CHAPTER 42 Midcarpal Instability
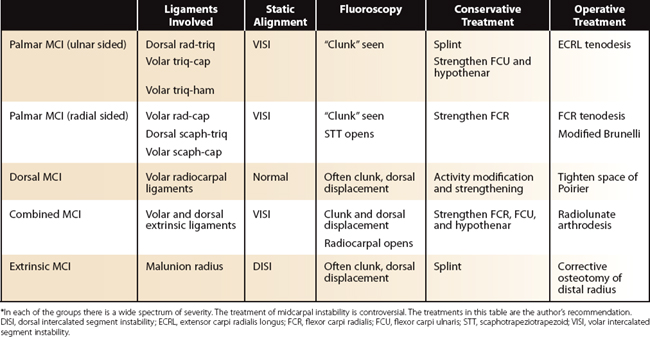
The first description of a “snapping wrist,” diagnosed as anterior midcarpal subluxation,1 was recorded in 1934, although “dorsal luxation of the capitate” had been presented in a congress in Paris in 1919. The article by Lichtman and colleagues2 in 1981 brought this particular condition to the attention of orthopaedists. Of all the forms of carpal instability, midcarpal instability (MCI) has been the most confusing. The two main reasons for this are that MCI is a mixed bag of conditions, and that their pathophysiology is not well understood. The management of MCI remains controversial. Table 42-1 provides a summary of MCI.
The term MCI covers a range of conditions characterized by a painful clunk, usually felt in ulnar deviation of the wrist. It has been suggested that the term “instability of the proximal carpal row” would be a more accurate description3 because the mechanical problem is a carpal instability nondissociative, affecting the radiocarpal or the midcarpal joints or both. The scaphoid, lunate, and triquetrum move like one unit, but not in a predictable, smooth manner.
What Causes the Clunk?
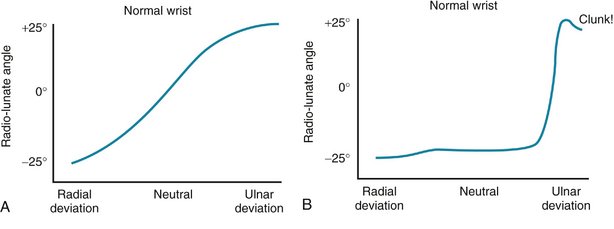
Clunking of the wrist can be caused by congenital laxity of the wrist ligaments, bone or joint dysplasia, lunotriquetral injury, distal radius malunion, or insufficiency of the extrinsic ligament affecting the radiocarpal or the midcarpal joint or both. In a normal wrist, during radial deviation, the proximal carpal row goes into flexion, and during ulnar deviation it extends, in a smooth transition (Fig. 42-1A). In a wrist with palmar MCI, there is palmar subluxation of the capitate head with the wrist in radial deviation in the midcarpal joint, and the proximal carpal row remains flexed until terminal ulnar deviation, at which time it is suddenly forced into extension. This sudden extension causes the so-called catch-up clunk felt by the patient and often clearly seen and heard by observers (Fig. 42-1B).
Classification of Midcarpal Instability
Lichtman and Wroten4 proposed a classification of MCI that includes intrinsic MCI, which is caused by ligamentous insufficiency, and extrinsic MCI, secondary to distal radius fractures. Intrinsic MCI is subdivided further into palmar, dorsal, and combined, depending on the direction of displacement. This classification is helpful in understanding the spectrum of conditions that constitute MCI, and in defining the boundaries between them.
Caputo and coworkers5 believe that only conditions with a static or dynamic volar intercalated segment instability (VISI) of the proximal carpal row constitute MCI. Their definition of MCI is more restrictive than generally accepted. These authors have classified MCI depending on whether the cause of the instability lies on the ulnar side or on the radial side of the wrist. Ulnar-sided MCI corresponds to palmar MCI without significant symptoms (type I) or with significant symptoms (type II). Radial-sided MCI manifests with a rotary subluxation of the scaphoid, with either an intact scapholunate ligament (type III) or a scapholunate ligament disruption (type IV).
Palmar Midcarpal Instability
Patients with palmar MCI present with a painful clunk of the wrist, often with a history of trivial injury or no trauma at all. Sometimes they can demonstrate the clunk voluntarily “to the amusement of friends, and consternation of doctors.”6 In the author’s experience, this is the most common form of MCI.
Pathomechanics of Palmar Midcarpal Instability
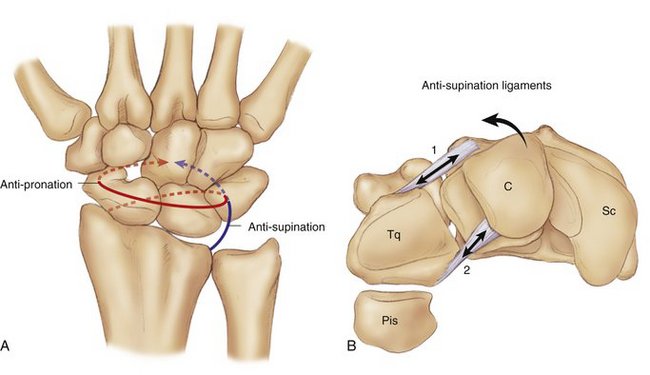
Palmar MCI is considered to be caused by insufficiency of some of the extrinsic wrist ligaments. Ligaments do not work in isolation, but in a synergistic manner, where groups of ligaments resist certain forces. The extrinsic ligaments in the wrist form an antisupination sling and an antipronation sling, both running around the carpus in opposite directions (Fig. 42-2A).
On the ulnar side of the wrist, the dorsal radiotriquetral, which is also known as the dorsal radiocarpal ligament, and the volar triquetrohamate capitate ligaments prevent the proximal carpal row from falling into a VISI alignment. The ligaments act as a sling from the dorsum of the radius, around the triquetrum, and onto the volar aspect of the capitate. This has an antisupination action on the wrist (Fig. 42-2B). If these ligaments fail, the carpus has a tendency to fall into a VISI alignment and into intercarpal supination. The proximal row loses its normal transition from flexion to extension during ulnar deviation of the wrist, causing a clunk.
The distal scaphoid has ligaments to the capitate and to the trapezium. If these ligaments fail, there is a tendency for the scaphoid to flex and to take with it the lunate and the triquetrum, causing a VISI alignment. There is a ligamentous sling, which starts with the volar radiocapitate ligament, follows around the triquetrum, connects to the dorsal scaphotriquetral ligament, and goes around the scaphoid ending with the volar scaphocapitate ligament (Fig. 42-2C). This sling goes round the wrist causing an antipronation effect. Failure of this mechanism may cause flexion of the proximal row, starting on the radial side, and a tendency toward intercarpal pronation. This would cause radial-sided palmar midcarpal instability.
Several studies have attempted to reproduce carpal instability in cadaver models. Biomechanical studies2 reported that sectioning the dorsal radiotriquetral and the triquetrohamate portion of the triquetrohamate capitate ligament did not produce frank instability or a clunk. Further division of the triquetrocapitate portion of the triquetrohamate capitate ligament produced a clunk similar, but not identical, to clunks observed in patients. Other studies have shown that sectioning either the ulnar arm of the distal volar “V” ligaments or the dorsal radiotriquetral ligament can produce a VISI and mechanical changes typical of palmar MCI.7,8
Assessment of Palmar Midcarpal Instability
The symptoms of a patient presenting with a clunking wrist range from none at all to severe. Looking at the wrist from the ulnar side, a palmar sag can be seen, which reduces with ulnar deviation of the wrist (Fig. 42-3). The midcarpal shift test, described by Lichtman,2 reproduces the patient’s wrist instability. This test is done by placing the patient’s wrist in neutral with the forearm pronated. A palmar force is applied to the hand at the level of the distal capitate. The wrist is simultaneously loaded axially and deviated ulnarly. The test is positive if a painful clunk occurs that reproduces the patient’s symptoms.
Plain radiographs generally show a VISI pattern, but no dissociation between the bones of the proximal carpal row (Fig. 42-4). If there is a dissociation between lunate and triquetrum, this is a type of carpal instability dissociative and not MCI (Fig. 42-5).
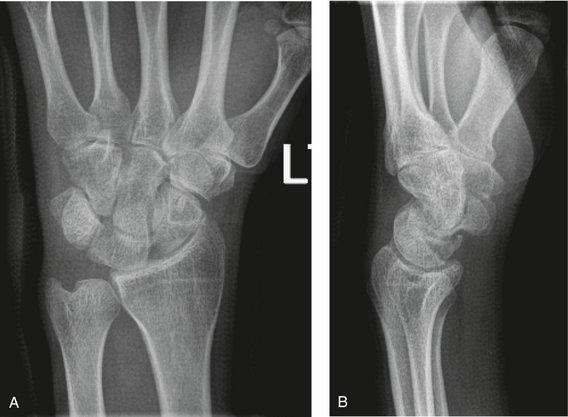
FIGURE 42-4 A and B, Plain radiographs show a volar intercalated segment instability alignment of the carpus. There is no dissociation. This is typical of palmar or combined midcarpal instability.
On a mini-C-arm, a lateral view of radioulnar deviation of the wrist shows the typical jump of the proximal row from flexion to extension. The examiner should perform a “passive palmar displacement” and a “passive dorsal displacement” of the wrist, and observe if there is displacement and opening at either joint. This maneuver establishes if the laxity is at the midcarpal joint or radiocarpal or both. On the posteroanterior view, radioulnar deviation needs to be observed, to rule out any scapholunate or lunotriquetral dissociation, and to look for any opening of the scaphotrapeziotrapezoid (STT) joint, which would indicate laxity of the ligaments on the radial side of the wrist.
Treatment of Palmar Midcarpal Instability
For palmar MCI, published studies support the use of limited carpal arthrodesis over soft tissue stabilizations.9,10 Triquetrohamate,11 four-corner arthrodesis,12 and STT5 fusions have been proposed. The downside of these procedures is that they block the midcarpal joint, preventing the useful movement in the “dart throwing” arc, from dorsoradial to palmar-ulnar.
If a particular ligament is found to be the cause of the instability, augmentation seems to be the most sensible option. In palmar MCI in which the pathology is ulnar-sided, the author’s limited experience with the procedure proposed by Garcia-Elias and Geissler13 has produced excellent results. This technique uses half the extensor carpi radialis brevis tendon to recreate the ulnar limb of the arcuate ligament and the dorsal radiotriquetral ligament.
If the cause of palmar MCI is on the radial side, conservative treatment including exercises to strengthen the flexor carpi radialis should be tried. Failing that, a modified Brunelli reconstruction using half of the flexor carpi radialis tendon would recreate the ligaments across the STT joint and the dorsal scapholunate ligament, providing a good alternative to an arthrodesis.13
Dorsal Midcarpal Instability
There are two subgroups in this type of MCI. The first subgroup manifests typically without a history of trauma, with pain and clicking of the wrist, precipitated by tight grasping, particularly with the forearm in supination; this has been named the capitolunate instability pattern.14 In a reported series of 11 patients, plain radiographs seemed normal, but doing a dynamic dorsal displacement under fluoroscopy revealed the diagnosis in all patients. To perform the test, the examiner applies dorsally directed force to the scaphoid tuberosity, with longitudinal traction and flexion of the wrist. X-rays show a dorsal subluxation of the proximal row with characteristic dorsal subluxation of the capitate from the lunate. This test reproduces the patient’s symptoms. Ten of 11 patients became asymptomatic with conservative treatment. This condition was attributed to laxity of the radiolunate ligaments and extrinsic ligaments of the scaphoid.
The second group of patients with dorsal MCI, called chronic capitolunate instability, present with post-traumatic chronic wrist pain, weakness, and wrist clicking, and a history of an extension wrist injury. In the report of a series of 12 patients, radiographs were normal except in 1 patient with a dorsal intercalated segment instability pattern.15 Under fluoroscopy, dorsal subluxation of the capitate on the lunate could be shown by pushing the capitate dorsally. This caused apprehension, and the patients recognized the click caused by the sudden movement of the lunate dorsal and ulnar. Of the 12 patients, 11 underwent surgery to suture the volar radiocapitate ligament to the radiotriquetral ligament, in an attempt to close the space of Poirier. Surgery was generally successful at stabilizing the wrist, although some extension was lost. This condition has been attributed to traumatic attenuation of the palmar radiocapitate ligament. Dorsal MCI seems to be related to insufficiency of the ligaments in the antipronation sling.
Treatment of Dorsal Midcarpal Instability
In the rare cases when surgery is required, the author recommends the method described by Johnson and Carrera.15 Through a volar approach, the space of Poirier is obliterated using a strong nonabsorbable suture, accepting certain loss of extension of the wrist.
Combined or Palmar-Dorsal Midcarpal Instability
Some patients present with a combination of palmar MCI and a positive passive dorsal displacement test, usually in a wrist with marked laxity. In a series of 14 such patients presenting with wrist pain and weakness, half of them had a history of trauma.16 Radiographs showed a VISI deformity. Doing a dorsal displacement test showed subluxation of the capitolunate joint and in some cases subluxation of the radiolunate also. These patients did not improve with nonoperative treatment, and they underwent surgery to obliterate the space of Poirier. This was done by sutureing the radiocapitate ligament to the long radiolunate on the radial side, and the capitotriquetral to the lunotriquetral on the ulnar side. The authors reported excellent outcome in eight cases, good in five, and fair in one.
Treatment of Combined Midcarpal Instability
Patients with combined dorsal and palmar MCI usually have marked laxity of the wrists, and they should be treated nonoperatively as far as possible. The reported result of surgery in multidirectional instabilities is unsatisfactory.3 This coincides with the author’s experience that patients with very lax wrists do not do well with soft tissue surgery.
If all conservative measures fail, and the patient is very symptomatic, the best option is a radiolunate arthrodesis as originally proposed by Halikis and colleagues.17 This procedure orientates the lunate appropriately and abolishes the “proximal row instability,” providing an excellent range of movement in these patients.
Extrinsic Midcarpal Instability
Carpal malalignment secondary to malunion of distal radial fractures was recognized in the 1970s.6 In 1984, Taleisnik and Watson18 reported 13 patients with symptoms of instability and wrist pain, 6 of them with recurrent voluntary midcarpal subluxation. Nine patients were treated by corrective osteotomy of the radius, which resulted in symptom relief and stabilization of the wrists. The one patient whose wrist was stabilized by ligament reconstruction presented with a recurrence of the voluntary midcarpal subluxation.
Caputo and coworkers5 no longer consider this condition to be MCI. They prefer the term “dorsal radius angulation carpal overload,” considering that the cause of the instability is the repetitive overload of the midcarpal joint as a result of the reversal of the normal palmar tilt of the distal radius. This cause is supported by the fact that the instability often manifests months after the injury. The ligaments in the wrist are developed to resist volar and ulnar directed forces, but are inadequate to resist dorsal or radial directed forces such as the ones present after a distal radius malunion.
An alternative explanation for this instability is insufficiency of the volar extrinsic wrist ligaments resulting from the reversal of the volar tilt of the radius.4 The secondary malalignment of the carpus shortens the distance these ligaments span, causing relative laxity and creating a situation similar to dorsal MCI. The instability immediately disappears when the carpal bones realign after a corrective osteotomy. Perhaps another contributing factor is that the mechanism of injury in a distal radius fracture is the same one that can cause an injury of the volar extrinsic wrist ligaments.
There also is a relationship between STT osteoarthritis and dorsal MCI.19 It seems that shortening of the scaphoid can cause extension of the proximal carpal row into a dorsal intercalated segment instability, which can be made worse with certain treatments, such as excision of the distal pole of the scaphoid (Fig. 42-6).
1 Mouchet A, Belot J. Poignet a’ressaut: subluxation medio-carpienne en avant. Bulletin et Memories de la Societe Nationale de Chirurgie. 1934;60:1243-1244.
2 Lichtman DM, Schneider JR, Swafford AR, et al. Ulnar midcarpal instability—clinical and laboratory analysis. J Hand Surg [Am]. 1981;6:515-523.
3 Wright TW, Dobyns RL, Linscheid RL, et al. Carpal instability non-dissociative. J Hand Surg [Br]. 1994;19:763-773.
4 Lichtman DM, Wroten ES. Understanding midcarpal instability. J Hand Surg [Am]. 2006;31:491-498.
5 Caputo AE, Watson HK, Weinzweig J. Midcarpal instability. In: Watson HK, Weinzweig J, editors. The Wrist. Philadelphia: Lippincott Williams & Wilkins, 2001.
6 Linscheid RL, Dobyns JH, Beaubout JW, et al. Traumatic instability of the wrist: diagnosis, classification, and pathomechanics. J Bone Joint Surg Am. 1972;54:1612-1632.
7 Trumble T, Bour CJ, Smith RJ, et al. Kinematics of the ulnar carpus related to the volar intercalated segment instability pattern. J Hand Surg [Am]. 1990;15:384-392.
8 Viegas SF, Patterson RM, Peterson PD, et al. Ulnar-sided perilunate instability: an anatomic and biomechanic study. J Hand Surg [Am]. 1990;15:268-277.
9 Lichtman DM, Bruckner JD, Culp RW, et al. Palmar midcarpal instability: results of surgical reconstruction. J Hand Surg [Am]. 1993;18:307-315.
10 Trumble T, Bour CJ, Smith RJ, et al. Intercarpal arthrodesis for static and dynamic volar intercalated segment instability pattern. J Hand Surg [Am]. 1988;13:384-390.
11 Rao SB, Culver JE. Triquetrohamate arthrodesis for midcarpal instability. J Hand Surg [Am]. 1995;20:583-589.
12 Goldfarb CA, Stern PJ, Kefhaber TR. Palmar midcarpal instability: the results of treatment with 4-corner arthrodesis. J Hand Surg [Am]. 2004;29:258-263.
13 Garcia-Elias M, Geissler WB. Carpal instability. In: Green DP, Hotchkiss RN, Pederson WC, et al, editors. Green’s Operative Hand Surgery. 5th ed. Churchill Livingstone; 2005:535-604.
14 Louis DS, Hankin FM, Greene TL, et al. Central carpal instability–capitate lunate instability pattern: diagnosis by dynamic displacement. Orthopaedics. 1984;7:1693-1696.
15 Johnson RP, Carrera GF. Chronic capitolunate instability. J Bone Joint Surg Am. 1986;68:1164-1176.
16 Aspergis EP. The unstable capitolunate and radiolunate joints as a source of wrist pain in young women. J Hand Surg [Br]. 1996;21:501-506.
17 Halikis MN, Colello-Abraham K, Taleisnik J. Radiolunate fusion: the forgotten partial arthrodesis. Clin Orthop Relat Res. 1997;341:30-35.
18 Taleisnik J, Watson HK. Midcarpal instability caused by malunited fractures of the distal radius. J Hand Surg [Am]. 1984;9:350-357.
19 Tay SC, Moran SL, Shin AY, et al. The clinical implications of scaphotrapezium-trapezoidal arthritis with associated carpal instability. J Hand Surg [Am]. 2007;32:47-54.