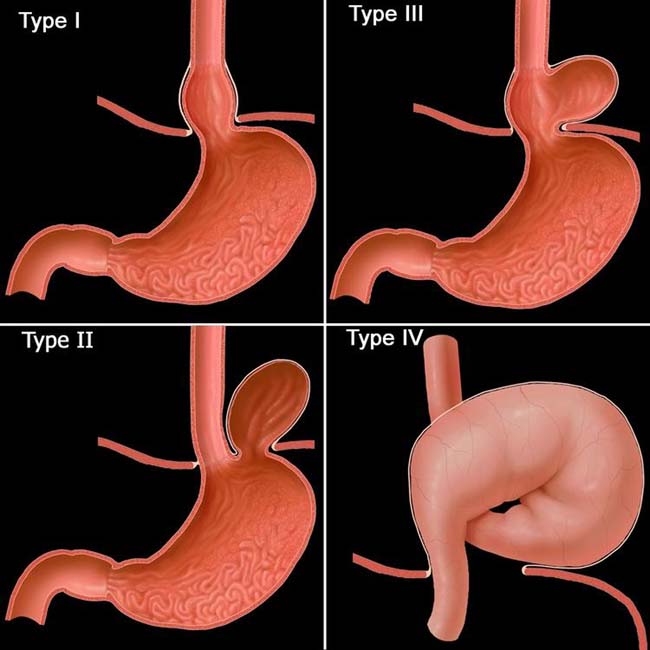
Sliding (axial) hiatal hernia (HH): Gastroesophageal (GE) junction and gastric cardia pass through esophageal hiatus
• Surgical classification
 Type II Paraesophageal (PEH): GE junction in normal position under diaphragm, fundus in chest (very rare)
Type II Paraesophageal (PEH): GE junction in normal position under diaphragm, fundus in chest (very rare)
 Type II Paraesophageal (PEH): GE junction in normal position under diaphragm, fundus in chest (very rare)
Type II Paraesophageal (PEH): GE junction in normal position under diaphragm, fundus in chest (very rare)• Type I (sliding HH): Signs on upper GI series
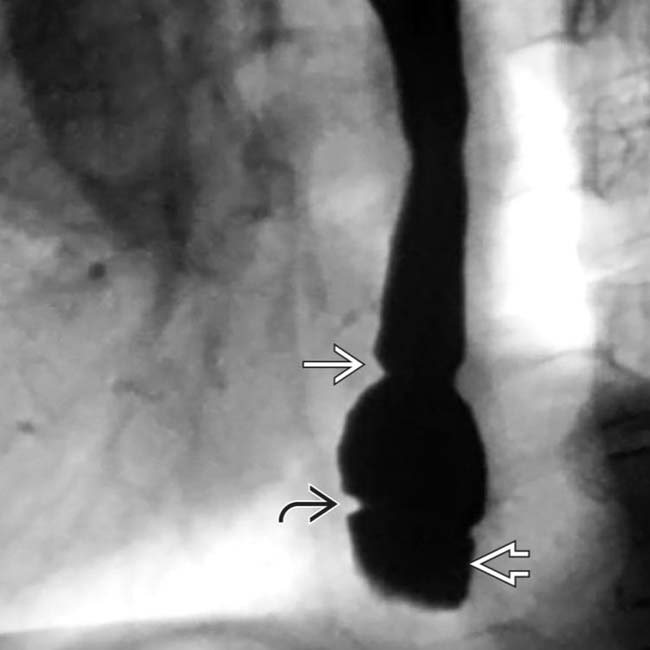
 proximally and the B ring
proximally and the B ring  distally. Just below the B ring is the herniated portion of the gastric cardia
distally. Just below the B ring is the herniated portion of the gastric cardia  .
.
 . Gastric folds
. Gastric folds  extend up through the hiatus.
extend up through the hiatus.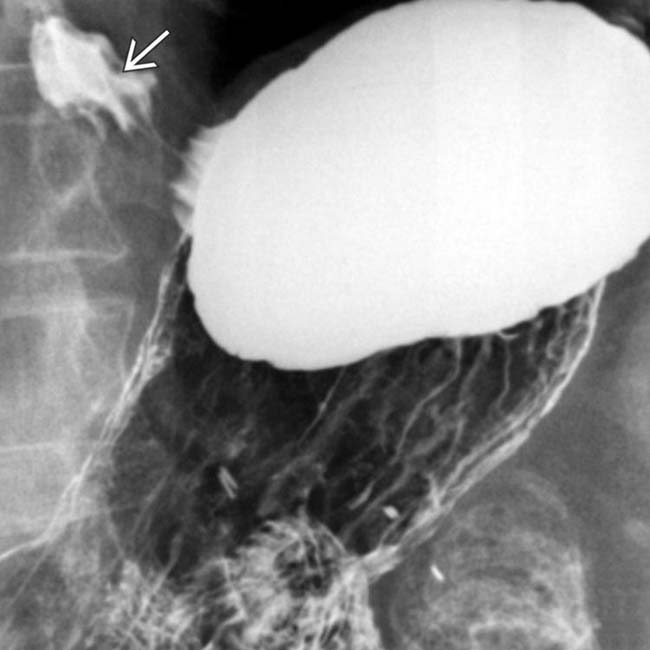
 . While reflux is commonly seen in patients with sliding HHs, it is uncertain whether the HH causes the reflux or vice versa.
. While reflux is commonly seen in patients with sliding HHs, it is uncertain whether the HH causes the reflux or vice versa.IMAGING
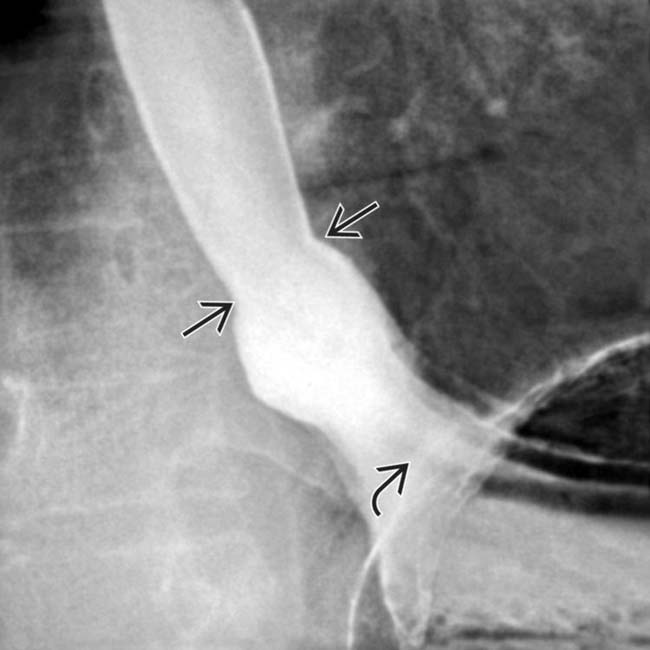
General Features

 in this patient with a type III PEH is in the chest, along with a substantial portion of the stomach. The stomach is pinched as it traverses the diaphragmatic hiatus
in this patient with a type III PEH is in the chest, along with a substantial portion of the stomach. The stomach is pinched as it traverses the diaphragmatic hiatus  . Type III PEHs are encountered with increased frequency.
. Type III PEHs are encountered with increased frequency.

 and what appear to be bowel segments
and what appear to be bowel segments  to the left of the thoracic spine.
to the left of the thoracic spine.
 lies within the right hemithorax and the colon
lies within the right hemithorax and the colon  lies to the left and behind the heart, along with omental fat, all herniating through a wide defect in the esophageal hiatus.
lies to the left and behind the heart, along with omental fat, all herniating through a wide defect in the esophageal hiatus.
 or compression of the colon as it traverses the hiatus.
or compression of the colon as it traverses the hiatus.
 . Note the position of a nasogastric tube
. Note the position of a nasogastric tube  within the herniated stomach and duodenum, which is within the abdomen.
within the herniated stomach and duodenum, which is within the abdomen.




























































 remains below the diaphragm.
remains below the diaphragm.
 in the hernia continuing into the abdomen. The “feline” appearance of the esophageal mucosa is due to reflux.
in the hernia continuing into the abdomen. The “feline” appearance of the esophageal mucosa is due to reflux.


