Esophagogastric Tamponade Tube
Esophagogastric tamponade therapy is used to provide temporary control of bleeding from gastric or esophageal varices.2
PREREQUISITE NURSING KNOWLEDGE
• Tamponade therapy exerts direct pressure against the varices with the use of a gastric or esophageal balloon and may be used for cases that are unresponsive to medical therapy or that are too hemodynamically unstable for endoscopy or sclerotherapy.1,3
• Esophagogastric tamponade tubes are used to control bleeding from either gastric or esophageal varices. The suction lumens allow the evacuation of accumulated blood from the stomach or esophagus. The suction lumens also allow for the intermittent instillation of saline solution to assist in the evacuation of blood or clots.
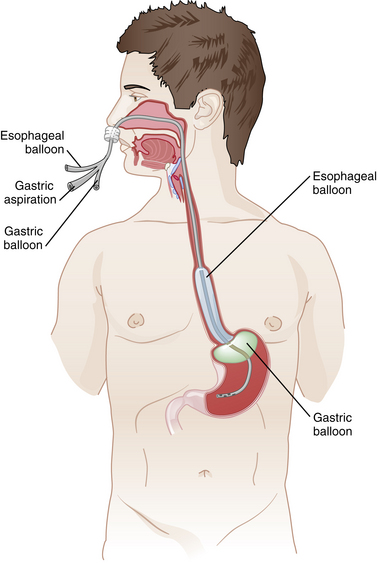
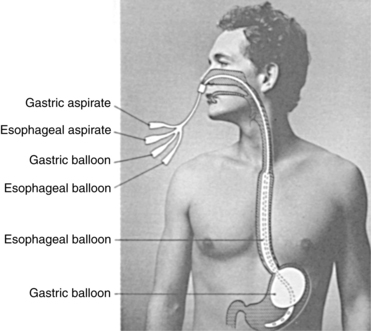
• Three types of tubes are available for esophagogastric tamponade therapy. The two most common are the Sengstaken-Blakemore (C.R. BARD, Inc., Covington, Georgia) tube (Fig. 104-1) has a gastric and esophageal balloon and a gastric suction lumen. The four-lumen Minnesota tube (Fig. 104-2) has gastric and esophageal balloons and separate gastric and esophageal suction lumens. The third, the Linton or Linton-Nachlas tube, (Mallinckrodt Inc. Tyco Health Care Group, Hampshire, UK) has a gastric balloon and separate gastric and esophageal suction lumens and is used only for treatment of bleeding gastric varices. The Minnesota tube is considered the preferred tube for esophagogastric tamponade therapy because it allows for suction above and below the balloons.
• Esophagogastric tamponade tubes may be introduced via either the nasogastric or the orogastric route. The tubes are then advanced through the oropharynx and esophagus and into the stomach.
• Contraindications include esophageal strictures or recent esophageal surgery, congestive heart failure, respiratory failure, hiatal hernia, and cardiac dysrhythmias.3 Because of the risk for aspiration, the patient may need endotracheal intubation for airway protection.
• Sedation should be considered, but dosing should be individualized on the basis of the likelihood of liver injury with its concomitant alteration in the metabolism of medications. The plan for sedation is individualized with the goal of achieving patient comfort through a safe use of medications if needed.
• Head of bed (HOB) should be at least 30 to 45 degrees at all times to reduce risk of aspiration.6
EQUIPMENT
• Tamponade tube (Sengstaken-Blakemore, Minnesota, or Linton-Nachlas)
• Irrigation kit (or catheter-tip, 60-mL syringe and basin)
• Nasogastric (NG) tubes (one for Sengstaken-Blakemore tube)
• Normal saline (NS) solution for irrigation
• NS solution, 500 mL (provides weight for traction on the tube)
• Sphygmomanometer or pressure gauge
• Two suction setups and tubing
• Endotracheal suction equipment
• Emergency medications, including atropine
• Emergency equipment, including transcutaneous pacemaker and intubation equipment
Additional equipment (to have available based on patient need) includes the following:
• Rubber cube sponge (used for nasal tamponade tube placement)
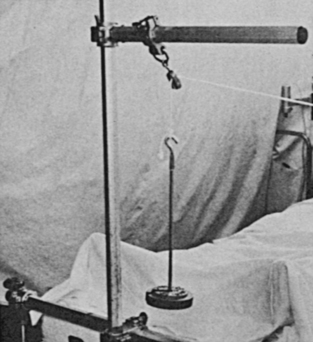
• Balanced suspension traction apparatus with 1 pound of weights, 500 mL of NS solution (Fig. 104-3), or football helmet with face mask (Figs. 104-4)

Figure 104-4 Tamponade tube secured in position with helmet.
• Lopez enteral valve (Fig. 104-5)7 (ICU, Medical, San Clemente, CA), a three-way stopcock used to attach a 60-mL catheter-tip syringe and the handheld manometer to the Minnesota tube
PATIENT AND FAMILY EDUCATION
• Explain the procedure and reason for the tube insertion.  Rationale: Patient anxiety may be decreased.
Rationale: Patient anxiety may be decreased.
• Explain the patient’s role in assisting with the passage of the tube and maintenance of tamponade traction.  Rationale: Patient cooperation is elicited during the insertion and tamponade therapy.
Rationale: Patient cooperation is elicited during the insertion and tamponade therapy.
• Explain that the procedure can be uncomfortable because the gag reflex may be stimulated, causing the patient to be nauseated or to vomit.  Rationale: Patient cooperation is elicited during the insertion.
Rationale: Patient cooperation is elicited during the insertion.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess signs and symptoms of major blood loss:
 Decreased filling pressures (pulmonary artery pressure, pulmonary capillary wedge pressure and central venous pressure)
Decreased filling pressures (pulmonary artery pressure, pulmonary capillary wedge pressure and central venous pressure)
 Rationale: Esophageal or gastric varices can cause significant blood loss.
Rationale: Esophageal or gastric varices can cause significant blood loss.
• Assess the baseline cardiac rhythm.  Rationale: Passage of a large-bore tube into the esophagus may cause vagal stimulation and bradycardia.
Rationale: Passage of a large-bore tube into the esophagus may cause vagal stimulation and bradycardia.
• Assess the baseline respiratory status (i.e., rate, depth, pattern, and characteristics of secretions).  Rationale: Use of topical anesthetic agents in the nares or oropharynx may alter the gag or cough reflex, increasing the risk for aspiration. Passage of a large-bore tube may impair the airway. Large amounts of blood in the stomach predispose a patient to vomiting and potential aspiration.
Rationale: Use of topical anesthetic agents in the nares or oropharynx may alter the gag or cough reflex, increasing the risk for aspiration. Passage of a large-bore tube may impair the airway. Large amounts of blood in the stomach predispose a patient to vomiting and potential aspiration.
• Assess the patient’s ability to protect the airway.  Rationale: Multiple factors can influence the patient’s ability to protect the airway, including presence of vomiting and depressed mental status.
Rationale: Multiple factors can influence the patient’s ability to protect the airway, including presence of vomiting and depressed mental status.
• Assess the mental status.  Rationale: Patients with altered mental status should be intubated and mechanically ventilated prophylactically to prevent airway complications.
Rationale: Patients with altered mental status should be intubated and mechanically ventilated prophylactically to prevent airway complications.
• If anticipating a nasal esophageal tube placement:
 Absolute contraindications include a history of transphenoidal hypophysectomy.
Absolute contraindications include a history of transphenoidal hypophysectomy.  Rationale: This type of surgical procedure may predispose placement of the tube into the cranial vault.
Rationale: This type of surgical procedure may predispose placement of the tube into the cranial vault.
 Assess for medical history of nasal deformity, surgery, trauma, epistaxis, or coagulopathy.
Assess for medical history of nasal deformity, surgery, trauma, epistaxis, or coagulopathy.  Rationale: The risk for complications and bleeding with nasal insertion is increased.
Rationale: The risk for complications and bleeding with nasal insertion is increased.
 Evaluate patency of nares. Occlude one naris at a time, and ask the patient to breathe through the nose. Select the naris with the best airflow.
Evaluate patency of nares. Occlude one naris at a time, and ask the patient to breathe through the nose. Select the naris with the best airflow.  Rationale: Choosing the most patent naris eases insertion and may improve patient tolerance of the tube.
Rationale: Choosing the most patent naris eases insertion and may improve patient tolerance of the tube.
 The nasal route is not recommended in patients with coagulopathy.
The nasal route is not recommended in patients with coagulopathy.  Rationale: The risk for bleeding and complications is increased.
Rationale: The risk for bleeding and complications is increased.
Patient Preparation
• Ensure that the patient and family understand preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Measure the tube from the bridge of the nose to the earlobe to the tip of the xiphoid process. Mark the length of tube to be inserted.  Rationale: Estimating the length of tube to be inserted helps place the distal tip in the stomach.
Rationale: Estimating the length of tube to be inserted helps place the distal tip in the stomach.
• If the patient is alert, place the patient in high Fowler’s or semi-Fowler’s position. If the patient is unconscious or obtunded, place the patient head down in the left lateral position.  Rationale: Positioning facilitates the passage of the tube into the stomach and reduces the risk for aspiration.
Rationale: Positioning facilitates the passage of the tube into the stomach and reduces the risk for aspiration.
References
1. Bard MedicalBard Medical DivisionCovington. GAInstructions for passing Minnesota four lumen esophagogastic tamponade tube for the control of bleeding from esophageal varicies. 8195 Industrial Boulevard, 30014; 2006.
2. Christensen, T, Christensen, M. The implementation for guideline of care for patients with Sengstaken-Blakemore tube in situ in a general intensive care unit using transitional change theory. Intensive Crit Care Nurs. 2007; 23:234–242.
3. Day, M. Gastrointestinal bleeding. In: Carlson K, ed. Advanced critical care nursing. St Louis: Saunders; 2009:748–751.
4. Hilinski, A, Stark, ML. Memory aide to reduce the incidence of ventilator-associated pneumonia. Crit Care Nurse. 2006; 26(5):80–81.
5. Isaacs, KL, Balloon tamponade. handbook of gastroenterologic procedures. ed 4. Lippincott Williams & Wilkins, Philadelphia, 2005:119–120. www.findarticles.com/p/articles/mi [retrieved August 17, 2009, from].
6. Mallinckrodt Inc, Tyco Health Care Group, 154 fareham road gosport, hampshire, UK, po 13 oas. Linton-Nachlas tube. April 19, 2009 retrieved. www.gpnotebook.co.uk/simplepage.cfm [from].
7. Martin, RK, Hassanein, T, Liver dysfunction and failure Carlson KK, ed.. Advanced critical care nursing. Saunders/Elsevier: Philadelphia, 2009:759–764.
8. Treger, R, Graham, TP, Dea, SK, Sengstaken-Blakemore tube. treatment & medication,. http//emedicine.medscape.com/article/-81020-treatment, 2008 [retrieved April1, 2009, from].