CHAPTER 38 Management of Loose Bodies and Other Limited Procedures
INTRODUCTION
The arthroscope has proven itself to be ideally suited for the removal of elbow loose bodies and is the most common indication for elbow arthroscopy.4,16,26 Other limited procedures such as débridement and synovectomy are also very amenable to arthroscopic management. Elbow arthroscopy has, in fact, proven itself valuable in the treatment of many elbow conditions.1,3,4,8,12,14–16,28,31,34 The potential advantages of elbow arthroscopy in the identification and removal of loose bodies include reduced iatrogenic insult using limited portal site incisions, a more thorough and complete assessment of the anterior and posterior compartments of the elbow, and possibly reduced propensity for scarring postoperatively as a result of limited disruption of the elbow capsule. Disadvantages of elbow arthroscopy center squarely on the technical requirements to safely and effectively perform the procedure due to the close proximity of neurovascular structures. A thorough knowledge of the anatomy of the elbow, particularly from the arthroscopist’s perspective, is critical in reducing the chances of neurovascular injury.33 Preinsufflation of the joint with fluid and maintaining the elbow at approximately 90 degrees of flexion during the procedure increase the distance of the neurovascular structures from the articular surfaces and arthroscopic instruments, decreasing the chance of morbidity from portal placement.17 Also, drawing the anatomic landmarks, including marking the location of the ulnar nerve at the initiation of the procedure, probably serves to reduce the risk of injury to these structures as well.32
LOOSE BODIES
Patients with loose bodies usually present with complaints of elbow pain and stiffness and often report catching, snapping, popping, or locking of the joint (Fig. 38-1) (see Chapter 84). Loose bodies do not cause elbow contracture, but they are often present in patients with elbow contracture. These patients with elbow contractures develop loose bodies as a result of the underlying pathologic condition such as osteochondritis dissecans, posterior impingement, or degenerative arthritis with posterior osteophytes on the olecranon and in the olecranon fossa. On physical examination, patients with loose bodies generally have maintenance of elbow motion but may have mild degrees of flexion and/or extension loss. Also, a mild effusion best identified in the posterolateral gutter of the elbow may be present.
Although anteroposterior (AP) and lateral radiographs of the elbow often demonstrate loose bodies (Fig. 38-2), as many as 30% of loose bodies are not detected on plain x-ray studies.26,29,41 Most often, when loose bodies are suspected but not identified on plain radiographs, they will be found in the posterior compartment of the elbow25 (Fig. 38-3). In addition, loose bodies will often migrate within the elbow and even between compartments, making reliable identification more difficult.
Computed tomographic arthrography and magnetic resonance imaging may be helpful in diagnosing loose bodies.41 However, even if objective testing fails to demonstrate loose bodies in patients with classic loose body symptoms, elbow arthroscopy may still be indicated because it represents the best diagnostic modality.
SURGICAL TECHNIQUE
Originally, elbow arthroscopy was performed with the patient in the supine position and the hand suspended in traction. Poehling et al33 used the prone position for elbow arthroscopy, allowing improved access to the posterior aspect of the elbow and facilitating the conversion to open procedures when necessary. O’Driscoll and Morrey27 have popularized the lateral decubitus position. In this position, the arm is placed across the chest. All of these positions are acceptable for removal of loose bodies, but the posterior compartment, where loose bodies are more often found, may be more difficult to access with the patient in the supine position. Regardless of patient position, a thorough assessment of both the anterior and posterior elbow compartments is required. In many patients, more loose bodies are identified at arthroscopy than can be seen on preoperative radiographs.27
Once the patient has been properly positioned, careful palpation of the anatomic structures, particularly the ulnar nerve, is imperative. A dislocated or subluxatable ulnar nerve is present in 16% of the population,5 and care should be taken to ensure that the nerve can be identified in its normal anatomic location. Next, 20 to 30 mL of sterile saline is injected into the joint using the straight posterior or soft spot portal location. Insufflation should continue until some resistance to further fluid injection is felt. Complete filling of the joint with fluid ensures a tight elbow capsule, making joint penetration with the arthroscopic trocar and cannula safer and more reliable.
A proximal anteromedial portal is established initially, and thorough arthroscopic assessment of the anterior elbow joint is carried out. Next, a proximal anterolateral portal may be established. On identification of loose bodies, they can be removed using a variety of arthroscopic graspers (Fig. 38-4). Loose bodies can be surprisingly large and may require a bigger grasper. In fact, these loose bodies will often be larger than the plastic cannula used in the procedure. Options for removal of large loose bodies include either breaking the loose body into more easily removable fragments or grasping the loose body with a large grasper and backing the cannula out of the elbow while keeping this loose body in contact with the tip of the cannula. Additionally, the arthroscopic camera can be used to help push the grasped loose body out of the opposite side of the elbow. Other tips for removal of loose bodies include “pinning” the loose fragment with a spinal needle to provide resistance for grasping the loose body.
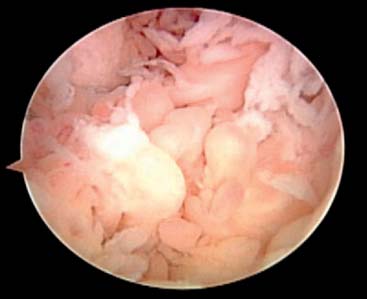
Débridement of osteophytes or loose articular fragments, and arthroscopic management of other anterior compartment pathologic conditions may be necessary at the time of loose body removal. Also, inflammatory tissue and reactive synovitis may be present, and synovectomy should be carefully performed as well11,13,20 (Fig. 38-5). However, use of motorized shavers around the anterior capsule can lead to perforation of the capsule and put the neurovascular structures at increased risk for injury. A thorough synovectomy is important, however, to maximize the outcome of arthroscopic treatment and to help identify loose bodies that can sometimes be obscured by the presence of this synovial tissue. The supplemental use of arthroscopic retractors is valuable and effective in improving visualization during procedures such as synovectomy and in providing additional protection of the capsule and the adjacent neurovascular structures. These retractors can be placed either on the same side as the working portal or opposite that portal depending on the areas to be accessed. In fact, retractors are important to use for a variety of arthroscopic procedures (Fig. 38-6). Blunt-tipped switching sticks and smooth freer elevators can also be used effectively as soft tissue retractors.

FIGURE 38-6 Arthroscopic retractors can improve visualization and protect the capsule and other structures.
Following loose body removal and débridement of the anterior compartment, attention is turned to the posterior compartment. Loose bodies or attached fragments of bone are often present in the olecranon fossa. Leaving the inflow anteriorly may help to “flush out” posteromedial gutter or posterolateral gutter loose bodies as well. In addition, “milking” the gutters, which is accomplished by manually pressing against the posterolateral and posteromedial capsule, may allow for the identification of additional loose bodies located here. Thorough arthroscopic visualization and assessment of both the posteromedial and posterolateral gutters helps to ensure that all loose bodies posteriorly are identified. Limited arthroscopic débridement of soft tissue, particularly in the posterolateral gutter, is often required to view all of the articulating surfaces and to identify loose bodies in this area. Finally, as is the case for the anterior compartment, débridement and removal of reactive tissue and prominent osteophytes posteriorly is important as well.
OUTCOMES
Multiple studies have demonstrated the effectiveness of elbow arthroscopy in the diagnosis and treatment of loose bodies, with success rates of 90% reported.4,16,23 In a review by O’Driscoll and colleagues,26 70% of 71 consecutive elbow arthroscopies were therapeutically beneficial, with loose body removal being the most successful procedure. In fact, all patients with isolated loose bodies benefited from the intervention. However, it is also important to recognize that loose body removal without supplemental arthroscopic management of osteoarthritis has not been found to help patients significantly.23,26,29
SYMPTOMATIC PLICAE
The initial description of elbow snapping caused by a synovial plica was by Clarke in 1988.6 Since that time, the presence of a synovial band or plica adjacent to the radiocapitellar joint has become accepted as a pathologic entity. Little, however, has been published regarding this entity. Antuna and O’Driscoll presented a case series of snapping plicae that represented 8.7% of their arthroscopic elbow procedures performed during a given period.2 Moore, Nirschl, and Stack have all described a synovial fringe excision as part of the operative treatment of lateral epicondylitis.18,22,37 Clarke suggests that a symptomatic synovial plica should be included in the differential diagnosis of tennis elbow or lateral elbow pain.6
Patients with soft tissue impingement due to plicae present with a variety of symptoms. The most dramatic involve a painful locking or catching of the elbow that can be resolved with gentle manipulation. These symptoms can be easily confused with a loose body except that the pain is reproducible over the radiocapitellar joint. More subtle presentations are often difficult to distinguish from lateral epicondylitis.
On physical examination, a band is sometimes palpable over the lateral aspect of the radiocapitellar joint. This point is slightly more distal than the typical lateral epicondylitis pain. A “flexion-pronation test,” described by Antuna and O’Driscoll,2 can reproduce symptoms and often even reproduces snapping. In this test, the forearm is maximally pronated and passively flexed to 90 to 110 degrees. The snapping can be felt during flexion through this limited arc of motion. Another cause of lateral elbow pain that can simulate a snapping plica is posterolateral rotatory instability, but this pathologic condition is usually characterized by pain with supination while under a valgus load at a flexion angle of about 40 degrees.24
SURGICAL INDICATIONS
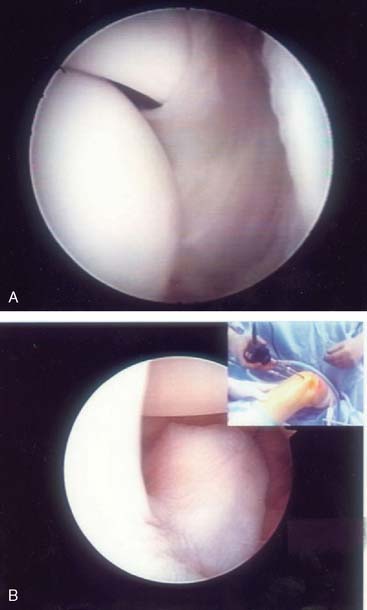
Patients suspected to have a snapping plica unresponsive to nonoperative measures such as activity limitations, nonsteroidal medications, and local injection of corticosteroids can often be treated successfully with arthroscopic débridement and excision of this plica. A systematic assessment of the entire elbow joint is important to avoid overlooking associated lesions or loose bodies. The plica is identified either anteriorly while visualizing through an anteromedial portal or posteriorly by viewing through a posterolateral portal (Fig. 38-7A and B). This lesion can vary from a thin synovial fold to a meniscoid-type band of tissue impinging on the radial head articulating surface.
ARTHROSCOPIC ASSESSMENT OF ELBOW INSTABILITY
Bennett and Waris were two of the first investigators to identify problems in the dominant elbows of overhead athletes.35,42 Since these early reports, understanding of medial and lateral elbow instability has advanced significantly. A thorough understanding of the relevant ligamentous anatomy about the elbow is important in assessing and treating patients with instability.
The diagnosis of the presence and degree of elbow instability can be difficult even for experienced clinicians. A thorough history and careful physical examination can improve the chances of making an accurate diagnosis, but symptoms and signs are often subtle. Arthroscopic evaluation of the elbow for the presence of either valgus instability due to disruption of the medial ulnar collateral ligament or arthroscopic assessment for posterolateral rotatory instability as a consequence of disruption of the lateral ligamentous structures can be helpful in certain clinical situations. Diagnostic elbow arthroscopy performed as an isolated procedure for the purposes of recognizing instability is rarely, if ever, indicated. However, as a surgical adjunct performed in concert with other arthroscopic and/or open surgical procedures, arthroscopic elbow instability assessment can provide valuable information.
MEDIAL INSTABILITY
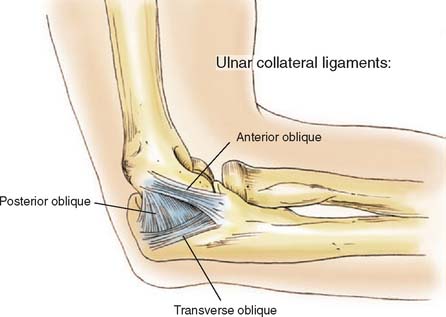
The medial ulnar collateral ligament is composed of an anterior bundle, a fan-shaped posterior bundle, and a transverse ligament that does not contribute to elbow stability35,40 (Fig. 38-8). Disruption of this medial ulnar collateral ligament may be caused by acute or chronic stresses. Overhead throwing regularly subjects the elbow to tremendous valgus forces, and these forces are concentrated on the anterior bundle of the medial ulnar collateral ligament. Undersurface tears of the ulnar medial collateral ligament have been reported, and a sudden valgus stress also can lead to acute rupture of the ligament.38 Such patients often complain of medial-sided elbow pain and sometimes complain of crepit-ation as well. Complaints of instability, however, are unusual.
Even in the presence of a complete disruption of the anterior bundle of the medial ulnar collateral ligament, valgus opening of the elbow occurs only to a very limited extent. This makes definitive diagnosis of medial ulnar collateral ligament instability sometimes difficult. The arthroscope has proven itself a valuable tool in identifying patients with complete disruptions of this ligament. Rarely would arthroscopic evaluation for instability be indicated simply to make a diagnosis of valgus instability, but arthroscopic assessment may greatly influence intraoperative decision making. In a cadaveric study, the medial ulnar collateral ligament was not able to be visualized arthroscopically.10 This makes direct arthroscopic assessment of the anterior bundle’s integrity difficult, if not impossible. Applying a valgus stress to the elbow, however, can provide for effective indirect arthroscopic evidence of medial ulnar collateral ligament insufficiency. This is accomplished through arthroscopic visualization of the most medial aspect of the anterior ulnohumeral articulation from the anterolateral portal with the elbow flexed 60 to 70 degrees. This test, called the arthroscopic valgus instability test, was first described by Timmerman and Andrews.38,39 In a cadaveric study, an evaluation of this arthroscopic valgus instability test demonstrated that opening of the ulnohumeral joint space of as little as 1 mm can represent a complete disruption of the anterior bundle of the medial ulnar collateral ligament.9 In this study, either 1 or 2 mm of ulnohumeral joint opening was seen even after complete transection of the anterior bundle in a cadaveric model while visualizing the ulnohumeral joint arthroscopically. Also, no opening of the medial ulnohumeral joint was seen before complete release of this ligamentous bundle was carried out. This study demonstrates that very little if any ulnohumeral joint opening is demonstrated arthroscopically until complete disruption of the ligament occurs. It also highlights the fact that when the ligament is completely disrupted, a small but reproducibly measurable amount of ulnohumeral joint opening occurs. As a result, the arthroscopic valgus instability test provides a very sensitive measure of the presence and degree of medial joint opening even when clinical examination reveals subtle or no appreciable opening to valgus stress. Finally, it is also important to note that when no ulnohumeral joint opening occurs at the time of arthroscopic assessment, integrity of the medial ulnar collateral ligament is confirmed (Fig. 38-9).
LATERAL INSTABILITY
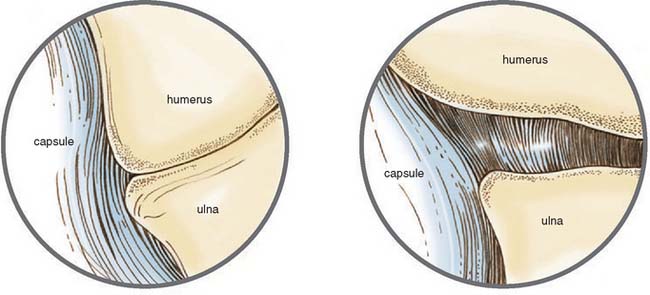
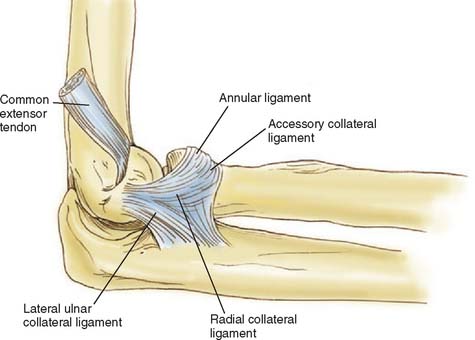
In 1991, O’Driscoll et al introduced the term posterolateral rotatory instability (PLRI) to describe elbow instability caused by injury to the radial ulnohumeral ligament (RUHL) or lateral ulnar collateral ligament. Since this original description, the concept of posterolateral rotatory instability has gained much attention. The original report was that of a group of patients who presented with symptoms of valgus instability after trauma but that did not show typical clinical signs of a deficient medial collateral ligament complex. They found that the radial head rotated and subluxated posteriorly when the elbow was forced into valgus from a supinated and extended position and attributed this instability to the incompetence of the posterolateral structures, specifically the radial ulnohumeral ligament. Although these patients had responded poorly to the standard treatment for valgus instability, they improved significantly after plication or reconstruction of this ligament.24 The lateral or radial ligament complex is made up of 4 components; the RUHL, the radial collateral ligament, the annular ligament, and the accessory lateral collateral ligament19 (Fig. 38-10). O’Driscoll and associates have shown that deficiencies of the RUHL and laxity of the lateral capsule allows the proximal radioulnar joint to rotate and the radial head to sublux posteriorly when stressed, leading to posterolateral rotatory instability.27 In patients with this instability pattern, the radial head subluxes, and on rare occasion, can dislocate posteriorly depending on the position of the elbow. With the forearm supinated and slightly flexed, valgus stress applied to the elbow causes rotation of the ulnohumeral joint, compression of the radiocapitellar joint, and posterior subluxation of the radial head.7,21,24
Symptoms vary from obvious instability complaints to reports of mild pain and discomfort. Occasionally, patients will complain of clicking, popping, snapping, or locking. True dislocations tend to be rare. Rather, patients describe the elbow slipping in and out of joint, particularly when the arm is supinated and slightly flexed.21,24,25,30 Posterolateral rotatory instability may be difficult to diagnose on elbow examination. Differential diagnoses include lateral epicondylitis, radial tunnel syndrome, valgus instability, symptomatic elbow plica, and true radial head dislocation.
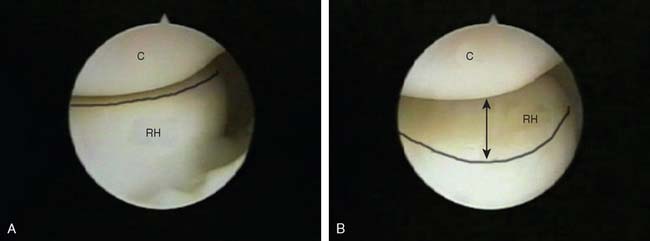
As in the arthroscopic assessment for valgus instability, the arthroscope can also be used to demonstrate posterolateral rotatory instability. In patients in whom PLRI is suspected, the “pivot shift test” described earlier can be performed while arthroscopically viewing the radiocapitellar joint from the anteromedial portal. The radial head will rotate and translate posteriorly if PLRI is present; with a competent ligament, the radial head will rotate but will not translate36 (Fig. 38-11A and B). Also, while viewing from the posterolateral portal, the radial head can be seen to sublux posteriorly when the pivot shift test is applied or often even with maximum forearm supination. Finally, in the presence of significant posterolateral rotatory instability, the arthroscope can often be easily driven through the lateral gutter and into the lateral aspect of the ulnohumeral joint. Arthroscopic visualization of the presence or absence of posterolateral rotatory instability can greatly influence intraoperative decision making as it pertains to the possibility of repair or reconstruction of the lateral collateral ligament complex.
SUMMARY
The most reliably successful elbow arthroscopic procedure in elbow arthroscopy is loose body removal. Thorough and intimate knowledge of elbow anatomy combined with careful surgical technique can be very effective for patients with these symptomatic loose bodies. Arthroscopic management of the underlying cause leading to the production of loose bodies is important as well with arthroscopic débridement and synovectomy often required. Recognition that more loose bodies are usually present than are represented radiographically and careful use of proper arthroscopic technique will help improve outcomes and minimize surgical complications. Symptomatic snapping plicae can also be effectively managed using arthroscopic techniques. Recognition of the lesion and differentiation from other more common causes of lateral elbow pain, including lateral epicondylitis, is important. Finally, when not otherwise obvious, the arthroscope can also be used to identify the presence and degree of elbow instability, including valgus and posterolateral rotatory instability.
1 Andrew J.R., Carson W.G. Arthroscopy of the elbow. Arthroscopy. 1985;1:97.
2 Antuna S.A., O’Driscoll S.W. Snapping plicae associated with radiocapitellar chondromalacia. Arthroscopy. 2001;17:491.
3 Bennett G.E. Shoulder and elbow lesions of the professional baseball pitcher. J. A. M. A. 1941;117:510.
4 Boe S. Arthroscopy of the elbow: diagnosis and extraction of loose bodies. Acta Orthop. Scand. 1986;57:52.
5 Childress H.M. Recurrent ulnar nerve dislocation at the elbow. Clin. Orthop. Relat. Res. 1986;108:168.
6 Clarke R. Symptomatic, lateral synovial fringe (plica) of the elbow joint. Arthroscopy. 1988;4:112.
7 Cohen M.S., Hastings H.II. Rotatory instability of the elbow: The anatomy and role of the lateral stabilizers. J. Bone Joint Surg. Am. 1997;79:225.
8 Commandre F., Taillan B., Benezis C., Follacci F.M., Hammou J.C. Plica synovialis (synovial fringe plica) of the elbow: report of one case. J. Sports Med. Phys. Fit. 1988;28:209.
9 Field L.D., Altchek D.W. Evaluation of the arthroscopic valgus instability test of the elbow. Am. J. Sports Med. 1996;24:177.
10 Field L.D., Callaway G.H., O’Brien J.S., Altchek D.W. Arthroscopic assessment of the medial collateral ligament complex of the elbow. Am. J. Sports Med. 1995;23:396.
11 Horiuchi K., Momohara S., Tomatsu T., Inoue K., Toyama Y. Arthroscopic synovectomy of the elbow in rheumatoid arthritis. J. Bone Joint Surg. 2002;84A:342.
12 Jackson D., Silvino N., Reiman P. Osteochondritis in the female gymnast’s elbow. Arthroscopy. 1989;5:129.
13 Lee P.H., Morrey B.F. Arthroscopic synovectomy of the elbow for rheumatoid arthritis. J. Bone Joint Surg. Br. 1997;79B:770.
14 Lindenfeld T.N. Medial approach in elbow arthroscopy. Am. J. Sports Med. 1990;18:413.
15 Lynch G., Meyers J., Whipple T., Caspari R. Neurovascular anatomy and elbow arthroscopy: inherent risks. Arthroscopy. 1986;2:191.
16 McGinty J. Arthroscopic removal of loose bodies. Orthop. Clin. North. Am. 1982;13:313.
17 Miller C.D., Jobe C.M., Wright M.H. Neuroanatomy in elbow arthroscopy. J. Shoulder Elbow Surg. 1995;4:168.
18 Moore M.Jr. Radiohumeral synovitis: a cause of persistent elbow pain. Surg. Clin. North Am. 1953;33:1363.
19 Morrey B.F. Anatomy of the elbow joint. In: Morrey B.F., editor. The Elbow and Its Disorders. 3rd ed. Philadelphia: WB Saunders; 2000:43.
20 Nemoto K., Arino H., Yoshihara Y., Fujikawa K. Arthroscopic synovectomy for the rheumatoid elbow: a short-term outcome. J. Shoulder Elbow Surg. 2004;13:652.
21 Nestor B.J., O’Driscoll S.W., Morrey B.F. Ligamentous reconstruction for posterolateral rotatory instability of the elbow. J. Bone Joint Surg. Am. 1992;74:1235.
22 Nirschl R.P., Pettrone F.A. Tennis elbow. J. Bone Joint Surg. Am. 1979;61:832.
23 O’Driscoll S.W. Elbow arthroscopy for loose bodies. Orthopaedics. 1992;15:855.
24 O’Driscoll S.W., Bell D.F., Morrey B.F. Posterolateral rotatory instability of the elbow. J. Bone Joint Surg. Am. 1991;73:440.
25 O’Driscoll S.W., Jupiter J.B., King G.J., Hotchkiss R.N., Morrey B.F. The unstable elbow. Instr. Course Lect. 2001;50:89.
26 O’Driscoll S.W., Morrey B.F. Arthroscopy of the elbow: diagnostic and therapeutic benefits and hazards. J. Bone Joint Surg. 1992;74A:84.
27 O’Driscoll S.W., Morrey B.F. Loose bodies of the elbow: diagnostic and therapeutic roles of arthroscopy. J. Bone Joint Surg. 1992;74B(suppl III):290.
28 O’Driscoll W.S., Morrey B.F. Arthroscopy of the elbow. In: Morrey B.F., editor. The Elbow and Its Disorders. 2nd ed. Philadelphia: WB Saunders; 1993:130.
29 Ogilvie-Harris D.J., Schemitsch E. Arthroscopy of the elbow for removal of loose bodies. Arthroscopy. 1993;9:5.
30 Osborne G., Cotterill P. Recurrent dislocation of the elbow. J. Bone Joint Surg. Br. 1966;48:340.
31 Poehling G.G., Ekman E.F. Arthroscopy of the elbow. J. Bone Joint Surg. 1994;76A:1265.
32 Poehling G.G., Ekman E.F. Arthroscopy of the elbow. Instruct. Course Lect. 1994;44:214.
33 Poehling G.G., Ekman F., Ruch D.S. Elbow arthroscopy: introduction and overview. In: McGinty J.B., Caspari R.B., Jackson R.W., Poehling G.G., editors. Operative Arthroscopy. 2nd ed. Philadelphia: Lippincott; 1996:821.
34 Poehling G., Whipple T., Sisco L., Goldman B. Elbow arthroscopy: a new technique. Arthroscopy. 1989;5:222.
35 Schwab G.H., Bennet J.B., Woods G.W., Tullos H.S. Biomechanics of elbow instability: the role of the medial collateral ligament. Clin. Orthop. Relat. Res. 1980;146:42.
36 Smith J.P.III, Savoiem F.H.III, Field L.D. Posterolateral rotatory lateral instability of the elbow. Clin. Orthop. Relat. Res. 2001;20:47.
37 Stack J.K., Hunt W.S. Radio-humeral synovitis. Q. Bull. Northwestern Univ. 1946;20:394.
38 Timmerman L.A., Andrews J.R. Undersurface tear of the ulnar collateral ligament in baseball players. Am. J. Sports Med. 1983;22:33.
39 Timmerman L.A., Andrews J.R. Histology and arthroscopic anatomy of the ulnar collateral ligament of the elbow. Am. J. Sports Med. 1994;22:667.
40 Tullow G.S., Schwab G., Bennett J.B., Woods G.W. Factors influencing elbow instability. Instr. Course Lect. 1981;30:185.
41 Ward W.G., Belhobek G.H., Anderson T.E. Arthroscopic elbow findings: correlation with preoperative radiographic studies. Arthroscopy. 1992;8:498.
42 Waris W. Elbow injuries of javelin throwers. Acta Chir. Scand. 1946;93:563.