis; work up usually not needed (see Ch. 5, Pediatrics / Strabismus)
Diagnosis
Orbital myositis
localized to extraocular muscles MR and LR most commonly involved (33% each), IR 10%
Thyroid-Related Ophthalmopathy
Autoimmune disease with spectrum of ocular manifestations
Most common cause of unilateral or bilateral proptosis in adults
Most common cause of acquired diplopia in adults
Women affected 8–10× more often than men
Associated with myasthenia gravis (in 5% of patients with Graves’ disease)
Pathology
enlargement of extraocular muscles; patchy infiltrates of lymphocytes, monocytes, mast cells, and fibroblasts; fibroblasts produce mucopolysaccharides, which leads to increased water content of muscles; inflammation spares tendons (Figure 6-18)
Treatment
Sarcoidosis
Chronic, idiopathic, multisystem, granulomatous disease primarily affecting lung, skin, eye
Vascular Abnormalities
AV Fistula
Direct carotid-cavernous sinus fistula
Tumors
| In Children (see Chapter 5, Pediatrics/Strabismus) | In Adults |
|---|---|
| 90% are benign; 10% are malignant | Mucocele |
| Rhabdomyosarcoma (most common primary orbital malignancy) | Cavernous hemangioma |
| Capillary hemangioma (most common benign orbital tumor) | Meningioma |
| Lymphangioma | Fibrous histiocytoma |
| Neuroblastoma (most common metastatic orbital tumor) | Neurilemmoma |
| Dermoid (most common orbital mass) | Pleomorphic adenoma (BMT) |
| Teratoma | Lymphoid tumors |
| ON glioma | Metastatic tumors |
| Granulocytic sarcoma (‘chloroma’) | |
| Burkitt’s lymphoma | |
| Histiocytic tumors |
Vascular Tumors
Cavernous Hemangioma
Most common benign orbital tumor in adults (usually middle-aged women)
Pathology
encapsulated lesion composed of blood-filled cavernous spaces, lined by endothelial cells (Figure 6-19)
Neural Tumors
Neurilemmoma (Schwannoma)
Encapsulated tumor consisting of benign proliferation of Schwann cells
Occurs in middle-aged individuals
Lesion can be painful due to perineural spread and compression of nerve
Usually located in the superior orbit causing gradual proptosis and globe dystopia
Schwannomas can grow along any peripheral or cranial nerve, most commonly CN 8 (acoustic neuroma)
Rarely associated with neurofibromatosis
Pathology
Meningioma
Lymphoid Tumors
Spectrum of disorders characterized by abnormal proliferation of lymphoid tissue
20% of all orbital tumors; 90% are non-Hodgkins B-cell lymphoma
Usually occur in adults 50–70 years old; rare in children
Conjunctival or lacrimal gland lesions
Tissue biopsy with immunohistochemical studies required for diagnosis
Perform every 6 months for 2 years
Bone marrow biopsy (better than bone marrow aspirate)
Benign Reactive Lymphoid Hyperplasia
Orbital Lymphoma
Pathology
atypical immature lymphocytes with mitoses; diffuse or follicular growth; monoclonal B-cell proliferations 60–90% with scattered or reactive T cells; involves reticuloendothelial system, including retroperitoneal lymph nodes (Figure 6-22)
Fibro-osseous Tumors
Osteoma
Dense bony lesions originating in the frontal and ethmoid sinus
Well-circumscribed, slow-growing mass
Symptoms secondary to sinus obstruction and intracranial or intraorbital extension
Fibrous Histiocytoma
Firm orbital mass composed of fibroblasts and histiocytes
Usually benign (malignant in 10%)
Distinguished from hemangiopericytoma only on biopsy
Epithelial Lacrimal Gland Tumors
50% of lacrimal gland lesions are inflammatory and lymphoproliferative; contour around the globe
50% of lacrimal gland tumors are of epithelial origin
50% of epithelial tumors are benign pleomorphic adenomas
50% of malignant tumors are adenoid cystic carcinomas
Pleomorphic Adenoma (Benign Mixed Tumor)
Most common epithelial tumor of the lacrimal gland
Occurs in 4th–5th decade of life
Firm mass in lacrimal fossa with painless proptosis; globe often displaced medially and downward
Progressive expansile growth may indent bone of lacrimal fossa
Tumor growth stimulates periosteum to deposit a thin layer of new bone (cortication)
Adenoid Cystic Carcinoma
Most common malignant tumor of the lacrimal gland
Presents in 4th decade of life
Rapidly progressive proptosis, pain and paresthesia due to perineural invasion and bony destruction
Sinus Tumors
Sinus Mucocele
Cystic, slowly expanding sinus lesion
Entrapment of mucus in aerated space due to obstruction of sinus ostia
Exerts pressure on surrounding bony structures
May become infected (mucopyocele)
Associated with cystic fibrosis
Must rule out encephalocele and meningocele
Metastatic Tumors
In contrast to adults, pediatric tumors metastasize to the orbit more frequently than to the uvea
Orbital metastases produce rapid painful proptosis with restricted ocular motility
Eyelid Disorders
Trauma
Lid Laceration
Partial- or full-thickness cut in eyelid that may involve the lid margin, canthus, or canaliculus
Inflammation
Hordeolum
Painful erythematous eyelid swelling
Accumulation of secretions causes acute inflammatory response
Lipogranuloma formation (chalazion) often evolves from internal hordeolum
Acne Rosacea
Idiopathic, chronic skin disorder affecting sebaceous glands of face (including meibomian glands)
Type IV hypersensitivity may play a role
Infections
Molluscum Contagiosum
Shiny, white-yellow papule with central umbilication
Spread by direct contact; consider HIV in healthy adult
Verruca Vulgaris (Papilloma)
Pink, pedunculated or sessile mass
Malposition and Other Disorders
Blepharospasm
Etiology unknown but may be due to abnormality of basal ganglia
Usually occurs in 5th–7th decade of life; female > male (3 : 1); associated with Parkinson’s disease
Treatment
Blepharoptosis (Acquired)
Eyelid malposition characterized by drooping upper eyelid
Mechanical
due to mass effect of orbital or eyelid tumors, dermatochalasis, blepharochalasis, cicatrix
Examination
Ectropion
Eversion of eyelid margin; may cause keratinization and hypertrophy of conjunctiva
Entropion
Lower eyelid entropion usually involutional
Upper eyelid entropion usually cicatricial
Spastic
associated with ocular inflammation, trauma, and prolonged patching
Involutional
Cicatricial
shortening of posterior lamella
Trichiasis
Misdirection of eyelashes and contact with ocular surface
Eyelid Tumors
Benign Epithelial Tumors
Squamous Papilloma
Keratinized epidermal fronds with fibrovascular cores
Most common benign lesion of eyelid
Associated with papovavirus (HPV) infection
Cysts
Epithelial lined chambers filled with debris
Epidermal Inclusion Cyst (Epidermoid Cyst)
Occurs after a fragment of epidermis is carried into the subepithelium by trauma
Trapped but viable epithelium proliferates and produces keratin
Dermoid Cyst
Contains keratin, cilia, and sebum
Sebaceous Gland Tumors
Tumors of Hair Follicle Origin
Trichofolliculoma
A keratin-filled dilated cystic hair follicle, surrounded by immature hair follicles
Appears as a small umbilicated nodule usually with central white hairs
Tricholemmoma
Small crusty lesion with rough ulcerated surface
Arises from glycogen-rich clear cells of the outer hair sheath
Pilomatrixoma (‘Calcifying Epithelioma of Malherbe’)
Solitary, firm, deep nodule with overlying normal, pink, or bluish skin
Freely movable subcutaneous pink-purple nodule
Most common cystic lesion of childhood
In young adult, arises from hair matrix of upper lid or brow
Occurs on the eyelid, face, neck, or arms
Can range from 5 to 30 mm in diameter
Precancerous Lesions
Actinic Keratosis
Most common precancerous lesion
Occurs in middle-aged individuals
Scaly, white, flat-topped lesion with surrounding erythema
Common on face, eyelid, and scalp
Nevus
Congenital or acquired hamartoma
Can be flat, but is usually elevated and pigmented
Arises from neural crest cells
Pigmentation and size tend to increase during puberty
With time, nevi tend to move deeper, migrating into the dermis
Contains benign-appearing dermal melanocytes
Malignant transformation is rare
Compound nevus
both intradermal and junctional components (Figure 6-31); slightly elevated or papillomatous, often pigmented
Malignant Epithelial Tumors
Basal Cell Carcinoma (BCC)
Most common malignancy of the eyelid (90%)
40 times more common than squamous cell carcinoma
Develops on sun-exposed skin in elderly patients; smoking is also a risk
Location (in order of frequency)
lower lid (50–60%), medial canthus (20–30%), upper lid (15%), outer canthus (5%)
Morbidity and mortality occur from local invasion of skull and CNS
Squamous Cell Carcinoma (SCC)
Flat, keratinized, ulcerated, erythematous plaque
Can arise de novo or from preexisting actinic keratosis
May spread by direct extension or may metastasize via local lymphatics or hematogenously
May be associated with HIV and HPV infection
More aggressive than basal cell carcinoma
Keratoacanthoma
Rapid onset (4–8 weeks); occurs in elderly
Central keratin-filled crater and elevated rolled edges; clinically resembles basal cell carcinoma
May cause permanent damage to lid margin and madarosis (loss of lashes)
Sebaceous Adenocarcinoma
Second most common malignancy of the eyelid (after BCC)
Occurs in the elderly (6th–7th decade of life)
Arises from meibomian glands, glands of Zeis, and glands of caruncle
Upper lid more commonly involved (greater number of meibomian glands)
Can masquerade and be misdiagnosed as a recurrent chalazion or chronic blepharitis
Often associated with madarosis
Pathology
lobules of anaplastic cells with foamy, lipid-laden, vacuolated cytoplasm, large hyperchromic nuclei, skip areas and pagetoid invasion (spread of tumor into conjunctival epithelium), positive lipid stains (oil-red-O stain) (Figure 6-36)
Malignant Melanoma (MM)
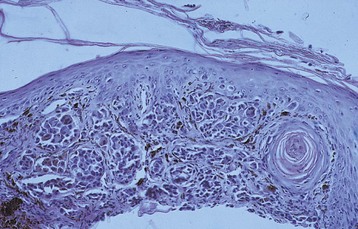
Figure 6-37 Malignant melanoma.
(From Yanoff M, Fine BS: Ocular Pathology, 5th edn, St Louis, Mosby, 2002.)
Superficial spreading melanoma (80%)
Neurogenic Tumors
Neurilemmoma (Schwannoma)
Solitary eyelid nodule composed of Schwann cells
Vascular Tumors
Cavernous Hemangioma
Appears as a port wine stain (nevus flammeus)
Other Lesions
Xanthelasma
Soft, flat or slightly elevated yellow plaques
More common on the medial aspect of the eyelids
Nasolacrimal System Disorders
Obstructions
Acquired tearing
Nasolacrimal Duct Obstruction
Infections
Canaliculitis
Dacryocystitis
Tumors of the Lacrimal Sac
Orbital Surgery
Review Questions (answers start on page 363)
American Academy of Ophthalmology. Orbit, Eyelids and Lacrimal System, vol 7. San Francisco: AAO; 2012.
Bosniak SL. Principles and Practice of Ophthalmic Plastic and Reconstructive Surgery. Philadelphia: WB Saunders; 1996.
Collin JRO. Manual of Systematic Eyelid Surgery, 3rd edn. Philadelphia: Butterworth-Heinemann; 2002.
Dutton JS. Atlas of Clinical and Surgical Orbital Anatomy, 2nd edn. Philadelphia: Saunders; 2011.
Levine MR. Manual of Oculoplastic Surgery, 4th edn. Thorofare: SLACK; 2010.
, Chen and Kahn: Color Atlas of Cosmetic Oculofacial Surgery, 2nd edn. Elsevier, 2009.
Fagien S. Putterman’s Cosmetic Oculoplastic Surgery, 4th edn. Philadelphia: Saunders; 2007.
Rootman J. Diseases of the Orbit, 2nd edn. Philadelphia: Lippincott Williams and Wilkins; 2002.
Smith BC, Nesi FA, Cantarella VH, et al. Smith’s Ophthalmic Plastic and Reconstructive Surgery, 2nd edn. St Louis: Mosby; 1998.

 of retina
of retina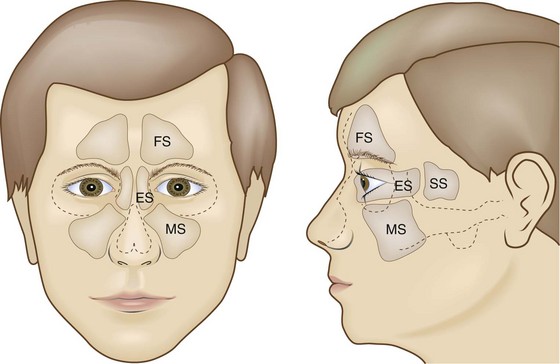
 of upper lid, medial
of upper lid, medial  of lower lid
of lower lid of upper lid, lateral
of upper lid, lateral  of lower lid
of lower lid























 of patients have normal serum lipids
of patients have normal serum lipids