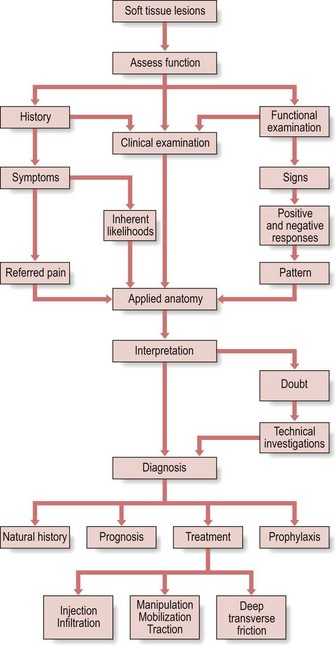
Clinical diagnosis of soft tissue lesions
Introduction
First of all, not every detected anatomical lesion causes pain or dysfunction. Asymptomatic lesions do exist and are present in numbers that are much larger than previously assumed: asymptomatic herniations in cervical, thoracic and lumbar spine are present in up to 50% of the population.1,2,3 Also the high prevalence of rotator cuff tears in elderly asymptomatic individuals is very well known.4,5 It is estimated that in the general population, approximately two-thirds of all rotator cuff tears are asymptomatic.6,7 Large numbers of asymptomatic lesions have also been demonstrated in the knee. A recent MRI study on asymptomatic soccer players demonstrated one or more MRI abnormalities in no less than 64%. Another study with MRI scans performed on the knees of asymptomatic male professional basketball players demonstrated an overall prevalence of articular cartilage lesions of 47.5%8 and meniscal lesions of 20%.9
Principles of diagnostic procedure in orthopaedic medicine
2 Look for objective physical signs
3 Avoid palpation as much as possible
The function of the different tissues is known
• Some regions in the body are always tender to touch (e.g. lesser tuberosity at the shoulder, lateral epicondyle at the elbow, border of the trapezius muscle).
• Some structures lie too deeply and cannot be reached by the palpating finger (e.g. capsule of the hip joint, cruciate ligaments at the knee).
• The painful area does not always correspond to the site of the lesion (referred pain) and referred dural tenderness is sometimes present.
• Some patients with altered perception or desire to deceive the examiner may produce misleading responses.
4 Functional testing: the principle of ‘selective tension’
5 Use physiological movements as much as possible
Normal movements may become disturbed
This approach has some advantages:
• The structures that participate in the movement are well known (applied anatomy).
• The movements are easily controllable and reproducible. Pain may be provoked, but also limitation can be seen and weakness is not difficult to detect. The inter- and intra-tester reliability is quite high.10–15
• Patterns can be found: pain patterns, patterns of limitation and patterns of weakness. The recognition of a known pattern confirms the symptoms and signs presented.16
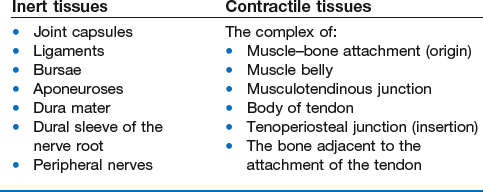
6 Distinguish between inert and contractile tissues
Soft tissues are either inert or contractile
This distinction is one of the pillars on which the whole system of orthopaedic medicine rests. The soft tissues of the locomotor system can be divided on the one hand into tissues that can contract (the contractile structures) and on the other hand, tissues that do not possess this capacity (the non-contractile or inert structures) (Box 4.1).
Contractile structure
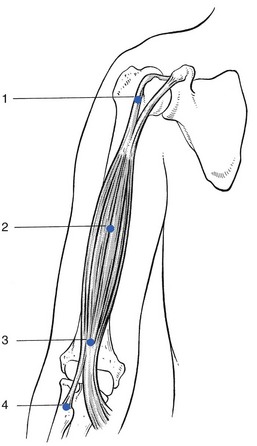
The complex of muscle origin, muscle belly, musculotendinous junction, body of tendon, tenoperiosteal junction and also the bone adjacent to the attachment of the tendon are considered clinically as contractile (Fig. 4.1).
10 Keep the balance between credulity and excessive scepticism
Objectivity is a fair attitude
Orthopaedic medical disorders produce symptoms and signs that may be difficult to analyse objectively. Patients who have a reason to assume disorders for some type of personal gain, therefore, commonly use clinical features in the locomotor system to try to establish their credibility (see online chapter Psychogenic pain).
Clinical evaluation
History
Cyriax said: ‘Every patient contains a truth. He will proffer the data on which diagnosis rests. The doctor must adopt a conscious humility, not towards the patient, but towards the truth concealed within the patient, if his interpretations are regularly to prove correct’.17
Taking the history
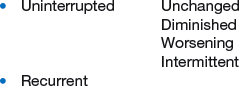
Progression/evolution
The symptoms may be present without interruption from their onset. However, it is also possible that the patient describes a recurrence (see Box 4.2).
A very important distinction should be made between the following definitions.
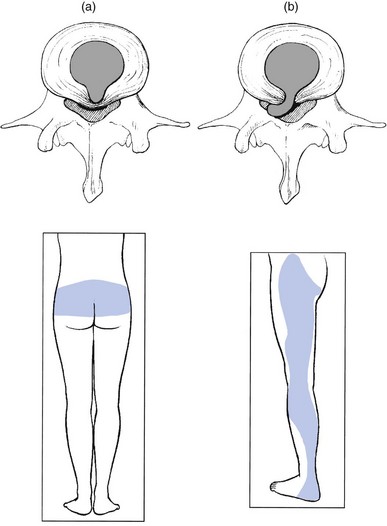
Reference of pain
Referred pain is a very typical feature in non-osseus lesions of the locomotor system. It is mostly segmental and thus experienced in a single dermatome, which indicates the segment in which the lesion should be sought. Reference of pain is influenced by the severity of the lesion: the more severe it becomes, so giving rise to a stronger stimulus, the further distally does the pain (usually) spread. The reverse also holds: reduction in the distal distribution is synonymous with improvement.18,19
Shifting pain
Pain coming on in one place as it leaves another indicates a shifting lesion.
The same happens in soft tissue lesions. A good example is central backache, which becomes unilateral, then later on shifts to the buttock and finally to the lower limb – the backache has become sciatica. This shift can only be explained as follows: a structure lying in the midline and originally compressing the dura mater (backache) has shifted to one side and now compresses the dural sleeve of the nerve root (root pain). To be able to shift, that structure has to lie in a cavity and, because the pain was originally central, this has to be a central cavity. The only structure lying in a central cavity and able to change its position is the intervertebral disc: there is no other possibility (Fig. 4.2).
Actual symptoms
Pain (Box 4.3)
There are many different ways of describing pain: it is amazing how much variation patients can achieve in their vocabulary and how many different descriptive terms can be used for the different sensations perceived. The reason lies in the fact that pain is mainly an unpleasant emotional state that is aroused by unusual patterns of activity in specific nociceptive afferent systems. The evocation of this emotional disturbance is contingent upon projection to the frontal cortex.20,21 The nature of the pain may have some diagnostic value: everybody knows the throbbing pain of migraine, the stabbing pain of lumbago or the burning sensation of neuralgic conditions. Although the way the patient describes the pain may sometimes point to a certain disorder, it can also indicate the emotional involvement of the patient with the lesion.
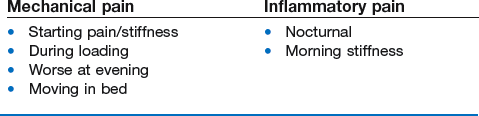
Pain may have either a mechanical or an inflammatory character (Box 4.4). Mechanical pain (e.g. in arthrosis) is characterized by pain and stiffness at the beginning of a movement; augmentation when load is put on the joint; pain at the end of the day and absence of pain at rest, although moving in bed may also be uncomfortable. Inflammatory pain (e.g. rheumatoid arthritis, gout or infectious arthritis) wakes the patient at night and gives rise to frank stiffness early in the day.22
A momentary subluxation of a loose fragment of cartilage in a joint
This happens quite often in the lumbar spine, the knee and the hip and less frequently in the elbow, ankle and subtalar joints. If there are any signs found during clinical examination, they will be articular – a non-capsular pattern (see p. 74). The combination of twinges and articular signs is pathognomonic of the existence of internal derangement.
Paraesthesia
Non-painful sensory disturbances, paraesthesia, are strongly indicative of a condition that originates in a nerve (Box 4.5). They may result from an intrinsic lesion (primary neuritis or secondary polyneuropathy) or from an extrinsic cause (compression). They may also vary in quality and in intensity. In orthopaedic medicine the variation lies between numbness and real pins and needles. It is very often described as ‘tingling’.
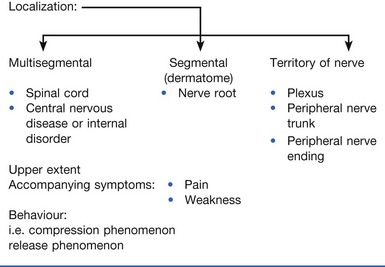
In entrapment neuropathies, knowledge of what brings the pins and needles on will show whether a compression phenomenon or the release phenomenon is acting (see pp. 26–27). For example, pressure on a small distal nerve gives rise to paraesthesia and analgesia in the cutaneous area of that nerve during the time of compression (e.g. meralgia paraesthetica). However, when a nerve trunk or nerve plexus becomes compressed, the paraesthesia are felt in a larger area, corresponding with the territory of that nerve and occur only after the compression has ceased (e.g. thoracic outlet syndrome). Nerve root compression results in segmental pain and paraesthesia felt within the corresponding dermatome (e.g. sciatica). Multisegmental bilateral paraesthesia indicates a lesion in the spinal cord.
Functional disability
When limitation of movement is mentioned, its nature will have to be determined during the functional examination: limitation of active movements only, or limitation of both active and passive movements, and in this case whether it is of the capsular or of the non-capsular type. End-feel at the end of the passive movements and the relationship between pain and end-feel must also be ascertained (see pp. 73–74).
Further questions
Other questions, if appropriate, are asked about similar symptoms, past or present, in other parts of the body, especially other joints (see Box 4.6). If the answer is positive, conditions such as rheumatoid arthritis, spondylitic arthritis, Reiter’s disease and gout should be suspected and further examination is required.
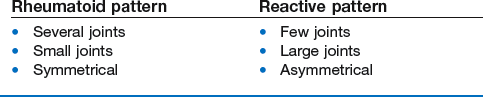
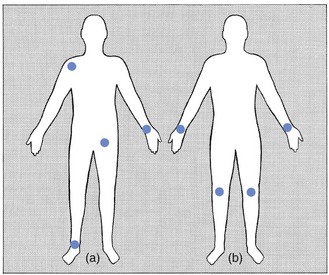
Disorders of rheumatoid type (rheumatoid arthritis, lupus erythematosus, systemic sclerosis, dermatomyositis) are characterized by the symmetrical joint involvement, usually of the small joints (e.g. metacarpophalangeal joints). Arthritis of reactive type (e.g. peripheral joint involvement in ankylosing spondylitis, ulcerative colitis, Reiter’s disease, sarcoidosis or psoriatic arthritis) affects a few large joints (e.g. shoulder, hip or knee) asymmetrically (Fig. 4.3).
Inquiries should also be made about previous treatments, which may give some idea of the chance of success of the proposed therapy. Previous surgery, its timing and indication are noted – it is not impossible that the present condition is the outcome of previous intervention (Box 4.7).
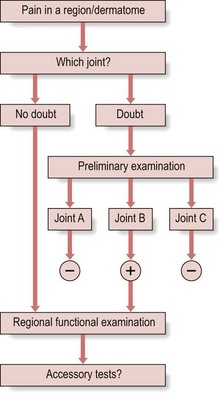
Preliminary examination
This ‘preliminary’ examination (Fig. 4.4) includes tests for the different joints. For example, the preliminary examination for pain down the arm includes tests for the cervical spine, shoulder girdle, shoulder, elbow, wrist and hand (Table 4.1).
Table 4.1
Movements tested in the preliminary examination of the upper limb
| Root | Region | Type |
| C1 | Neck movements | Active |
| Resisted | ||
| C2–C4 | Shoulder movements | Active |
| Resisted | ||
| C5 | Arm movements | |
| Shoulder | Active | |
| Resisted | ||
| C6–C7 | Elbow | Passive |
| Resisted | ||
| Wrist | Resisted | |
| C8 | Thumb | Resisted |
| T1 | Fingers | Resisted |
Functional examination
This does not imply that the diagnosis will always be reached after the standard functional examination. It may sometimes be necessary to add accessory tests (see pp. 66–67).
Movements
Active movements
Active movements are mainly used to determine quickly the area from which symptoms originate and what structures to test in detail with passive and/or resisted movements (Box 4.8).
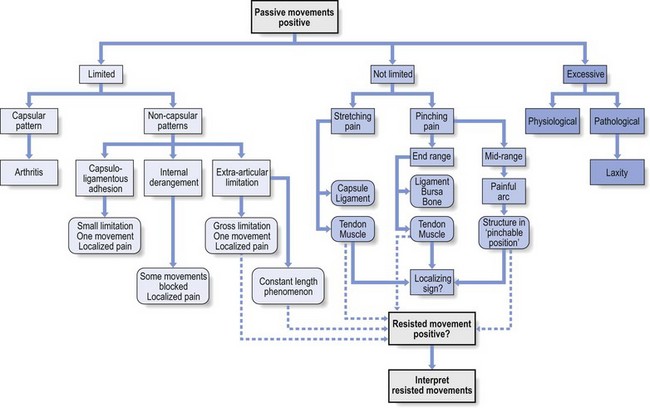
Passive movements (Fig. 4.5)
These tests are meant to examine the inert tissues. The information they give is precise, provided they are performed correctly. The patient should completely relax the muscles and let the examiner do the movement. It is important to realize that non-inert tissues may also be stretched by the manœuvre: if this gives rise to pain, it must be determined whether there is a ‘contractile tissue pattern’, in which case active contraction in the opposite direction will also be painful (see pp. 77).
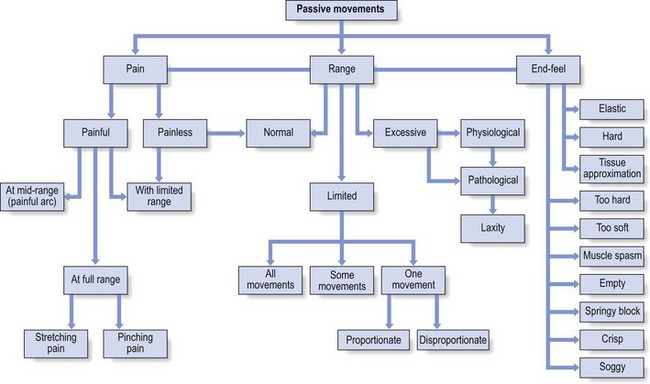
Fig 4.5 Passive movements.
The criteria for passive testing are pain, range and end-feel (Box 4.9).
Amplitude
Limited movement requires the examiner to ascertain whether the limitation is in all directions or only in some directions or in one direction only. If only one movement is reduced, a ‘proportionate’ or a ‘disproportionate’ limitation may be present (see p. 76).
End-feel
End-feel is diagnostically important as it gives an idea of the structure or condition that stops the movement.23 In addition it has therapeutic consequences. Especially during attempted spinal manipulations, the sensation imparted to the operator’s hand will indicate whether or not to proceed. Likewise, in the shoulder or hip, the decision whether to undertake capsular stretching depends on end-feel.
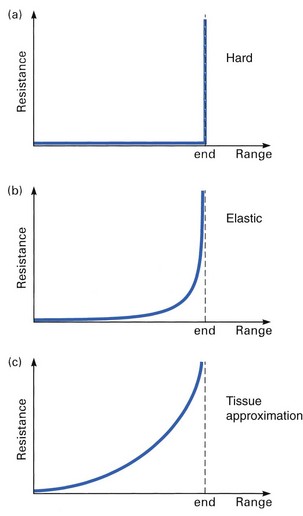
This can be hard, elastic or related to tissue approximation:
• Hard: the movement comes to an abrupt stop, either because two bony surfaces meet (bone-to-bone end-feel) or because a ligamentous structure prevents further movement (Fig. 4.6a). Extension of the elbow has a bone-to-bone end-feel, because the main factor that stops the movement is the engagement of the olecranon process in the olecranon fossa. Extension of the knee also has a hard stop, though less clearly direct than the elbow; here, the main structure that stops movement is the posterior cruciate ligament, which does not stretch.
• Elastic: at the end of range the examiner feels resistance but further stretching over a few degrees is possible (Fig. 4.6b). The feeling is one of two pieces of tough rubber being squeezed together or of a piece of thick leather being stretched. This end-feel is typical of a normal joint capsule and is felt during most rotation movements in shoulder, elbow, hip, knee, cervical and thoracic spine. The tern ‘elastic’ has the same meaning as ‘capsular’.
• Tissue approximation: this end-feel is normal in those movements where extra-articular soft tissues engage against each other (Fig. 4.6c). Flexion at elbow and knee give this ‘soft’, ‘muscular’ end-feel. At the elbow the muscles of the forearm come in contact with the biceps and at the knee the calf muscles engage against the hamstrings. This ‘extra-articular’ end-feel does not occur in patients with poorly developed muscles: they present an ‘articular’ end-feel, either hard or elastic.
A number of types of end-feel are pathological.
• Too hard: the normal elastic, or tissue approximation, end-feel may become harder when the quality of the tissue that stops the movement alters under the influence of pathological conditions. This change very often accompanies limitation of movement because of capsular contracture, osteophytic outcrops of bone, myositis ossificans or a malunited fracture close to the joint. Dependent on the condition, the end-feel may vary from a slight increase in hardness (early arthrosis) to a bony block (ankylosing spondylitis). The latter forms a contraindication to further stretching (i.e. during manipulation).
• Too soft: in those instances where a hard end-feel is expected, the movement may come to a soft stop. This is especially the case in a loose body blocking a movement as may happen at the elbow: extension is limited by a few degrees with a soft end-feel.
• Muscle spasm: this involuntary muscular contraction usually indicates severe disorder. The muscles contract with a sudden, vibrant ‘twang’ even when the movement is performed very gently. This is reflex protective spasm and may happen in acute conditions, such as arthritis in the acute stage. It may also be a sign of more serious lesions such as recent fracture (e.g. scaphoid fracture at the wrist) or secondary deposits (e.g. in a cervical vertebra). Such an end-feel is always an absolute contraindication to manipulation.
• Empty: movement may be so painful that the patient begs the examiner to desist. The latter feels that further movement would be possible because there is no organic resistance but stops the movement because of the perceived pain or out of sympathy for the patient. Further forcing would result in active voluntary muscular contraction. This situation always indicates a serious problem. Acute bursitis, extra-articular abscess or neoplasm is a possibility, but there is nothing wrong with the joint itself. This end-feel may also indicate laxity in a joint or a non-organic lesion. In the latter case there is initial strong resistance, which yields to sustained pressure, disclosing a full range of motion.
• Springy block: this finding always indicates internal derangement: when part of an intra-articular cartilaginous tissue displaces, it may prevent a full range of movement which leads to a rebound at the extreme of the possible range. The commonest examples are a displaced meniscal fragment in the knee and a buckled end-plate in the lumbar spine.
• Crisp: this is typical for a disc protrusion and is best felt in the cervical spine. The feeling is the result of small involuntary muscular contraction at the end of the possible range, known as ‘muscle guarding’. The condition is not acute, as a result of which there is no real muscle spasm.
• Soggy: this end-feel is seldom encountered and can be situated somewhere between a soft and an empty feeling. It is typical of rheumatoid arthritis in the upper cervical joints and is a strong contra-indication to manipulation.
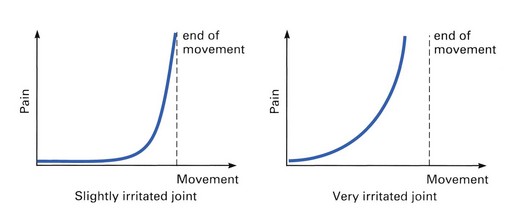
Relationship between pain and end-feel
It is also important to look for the relationship between the moment of appearance of pain and that of the end-feel. Usually the pain comes on at the same time as the end of range is sensed (Fig. 4.7). Earlier pain implies that the joint is in a very irritated state which has therapeutic implications.
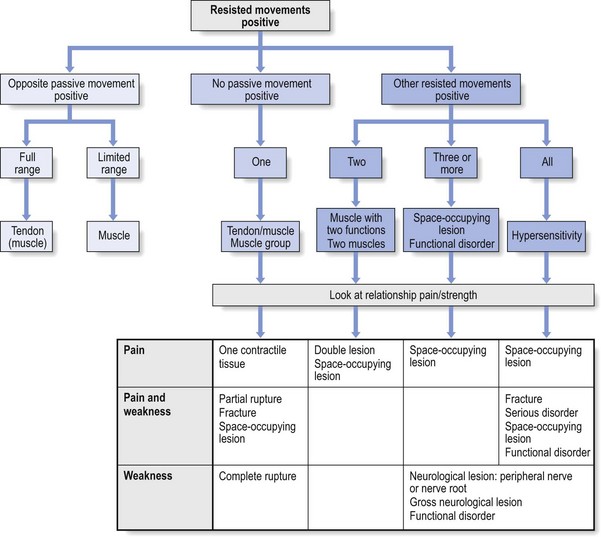
Resisted movements
The position of the examiner must be such that the force exerted by the patient can be resisted. A maximal contraction is asked for and held for a few seconds. Counterpressure is therefore taken by the other hand at the opposite side. For example, to test resisted extension of the neck, one hand is put on the occiput and another hand on the sternum (Fig. 4.8). Similarly, to test resisted flexion, one hand is placed on the forehead and the other between the scapulae.
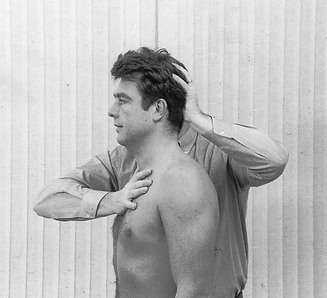
Fig 4.8 Resisted extension of the neck.
The criteria when testing against resistance are pain and strength (Box 4.10).
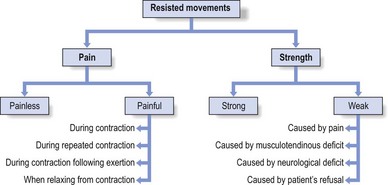
Fig 4.9 Resisted movements.
Accessory tests
An important feature is that a distinction should be made between standard functional examination and accessory tests. The basic examination is always done in its entirety, whereas the accessory tests are applied selectively (Box 4.11).
When unusual signs are found
Discrepancies between individual findings on functional examination may suggest an unusual and possibly serious lesion, a psychogenic problem or an attempt to deceive. In the former, the patient is sent for further specialized examination. When neurosis or deception is suspected, the patient is subjected to a number of accessory tests: additional movements that cannot possibly influence the alleged symptoms or repetition of tests in other positions. The opportunity for the patient to make mistakes is thus presented, which in a positive way can confirm the examiner’s suspicion (see online chapter Psychogenic pain).
Palpation
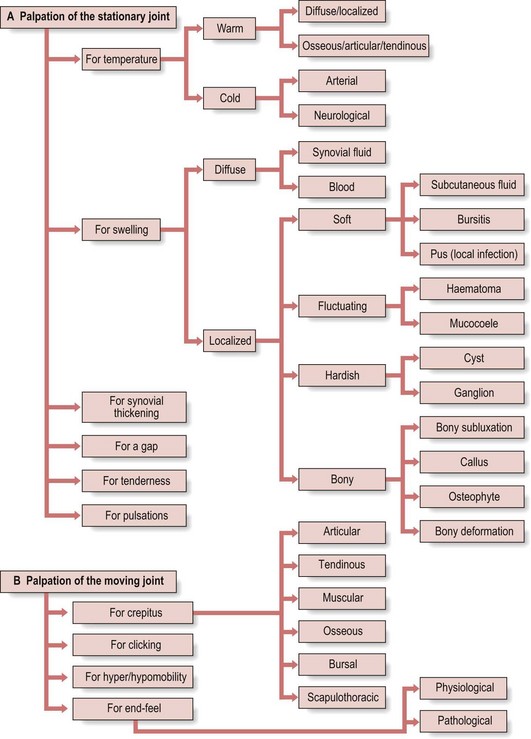
Palpation of the stationary joint
During palpation of a motionless joint (Fig. 4.10a) the examiner may assess temperature (either warmth or cold), swelling, synovial thickening or structural changes. Palpation may also elicit tenderness.
Gaps
A gap may be palpated at the site of the rupture of a muscle or tendon.
Tenderness
Localized, deep referred tenderness may occur within a painful region, for example, as the result of compression of the dura mater usually by a small displaced fragment of the intervertebral disc. This phenomenon is described in Chapter 1 and can be very deceptive unless the examiner is familiar with the rules of pain reference.
Palpation of the moving joint
Next, the moving joint is palpated. The examiner may either experience crepitus or clicks, or can assess end-feel or mobility (see Fig. 4.10b).
Crepitus
Muscular crepitus
This is observed in two situations only:
• Tenosynovitis of the two extensors and of the long abductor of the thumb in the distal part of the forearm is usually accompanied by crepitus that can be felt locally. The crepitus is, however, sometimes felt throughout the muscle bellies, possibly as far up as the elbow (see p. 524).
• Localized crepitus is usually felt in a lesion at the musculotendinous junction of the tibialis anterior muscle.
End-feel
End-feel can be assessed when a passive movement comes to a stop. It is either physiological or pathological and has important diagnostic and therapeutic consequences (see pp. 64–65).
Hypermobility and hypomobility
These are terms that are currently used by osteopaths and manual therapists.24–25 During their so-called ‘segmental examination’ they claim to be able to feel the difference in mobility between different, mostly spinal, joints.26 To establish hyper- or hypomobility would afford an excellent guide to the level of the lesion if it were always at the joint in which the fault lay, which is not in fact the case. Moreover, these findings are so subjective that they are not verifiable or reproducible. It has been shown on different occasions that even experienced osteopaths or therapists cannot agree about the findings.27–31 The main mistake, however, consists in attributing diagnostic significance to such differences in mobility. When movement in a hypomobile or hypermobile joint strongly evokes the patient’s symptoms, this has to be considered as the best criterion and clearly shows where the lesion must lie. However, when the abnormal mobility does not elicit the known symptoms, the problem clearly has nothing to do with the hypermobile joint.32–34 Furthermore, there are no universal standards to determine abnormal mobility. What is normal for one person can be abnormal for another. Hypermobility can be physiological up to a certain level, especially in women, and hypomobility can also be considered as normal, particularly in the elderly. When hypermobility gives rise to symptoms, then and then only can it be considered as pathological. The terms ‘laxity’ and ‘instability’ are then used. The end-feel will add greatly to this conclusion.
Diagnostic infiltration or aspiration
Diagnostic local anaesthesia
This approach is useful in the following circumstances:
• When the examiner is not certain about a diagnosis or when the examiner wants positive confirmation of a tentative diagnosis, the induction of a local anaesthetic may help.
• For lesions in the extremities, infiltration is particularly useful and gives reliable answers. However, it is not useful on the posterior aspect of the trunk: paraspinal infiltrations may give temporary relief but have no diagnostic value.
• In difficult cases this approach may be the final ‘court of appeal’.
Technical investigations
It should be stressed again that there still remains a huge discrepancy between discovered anatomical changes and existing pain and disability. During the last decades the medical profession has focused on, and been fascinated by, techniques of imaging that can clearly show existing anatomical aberrations. However, very often, these anatomical changes are not the source of the pain because they appear to exist also in large groups of symptomless individuals. For example, the prevalence of herniated lumbar discs in a normal asymptomatic population ranges from 35%–50%.35–41 Evidence of cervical discopathy is also found in asymptomatic subjects42–44 and there is not always good concordance between the different imaging techniques.45 In the shoulder, echography can discover partial thickness and full thickness ruptures of the rotator cuff even in large asymptomatic groups.46–49 The finding of asymptomatic anatomical changes in knee joints during arthroscopy is not uncommon.50,51
In orthopaedic medicine, technical examinations are not routinely performed but are instead used only when necessary to refine the clinical diagnosis, to exclude certain lesions or to clarify differential diagnosis. They are always undertaken when the history and/or functional examination have revealed warning signs (Box 4.12).
The clinician should not ascribe too much diagnostic importance to technical investigations – a positive answer does not always identify with certainty the condition present. The reverse also holds: a negative picture does not always mean that there is nothing wrong. Knowing when to ignore a positively or negatively misleading picture comes only from proper clinical examination (see Box 4.13). The latter always remains the most important of the tools available and it is far more dangerous to omit a proper clinical examination and rely on technical investigations than to do the reverse.
Interpretation
Interpretation is only possible if the clinical examination has been performed correctly: a detailed history, followed by inspection and a careful functional examination. Every part of the examination may be important, and consequently a complete examination should be carried out on each occasion. Cyriax stated ‘Omission of part of this examination, because the diagnosis seems obvious or to save time, is the common source of error’.52 Examining patients may become a routine and repetitive, with the same features being frequently encountered so that it is tempting to omit that part of the examination which is expected to be negative. By doing this, the presence of a double lesion can easily be overlooked or, even worse, the signs of an uncommon (possibly serious?) disorder (one of the classic ‘warning signs’) may be missed.
In practice one of a number of patterns can emerge (see Box 4.14).
Impairment of active movements
In combination with impairment of passive movements
The response to active movements (Fig. 4.11) may correspond with that found on passive testing. When an active movement is found to be painful, passive movement in the same direction will usually be more painful. In this case, the passive movement must be considered as the important one and the response to it is used for interpretation (see pp. 73–77). When the active movement is limited, passive movement is usually also restricted, although it should be possible to go a little further in the limited direction.
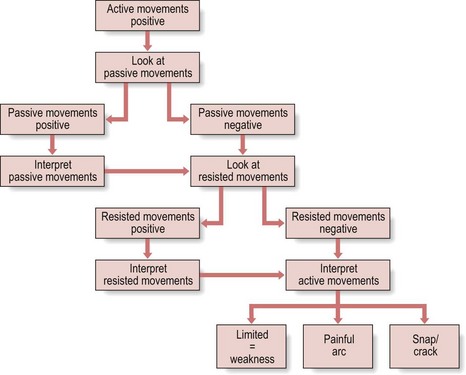
Fig 4.11 Response to active movements.
In combination with impairment of resisted movements
When an active movement hurts and the same movement performed against resistance is also painful, the latter has to be considered as being most important (see pp. 77–78). Limitation of an active movement and not of the corresponding passive one indicates gross weakness. The same movement performed against resistance usually also proves to be weak. Sometimes, however, other (accessory) tests against resistance must be done to uncover the lesion.
In isolation
One or more active movements are limited but are full range on passive movement
This occurs when one or more muscles are out of action. The resisted movements aimed to test the same muscles will also be weak. Weakness is quite often encountered in orthopaedic medical disorders. It may be of organic type or functional type (Fig. 4.12).
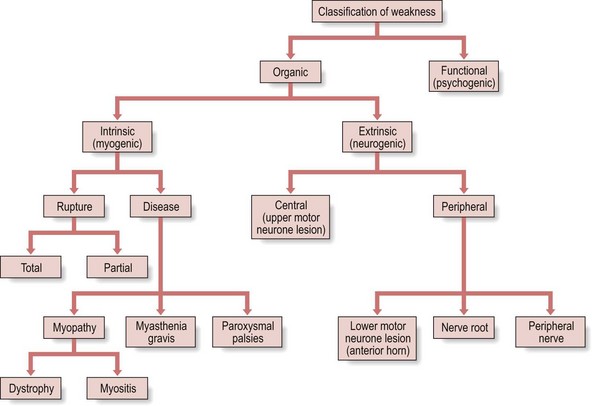
Fig 4.12 Classification of weakness.
Intrinsic (myogenic) lesions are the result of either a structural disorder, such as a severe partial or a total rupture of muscle or tendon, myopathy (e.g. muscular dystrophy or myositis) or a biochemical disorder (e.g. myasthenia gravis or paroxysmal palsies). Extrinsic (neurogenic) lesions may be either central or peripheral (Table 4.2).
Table 4.2
Differences between central and peripheral palsies
| Central | Peripheral |
| Muscular hypertonus | Muscular hypotonus |
| Hyperreflexia | Hyporeflexia |
| No muscular atrophy | Muscular atrophy |
| Upper skin reflexes disappear | |
| Lower skin reflexes appear |
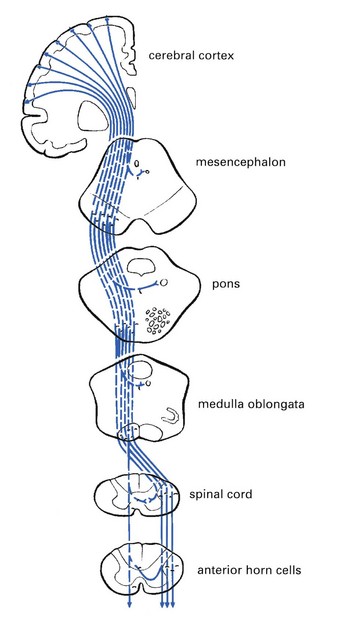
Central palsy
A central palsy is the result of a lesion of the upper motor neurone (i.e. the corticospinal and/or corticonuclear tracts), caused by a vascular condition, a tumour, trauma or disease (e.g. encephalitis or multiple sclerosis) in the region between the cerebral cortex and the spinal cord (Fig. 4.13). Hemiplegia, monoplegia, paraplegia or quadriplegia follows, characterized by muscular hypertonus, hyperreflexia, disappearance of the upper skin reflexes and appearance of abnormal skin reflexes (e.g. the Babinski reflex). Because the cells in the anterior horn of the spinal cord are not affected, there is no muscular atrophy apart from some slight wasting because of the patient’s inactivity.
Impairment of passive movements
Positive passive movements in combination with negative resisted movements draw attention to the inert structures, although they do not unconditionally exclude a lesion of contractile tissue (see Fig. 4.14).
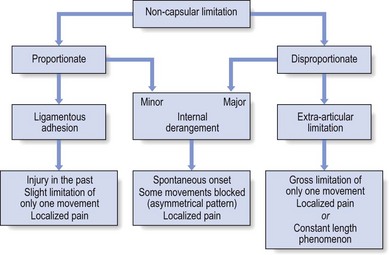
Limited range
Non-capsular patterns or partial articular limitation
In contrast to the capsular pattern a non-capsular pattern is less well defined, but for each joint different patterns may occur, all of which do differ from the capsular pattern (see Fig. 4.15).
Internal derangement
Two different types of limitation occur:
Proportionate derangement. When the displaced fragment is small and lies in such a position that it does not greatly hinder the function of the joint, restriction of movement is also small by comparison with normal movement. The picture may very well mimic the proportionate limitation in ligamentous adhesions but the absence of an injury and the short history exclude this possibility. A typical example is the loose body in an arthrotic knee: flexion is 15–30° limited and the pain is felt at the inner side.
Disproportionate derangement. A large displacement causes gross limitation of movement in some directions and full or almost full range in other directions – an asymmetrical pattern. This is a well-known clinical picture in acute lumbago. Two or three trunk movements are totally blocked and one movement, usually one lateral flexion, is scarcely limited.
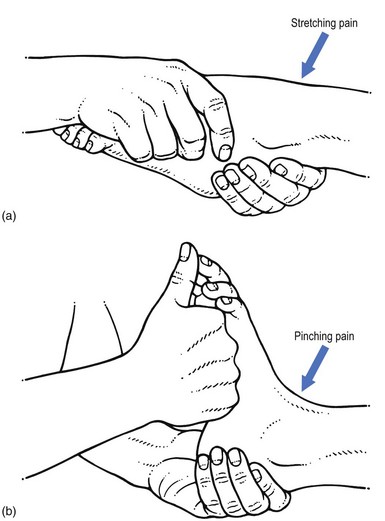
Full range
When no limitation of movement exists on passive testing, the picture may be difficult to interpret. The site of pain usually helps to determine whether it is caused by stretching or by pinching of the affected tissue (Fig. 4.16).
Impairment of resisted movements
In combination with impairment of other resisted movements
Relationship of pain and strength
Resisted movements test for strength and pain. The patterns that emerge are usually a combination of strength or weakness and the presence or absence of pain. In practice, four combinations may occur (Table 4.3).
Table 4.3
Relationship of pain and strength in resisted movement
| Pain | Strength | Disorder |
| − | Normal | − |
| + | Normal | Contractile tissue |
| − | Weak | Nervous lesion |
| Complete rupture | ||
| + | Weak | Serious lesion |
| Partial rupture |
Diagnostic difficulties
Difficult clinical pictures
A patient may present the symptoms and signs of a genuine, although minor, lesion which is overshadowed by psychogenic features. The picture is correct in quality, but grossly excessive in quantity. The examiner recognizes the truth within the patient’s story but finds that it is interwoven with unlikelihoods and improbable signs are mixed up with the genuine findings (see online chapter Psychogenic pain).
The clinical approach in orthopaedic medicine is summarized in Fig. 4.18.
References
1. Takatalo, J, Karppinen, J, Niinimäki, J, et al, Does lumbar disc degeneration on MRI associate with low back symptom severity in young Finnish adults? Spine (Phila PA 1976), 2011 Feb 24. ![]()
2. Ernst, CW, Stadnik, TW, Peeters, E, et al, Prevalence of annular tears and disc herniations on MR images of the cervical spine in symptom-free volunteers. Eur J Radiol. 2005;55(3):409–414. ![]()
3. Wood, KB, Garvey, TA, Gundry, C, Heithoff, KB, Magnetic resonance imaging of the thoracic spine. Evaluation of asymptomatic individuals. J Bone Joint Surg Am. 1995;77(11):1631–1638. ![]()
4. Hirano, Y, Sashi, R, Izumi, J, et al, Comparison of the MR findings on indirect MR arthrography in patients with rotator cuff tears with and without symptoms. Radiat Med. 2006;24(1):23–27. ![]()
5. Reilly, P, Macleod, I, Macfarlane, R, et al, Dead men and radiologists don’t lie: a review of cadaveric and radiological studies of rotator cuff tear prevalence. Ann R Coll Surg Engl. 2006;88(2):116–121. ![]()
6. Yamamoto, A, Takagishi, K, Kobayashi, T, et al, Factors involved in the presence of symptoms associated with rotator cuff tears: a comparison of asymptomatic and symptomatic rotator cuff tears in the general population. J Shoulder Elbow Surg 2011 Mar 29; . ![]()
7. Kim, HM, Teefey, SA, Zelig, A, et al, Shoulder strength in asymptomatic individuals with intact compared with torn rotator cuffs. J Bone Joint Surg Am. 2009;91(2):289–296. ![]()
8. Soder, RB, Simões, JD, Soder, JB, Baldisserotto, M, MRI of the knee joint in asymptomatic adolescent soccer players: a controlled study. AJR Am J Roentgenol. 2011;196(1):W61–W65. ![]()
9. Kaplan, LD, Schurhoff, MR, Selesnick, H, et al, Magnetic resonance imaging of the knee in asymptomatic professional basketball players. Arthroscopy. 2005;21(5):557–561. ![]()
10. Christensen, HW, Nilsson, N, The reliability of measuring active and passive cervical range of motion: an observer-blinded and randomized repeated-measures design. J Manipulative Physiol Ther. 1998;21(5):341–347. ![]()
11. Pellecchia, GL, Paolino, J, Connell, J, Intertester reliability of the Cyriax evaluation in assessing patients with shoulder pain. J Orthop Sports Phys Ther. 1996;23(1):34–38. ![]()
12. Chesworth, BM, MacDermid, JC, Roth, JH, Patterson, SD, Movement diagram and ‘end-feel’ reliability when measuring passive lateral rotation of the shoulder in patients with shoulder pathology. Phys Ther. 1998;78(6):593–601. ![]()
13. Wong, A, Nansel, DD, Comparisons between active vs. passive end-range assessments in subjects exhibiting cervical range of motion asymmetries. J Manipulative Physiol Ther. 1992;15(3):159–163. ![]()
14. Youdas, JW, Carey, JR, Garrett, TR, Reliability of measurements of cervical spine range of motion – comparison of three methods. Phys Ther. 1991;71(2):98–104. ![]()
15. Fritz, JM, Delitto, A, Erhard, RE, Roman, M, An examination of the selective tissue tension scheme, with evidence for the concept of a capsular pattern of the knee. Phys Ther. 1998;78(10):1046–1056. ![]()
16. Hanchard, NC, Howe, TE, Gilbert, MM, Diagnosis of shoulder pain by history and selective tissue tension: agreement between assessors. J Orthop Sports Phys Ther. 2005;35(3):147–153. ![]()
17. Cyriax, JH. Textbook of Orthopaedic Medicine, vol I: Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.
18. Donelson, R, Silva, G, Murphy, K, Centralization phenomenon, its usefulness in evaluating and treating referred pain. Spine. 1990;15(3):211–213. ![]()
19. Donelson, R, Aprill, C, Medcalf, R, Grant, W, A prospective study of centralisation of lumbar and referred pain. Spine. 1997;22(10):1115–1122. ![]()
20. Wyke, W. Neurological mechanisms in the experience of pain. Acupunc Electrother Res J. 1979; 4:27.
21. Wyke, BD. The neurology of low back pain. In Jayson MIV, ed.: The Lumbar Spine and Back Pain, 2nd ed, Kent: Pitman Medical, 1980.
22. Veys, EM, Mielants, H, Verbruggen, G. Reumatologie. Ghent: Omega Editions; 1985.
23. Hayes, KW, Petersen, CM, Reliability of assessing end-feel and pain and resistance sequence in subjects with painful shoulders and knees. J Orthop Sports Phys Ther. 2001;31(8):432–445. ![]()
24. Greenman, PE. Principles of Manual Medicine. Baltimore: William & Wilkins; 1989.
25. Twomey, LT, Taylor, JR. Physical Therapy of the Low Back. New York: Churchill Livingstone; 1987.
26. Jones, MA, Jones, HM. Principles of the physical examination. In: Boyling JD, Palastanga N, eds. Grieve’s Modern Manual Therapy, The Vertebral Column. Edinburgh: Churchill Livingstone; 1994:491–501.
27. Panzer, DM, The reliability of lumbar motion palpation. J Manipulative Physiol Ther. 1992;15(8):518–524. ![]()
28. Matyas, T, Bach, T. The reliability of selected techniques in clinical arthrometics. Aust J Physiother. 1985; 31:175–199.
29. Hardy, GL, Napier, JK. Inter- and intratherapist reliability of passive accessory movement and technique. NZ J Physiother. 1991; 22–24.
30. Fjellner, A, Bexander, C, Faleij, R, Strender, LE, Interexaminer reliability in physical examination of the cervical spine. J Manipulative Physiol Ther. 1999;22(8):511–516. ![]()
31. Vincent-Smith, B, Gibbons, P, Inter-examiner and intra-examiner reliability of the standing flexion test. Manual Therapy. 1999;4(2):87–93. ![]()
32. Maher, C, Latimer, J. Pain or resistance – the manual therapists’ delimma. Aust J Physiother. 1992; 38:257–260.
33. Keating, J, Bergman, T, Jacobs, G, Bradley, D, Finer, A, Larson, K, Inter-examiner reliability of eight evaluative dimensions of lumbar segmental abnormality. J Manipulative Physiol Ther 1990; 13:463–470. ![]()
34. Potter, N, Rothstein, J, Intertester reliability for selected clinical tests of the sacroiliac joint. Phys Ther 1985; 65:1671–1675. ![]()
35. MacRae, DL, Asymptomatic intervertebral disc protrusion. Acta Radiologica 1956; 46:9. ![]()
36. Hitselberger, WE, Whitten, RM, Abnormal myelograms in asymptomatic patients. J Neurosurg 1968; 28:204. ![]()
37. Wiesel, SW, Tsourmas, N, Feffer, HL, Citrin, CM, Patronas, N, A study of computer-assisted tomography: 1. The incidence of positive CAT scans in an asymptomatic group of patients. Spine 1984; 9:549–551. ![]()
38. Powell, MC, Wilson, M, Szypryt, P, Symonds, EM, Prevalence of lumbar disc degeneration observed by magnetic resonance in symptomless women. Lancet 1986; 13:1366–1367. ![]()
39. Weinreb, JC, Wolbarsht, LB, Cohen, JM, Brown, CE, Maravilla, KR, Prevalence of lumbosacral intervertebral disc abnormalities on MR images in pregnant and asymptomatic non-pregnant women. Radiology 1989; 170:125–128. ![]()
40. Boden, SD, Davis, DO, Dina, TS, Patronas, MJ, Wiesel, SW, Abnormal magnetic resonance scans of the lumbar spine in asymptomatic subjects. J Bone Joint Surg 1990; 72A:403–408. ![]()
41. Buirski, G, Silberstein, M, The symptomatic lumbar disc in patients with low-back pain. Magnetic resonance imaging appearances in both a symptomatic and control population. Spine 1993; 18:1808–1811. ![]()
42. Matsumoto, M, Fujimura, Y, Suzuki, N, Nishi, Y, Nakamura, M, Yabe, Y, Shiga, H, MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg (Br). 1998;80(1):19–24. ![]()
43. Humphreys, SC, Hodges, SD, Fisher, DL, Eck, JC, Covington, LA, Reliability of magnetic resonance imaging in predicting disc material posterior to the posterior longitudinal ligament in the cervical spine. A prospective study. Spine. 1998;23(22):2468–2471. ![]()
44. Kaiser, JA, Holland, BA, Imaging of the cervical spine. Spine. 1998;23(24):2701–2712. ![]()
45. Shafaie, FF, Wippold, FJ, 2nd., Gado, M, Pilgram, TK, Riew, KD, Comparison of computed tomography myelography and magnetic resonance imaging in the evaluation of cervical spondylotic myelopathy and radiculopathy. Spine. 1999;24(17):1781–1785. ![]()
46. Thompson, WO, Debski, RE, Boardman, ND, 3rd., Taskiran, E, Warner, JJ, Fu, FH, Woo, SL, A biomechanical analysis of rotator cuff deficiency in a cadaveric model. Am J Sports Med. 1996;24(3):286–292. ![]()
47. Petersson, CJ, Ruptures of the supraspinatus tendon. Cadaver dissection. Acta Orthop Scand. 1984;55(1):52–56. ![]()
48. Jerosch, J, Muller, T, Castro, WH, The incidence of rotator cuff rupture. An anatomic study. Acta Orthop Belg. 1991;57(2):124–129. ![]()
49. Kummer, FJ, Zuckerman, JD, The incidence of full thickness rotator cuff tears in a large cadaveric population. Bull Hosp Dis. 1995;54(1):30–31. ![]()
50. Jerosch, J, Castro, WH, Assheuer, J, Age-related magnetic resonance imaging morphology of the menisci in asymptomatic individuals. Arch Orthop Trauma Surg. 1996;105(3–4):199–202. ![]()
51. LaPrade, RF, Burnett, QM, 2nd., Veenstra, MA, Hodgman, CG, The prevalence of abnormal magnetic resonance imaging findings in asymptomatic knees. With correlation of magnetic resonance imaging to arthroscopic findings in symptomatic knees. Am J Sports Med. 1994;22(6):739–745. ![]()
52. Cyriax, JH. Textbook of Orthopaedic Medicine, vol I: Diagnosis of Soft Tissue Lesions, 8th ed. London: Baillière Tindall; 1982.