Z-Plasty
Introduction
The history of Z-plasty has been reviewed by Borges1 and Davis and Renner.2 Classically, this technique involves designing a Z with three limbs of equal length that form two triangular flaps of equal angles. The triangles represent angular flaps that are interchanged with each other by both pivotal and advancement tissue movement. Although the initial description of transposing equilateral triangular flaps was by Berger3 in 1904, numerous other descriptions have been recorded. In the 1800s, Fricke,4 Horner,5 Serre,6 and Denonvilliers7 described the transposition of cheek and temporal skin to correct eyelid ectropion and regional defects. However, in these case descriptions, the triangular flaps transposed did not have equal angles, nor were they the same size. In the late 1920s, Limberg elucidated the geometric principles involved with Z-plasty.8 He also noted that Z-plasties as well as the related Limberg or rhombic flap are best described as having both pivotal and advancement components. Whereas the classic Z-plasty follows specific geometric guidelines, Limberg demonstrated the flexibility of double transposition flaps that have a Z-plasty design. It is this flexibility that allows the wide-ranging applications and variations from the classic description.
Geometry and Design
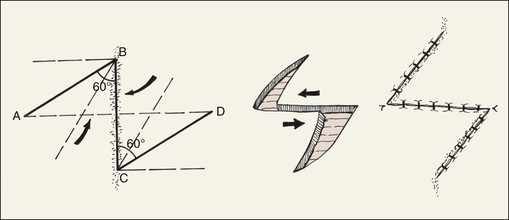
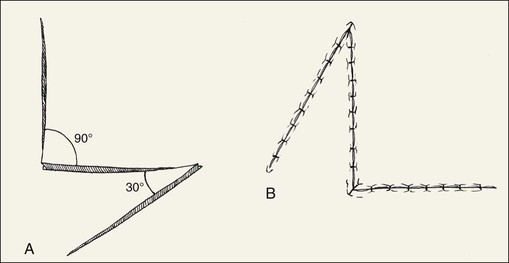
The classic description of Z-plasty consists of a design in which the central limb and two peripheral limbs are in the shape of a Z such that two triangle-shaped flaps of equal size are created. All three limbs are of identical length, and the central limb consists of the scar that is to be lengthened or realigned. In the standard 60° Z-plasty (Fig. 14-1), a protractor may be used to measure the angles. However, a more practical means of estimating Z-plasty angles is to mark out a 90° angle and to divide it into thirds. A caliper or ruler is useful in the design of limbs of equal lengths. Transposition of the triangular flaps (angles ABC and BCD in Fig. 14-1) results in the following changes: the axis of the central limb is rotated 90° (in the example, a vertical scar is changed to a horizontal orientation); the distance between the points labeled B and C of the original central limb is increased; and the final scar is changed from a straight line to a nonlinear Z configuration. The overall length of the new scar created by the Z-plasty is increased by the sum of the length of the peripheral limbs of the Z.
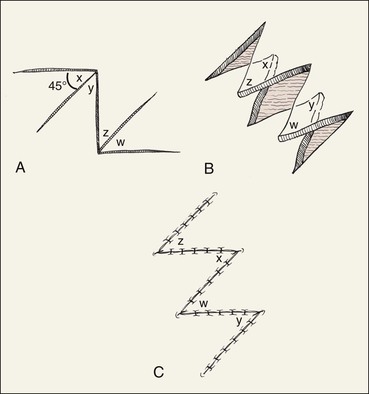
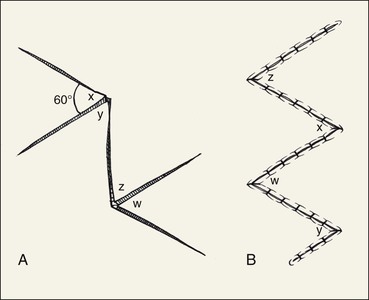
Although a 60° Z-plasty is perhaps the most common design, angles between 30° and 90° are possible. Changing the angle of the flaps will cause a change in the length gained in the axis of the original central limb (B-C in Fig. 14-1). Theoretically, the percentage gain in length increases with larger angles (Fig. 14-2 and Table 14-1). However, the amount of lengthening noted in actual practice is usually less.
TABLE 14-1
Theoretical Increase in Length of Central Limb of Z-Plasty
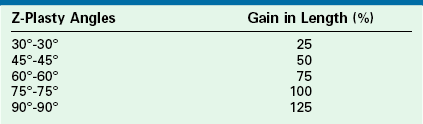
From Frodel JL, Wang TD: Z-plasty. In Baker SR, Swanson NA, editors: Local flaps in facial reconstruction, St. Louis, Mosby, 1995.
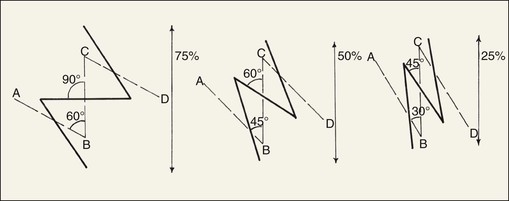
FIGURE 14-2 Length gained in contracted scar and change in orientation of central limb of Z relative to Z-plasty angle. Greater Z-plasty angle causes greater change in scar orientation.
The degree of directional change of the central limb of the Z-plasty (B-C in Fig. 14-2) is also variable. In the 60° Z-plasty, the orientation of the central limb is changed 90° from its original orientation. In the 45° Z-plasty, the orientation of the central limb is changed approximately 60° from its original position. In the 30° Z-plasty, the change is approximately 45° (see Fig. 14-2). This relationship between the angle of the Z-plasty and the change in orientation of the central limb of the Z-plasty is an extremely important consideration in planning of Z-plasty (Table 14-2).
TABLE 14-2
Direction of Peripheral Limbs of Z in Relationship to RSTLs and Z-Plasty Design
| Variance to RSTLs | Z-Plasty Design |
| 90° | 60° Z |
| 60°-90° | 60° Z (try to follow RSTLs as much as possible) |
| 30°-60° | Parallel to RSTLs |
| 30° | Fusiform excision best |
RSTLs, relaxed skin tension lines.
From Davis WE, Renner GJ: Z-plasty. In Thomas JR, editor: Scar revision, St. Louis, Mosby–Year Book, 1989.
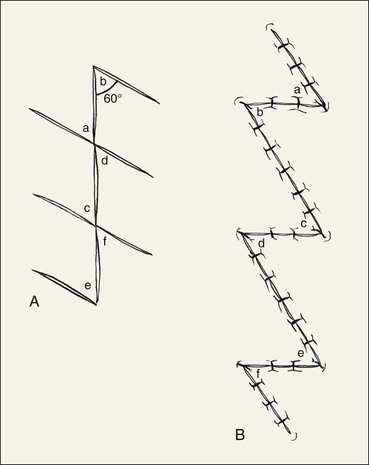
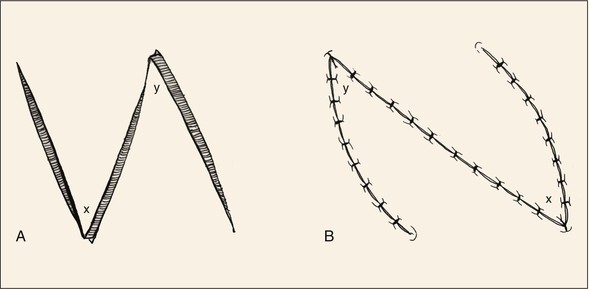
The initial length of the central limb affects the final outcome of Z-plasty. As the central limb of the Z is increased in length, so too is the gain in linear length between the points marking the ends of the central limb (points B and C in Fig. 14-1).9 Unfortunately, as the three limbs of the Z-plasty become longer, there is also a greater likelihood of a more apparent scar (Fig. 14-3). Multiple Z-plasties with shorter limbs to replace a single large Z-plasty with long limbs can circumvent this problem (Fig. 14-4). In this instance, a single long scar is divided into several smaller Z-plasties, usually with 60° angles.10 A single large 60° Z-plasty provides more gain in length than multiple small 60° Z-plasties along the same central limb.11 However, the aesthetic consequences and tissue availability for construction of the Z-plasty flaps often preclude the use of a single, large Z-plasty. On the face, limb length is usually limited to 1 cm or less. On the neck, limb length should not exceed 2 cm.
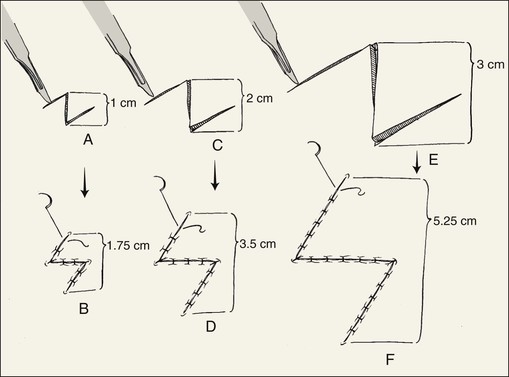
FIGURE 14-3 Length gained in contracted scar relative to length of Z-plasty limbs. Longer limbs are associated with greater scar lengthening.
In addition to the ability to vary limb length and angles of a Z-plasty, the actual design of a Z-plasty can be modified. One example is the four-flap Z-plasty. This technique increases the gain in length of the central limb by using four triangular flaps that are interposed between each other. A 90° Z-plasty is first designed, and then the 90° angle is bisected to design two 45° triangular flaps that are transposed (Fig. 14-5). Even greater gain in length of the central limb of a Z-plasty can be obtained by using 120° angles, which subsequently are bisected into four 60° flaps (Fig. 14-6). There are a number of variations on this theme, including a six-flap Z-plasty. However, the greater the number of flaps created, the greater is the total number of limbs and thus scars and the greater is the number of standing cutaneous deformities that develop when the flaps are transposed. Z-plasty may also be modified by use of flaps that have unequal angles. In such situations, the flap with the more acute angle is pivoted in a greater arc than that of the larger angled flap (Fig. 14-7). Minimal gain in length of the central limb will occur with unequal-angled Z-plasties. The main purpose of such designs is to transpose skin of the smaller angled flap to a more desirable location.2
Surgical Application and Technique
The discussion to this point has involved theoretical concerns about the classic geometry of Z-plasty. An understanding of the classic design is critical, but practical clinical considerations are even more important. Whereas length in the direction of the central limb is gained when a Z-plasty is used, it is usually not increased to the degree calculated.9 A number of studies have shown that the increase is considerably less in the clinical situation compared with the calculated gain.11 Similarly, there is a limit to the angles of the Z-plasty flaps that may be useful. Z-plasties less than 30° generally should not be used because of concern for vascularity of the narrow triangular flaps created by these acute angles. In the design of acutely angulated flaps, the width of the flap may be broadened by curving the limbs of the flap (Fig. 14-8). This modification may be useful in skin with an impaired blood supply, such as scar contracture associated with a burn or previous irradiation. Conversely, triangular flaps with angles greater than 75° will commonly produce standing cutaneous deformities that require excision. Thus, such large angled Z-plasties should be avoided whenever possible.
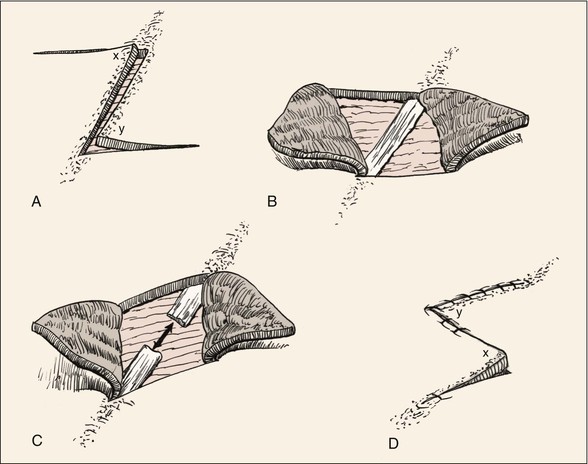
In designing a Z-plasty, evaluation of the surrounding skin and facial structures is necessary. Skin laxity at the base of each triangular flap of the Z-plasty must be adequate to allow proper pivotal movement of the flaps. If skin is contracted in a direction perpendicular to the central limb, Z-plasty may not be possible. Likewise, if a facial structure such as the eyelid, oral commissure, lip, or nasal ala is in proximity of the Z-plasty, distortion of these structures may occur. In planning of Z-plasty, it is also important to assess the degree of scar tissue in the central limb of the Z. The scar must be adequately resected or released to reduce resistance to transposition of the Z-plasty flaps (Fig. 14-9). Accordingly, it is essential to release and commonly to remove subcutaneous scar tissue.
A 60° Z-plasty will reposition the central limb 90°; more acutely angled Z-plasties will position the central limb less than this. An understanding of this concept will assist in proper positioning of Z-plasty limbs in relation to RSTLs. To reposition the central limb of a Z-plasty in RSTLs, the angles of the Z should be calculated accordingly. With scars located approximately 90° to RSTLs, a 60° Z-plasty is required to reposition the central limb parallel to RSTLs. As the axis of a scar in relationship to RSTLs becomes more acute, Z-plasty angles should become more acute to position the central limb and the two peripheral limb scars as parallel as possible to RSTLs (see Table 14-2).2 For scars less than 30° to RSTLs, Z-plasty may not be necessary for scar realignment. For every scar, there are always two choices for alignment of the peripheral limbs of a Z-plasty used to revise the scar. These are mirror images of one another. Both options should be considered. For scar camouflage, the selection of one of the alternatives is usually a better choice than the other because of the orientation of the resulting scar (Fig. 14-10).
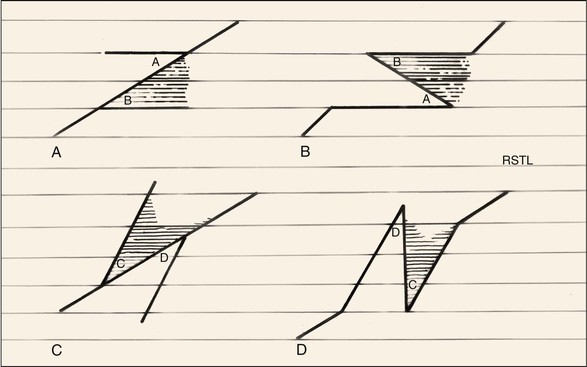
FIGURE 14-10 Two alternatives for design of Z-plasty: A-B and C-D. A-B is the preferred alternative as it best aligns scars with RSTLs.
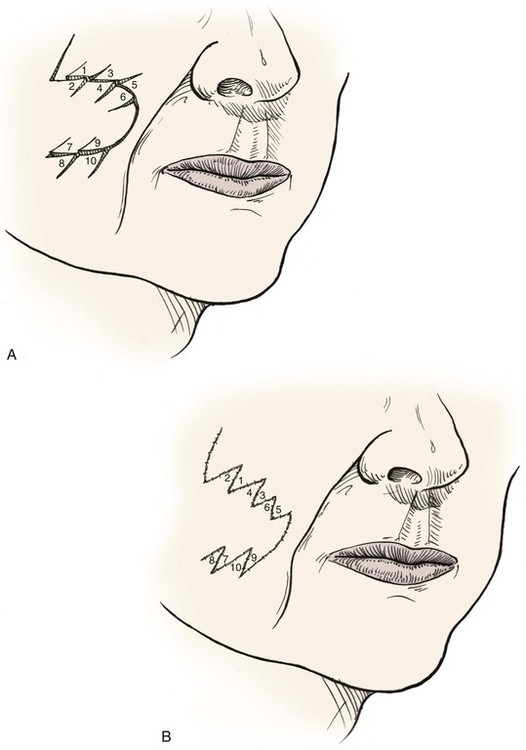
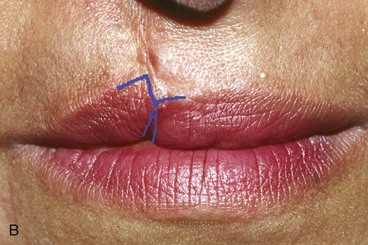
An example of a wide scar oriented perpendicular to the melolabial crease can be used to illustrate the surgical technique of Z-plasty (Fig. 14-11). Improvement in the appearance is achieved by realigning the scar by a Z-plasty to translocate the scar (central limb of the Z) into RSTLs, in this case the melolabial crease. Because the scar is aligned 90° to the crease, a 60° Z-plasty is the preferred design. This will change the axis of the central limb of the scar 90° to its original axis. Note that two options exist for the 60° Z-plasty design (see Fig. 14-11). Figure 14-11A illustrates the preferred design option. After transposition of the flaps, the central limb lies within the melolabial crease, and the two peripheral limbs approximate RSTLs of the lateral upper lip and medial cheek (Fig. 14-11C). Conversely, even though the mirror image Z-plasty (Fig. 14-11D) also realigns the central limb appropriately, the peripheral limbs of the Z-plasty have an undesirable orientation to RSTLs. Accordingly, the first option is optimal. Figure 14-12 shows the use of Z-plasty to align a scar with the melolabial crease. Because of the length of the scar, two Z-plasties were used to accomplish the reorientation of the scar. Whereas the overall scar length has been increased by the length of four peripheral limbs, the original scar (central limb of the Z) is transposed directly into the melolabial crease for maximal scar camouflage.
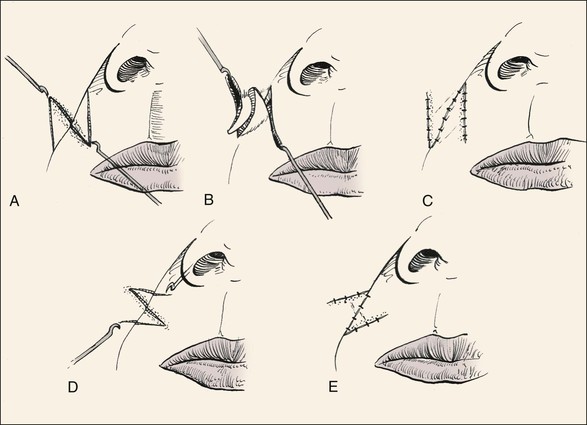
FIGURE 14-11 Two alternatives for design of Z-plasty to correct scar perpendicular to melolabial crease (A-C and D-E). The first alternative is preferred.




FIGURE 14-12 A, Scar with unfavorable orientation. B, Two Z-plasties designed to align scar with melolabial crease. C, Flaps transposed and wound repaired. D, Postoperative view at 6 months. (Courtesy Shan R. Baker.)
To perform a Z-plasty, the design is marked on the skin before injection of local anesthetic to avoid distortion of the skin. Proper limb length is precisely measured with a ruler or caliper. A sterile solution is used to prepare the skin, followed by injection of a local anesthetic. Significant undermining of the skin surrounding the flaps may be necessary to allow transposition of the flaps without distortion of facial structures, such as the lip, commissure, and alar base. Therefore, local anesthetic is injected to the extent of the anticipated undermining. After a 7- to 10-minute pause to ensure the maximal vasoconstrictive effect of the epinephrine contained in the anesthetic, the scar is excised. In cases in which the scar is wide, it is occasionally useful to temporarily suture the wound together to facilitate the design of the peripheral limbs of the Z-plasty. Incision of the peripheral limbs follows and is best accomplished with skin fixation and incision from the base of the triangular flap toward the apex. Because of skin retraction after release of the central limb scar, there is a tendency to incise the tips of the Z-plasty flaps such that they become overly narrowed. This tendency can be countered by slightly rounding and widening the incision where the peripheral limb joins the central limb of the Z-plasty. Conversely, the peripheral limbs may be incised before the central limb is. The flaps are dissected beginning at their tips. The tips are delicately retracted with a skin hook, and meticulous sharp dissection is performed in a tissue plane just within the subdermal fat. Dissection continues well beyond the flap bases. After appropriate undermining, the flaps are easily transposed by retraction of the ends of the central limb with skin hooks (Fig. 14-11B). On occasion, tension prohibits adequate transposition and necessitates further undermining and extension of the incision at the base of one or both of the flaps. The flaps are sutured in place beginning with placement of several subcutaneous sutures made of an absorbable material. However, the number of sutures should be limited so as not to compromise the vascularity of the flaps. Skin incisions are closed with fine (5-0 or 6-0) suture material by meticulous, atraumatic, wound-everting techniques. Cutaneous sutures are removed 3 to 5 days postoperatively.
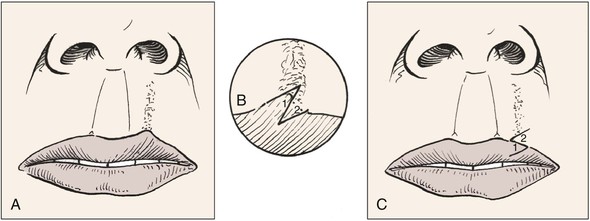
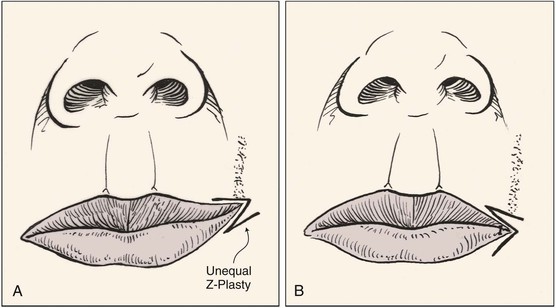
Lengthening of a contracted scar is often necessary, particularly if the scar is causing distortion of a facial structure and impairing function. An example of this is illustrated in Figure 14-13. In the illustration, the vermilion border is distorted by scar tissue. Such a condition may occur from a deep laceration of the upper lip or after cleft lip repair. Because additional length is required in the direction of the axis of the scar, a Z-plasty is designed with the central limb oriented along the axis of the scar. Transposition of the Z-plasty flaps results in an increased lip length in the scarred region and realignment of the vermilion border.
Similar to scars that restrict movement of the lip, long scars on the neck can impair the freedom of movement of the head (Fig. 14-14). A long, webbed scar on the neck is ideal for treatment with single or multiple Z-plasties. Z-plasty not only lengthens scars and corrects webbing but may also position scars in a better relationship to obliquely oriented RSTLs. Although a single large Z-plasty may provide maximum lengthening of a neck scar, the resulting scar will tend to be noticeable because of the long peripheral limbs of the Z. Accordingly, multiple Z-plasties are preferred in most circumstances (Fig. 14-14C, D).
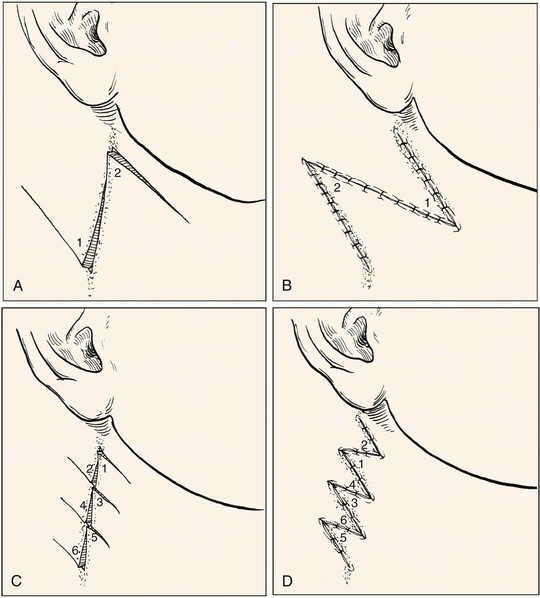
FIGURE 14-14 Z-plasty used to correct webbed neck scar. A, B, Single Z-plasty. C, D, Multiple Z-plasties.
Multiple Z-plasties may be of value in treating forehead scars by repositioning portions of the scar into horizontal forehead furrows (Fig. 14-15). Whereas the four-flap Z-plasty has few indications in the head and neck, it is occasionally useful for correction of lower eyelid ectropion or retraction (see Fig. 14-15). Multiple Z-plasties are also useful for improving the contour of curvilinear flaps that have trap-door deformities, such as might occur with a cheek transposition flap (Fig. 14-16). These deformities essentially result from scar contracture. Thus, an effective method of correcting trap-door deformity is scar lengthening achieved with Z-plasty and simultaneous contouring of the flap.
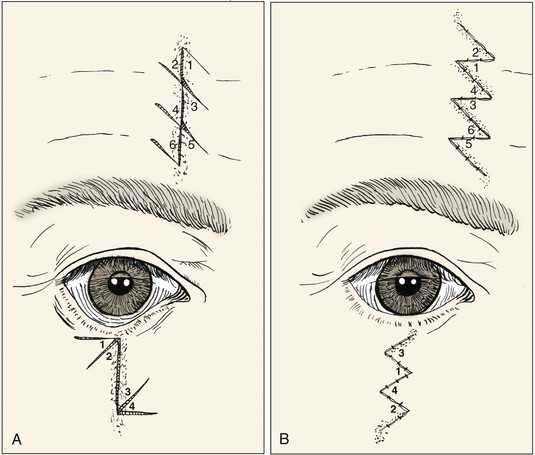
FIGURE 14-15 Multiple Z-plasties used to improve camouflage of vertical forehead scar and to correct contracted lower eyelid and cheek scar.
Z-plasties may be designed with unequal angles. The more acutely angulated flap is transposed in a greater arc than the larger angled flap. Variations on such unequal Z-plasties can be used to treat asymmetric facial features. An example is when a scar contracture distorts the oral commissure (Fig. 14-17). In such cases, the larger flap consisting of the commissure is undermined only a limited degree and the smaller flap is transposed into the tissue void created by release of the contracted commissure. This facilitates transfer of the oral commissure to a more natural position.
Summary
Z-plasty is one of the oldest concepts in plastic surgery and remains a prevalent and important technique. An understanding of its geometric principles is critical to its successful application. Z-plasty is a double transposition flap technique that is used to lengthen contracted scars, to change the orientation of scars for better alignment with RSTLs, or to interrupt straight scars for better camouflage. Z-plasty is also helpful in the repair of some cutaneous defects and for realignment of malpositioned facial structures. Classic indications for Z-plasty include realignment of scars that are not parallel to RSTLs, correction of scars that cause contracted webbing of the neck, repositioning of an oral commissure or eyelid that is malpositioned from scarring, and correction of congenital or post-traumatic epicanthal folds.12,13 Z-plasty is also helpful in the repair of a primary cleft palate.14,15 It is impossible to list all of the reported uses of Z-plasty described in the literature. Suffice to say that with a thorough understanding of its principles, Z-plasty is an extremely powerful tool in the reconstructive surgeon’s armamentarium.
Case Reports
Case 1
The vertical, mature, widened and thickened tracheotomy scar shown in Figure 14-18A is ideal for scar revision by Z-plasty. A 60° Z-plasty was planned and marked with use of a caliper for precise measurement and alignment. The central limb of the Z-plasty consisted of the thickened scar. A 60° Z-plasty was used to reposition the vertically oriented scar 90° so it would lie in RSTLs. In the anterior neck, RSTLs are horizontally oriented as demonstrated by the curvilinear dotted line bisecting the scar in Figure 14-18B. The circle marked with a dotted line in Figure 14-18C represents the extent of subcutaneous undermining of the skin required for transposition of the Z-plasty flaps. Note the horizontal alignment of the central limb (original scar) after transposition of the flaps (Fig. 14-18D). The final result is shown 1 year postoperatively in Figure 14-18E.
Case 2
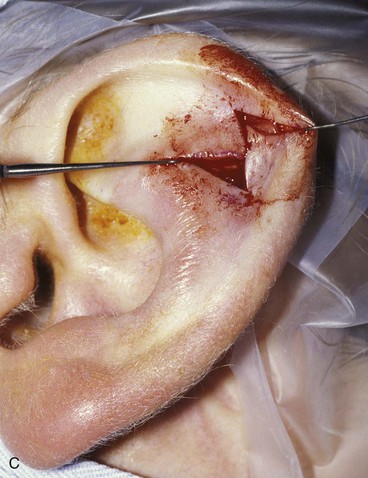
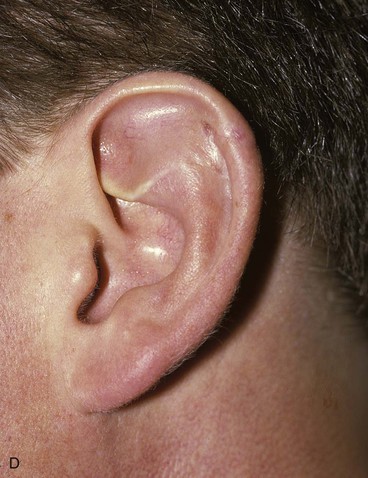
A patient presented with a contracted scar disrupting the contour of the concavity of the scapha of the left ear (Fig. 14-19A). Z-plasty was an ideal solution to this problem because the technique offered a method of improving the contracture and eliminating the web of scar that was deforming the concave contour of the scapha. Figure 14-19B shows the planned incision. Note the orientation of the peripheral limbs of the Z-plasty, which are aligned with the vertical axis of the concavity of the scapha. The mirror image of this planned Z-plasty would be less desirable because the peripheral limbs would conform less optimally to the vertically oriented surrounding ear structures. Figure 14-19C shows the flaps incised and transposed. Note the horizontal release of the scar contracture. The result 1 year after surgery was satisfactory (Fig. 14-19D).
Case 3
Figure 14-20A shows a patient with an oblique forehead scar extending through the medial aspect of the right eyebrow and into the right upper eyelid. Revision surgery to improve camouflage of the forehead component of this scar required excision of the existing widened scar tissue and realignment of the oblique portions of the scar in an axis more parallel to the horizontal RSTLs of the forehead. An example of this technique is illustrated in Figure 14-15. Figure 14-20B demonstrates the planned excision of the forehead scar and two Z-plasties designed. The irregular line drawn on the right side of the patient’s forehead represents the anticipated final appearance of the suture line after scar excision and completion of the two Z-plasties. The anticipated appearance of the suture line closely resembles the true incision line after transposition of the Z-plasty flaps (Fig. 14-20C). The outcome 1 year postoperatively showed an improvement of scar camouflage (Fig. 14-20D).
Case 4
A patient presented with a contracted lateral neck scar that limited movement of the head and neck (Fig. 14-21A). A single large Z-plasty might have been effective in releasing the contraction, but it was elected to use two Z-plasties designed similar to the three Z-plasties illustrated in Figure 14-14C, D. The two options for design of the Z-plasties were drawn on the neck skin (Fig. 14-21B). The design on the right was selected, although either option would have been appropriate in this case. The flaps were elevated, followed by resection of the dense subcutaneous scar band marked in purple in Figure 14-21C. After resection of the scar and completion of the double Z-plasty, the contraction was released, creating a more natural contour of the lateral neck (Fig. 14-21D, E). The Z-plasties were successful in releasing the contracted scar (Fig. 14-21F).



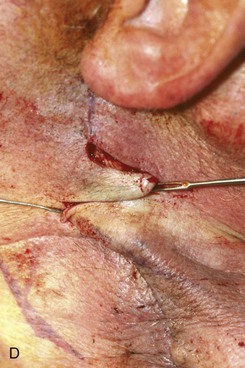

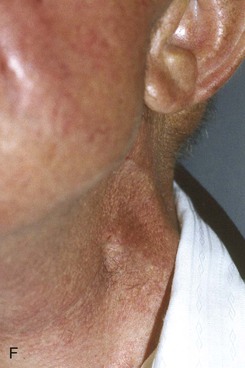
FIGURE 14-21 A, Contracted vertical neck scar selected for double Z-plasty scar revision. B, Two alternative designs for Z-plasty. Design on right was selected. C, Superior Z-plasty flaps retracted to expose underlying scar marked in purple, which was removed to facilitate release of contracture. D, Superior Z-plasty flaps transposed. E, Inferior Z-plasty flaps transposed and wound repaired. F, Postoperative view at 6 months.
Case 5
The patient shown in Figure 14-22 underwent cleft lip repair as an infant. She presented with concerns about her lip deformity. Examination of the lip revealed a contracted depressed scar and notching of the vermilion border (Fig. 14-22A). A Z-plasty was designed (Fig. 14-22B) with the intention of inferiorly transposing the vermilion border lateral to the scar. The second flap of the Z-plasty was designed to superiorly transpose the skin of the lip medial to the scar to better align the border of the vermilion. The small notch in the wet line of the vermilion was corrected by direct excision and reapproximation of the vermilion muscle. The Z-plasty and orbicularis muscle realignment within the substance of the vermilion were successful in improving the appearance of the lip (Fig. 14-22C).
Case 6
The man shown in Figure 14-23A sustained a gunshot wound causing damage to the cheek, lip, and maxilla. He presented with a long, wide scar. There was a trap-door deformity involving the portion of the scar on the upper lip. A scar revision with Z-plasty was planned to interrupt the linearity of the scar and to reposition a portion of the scar in the nasofacial sulcus (Fig. 14-23B, C). Figure 14-23D shows improvement in the appearance of the scar 6 months postoperatively.
Case 7
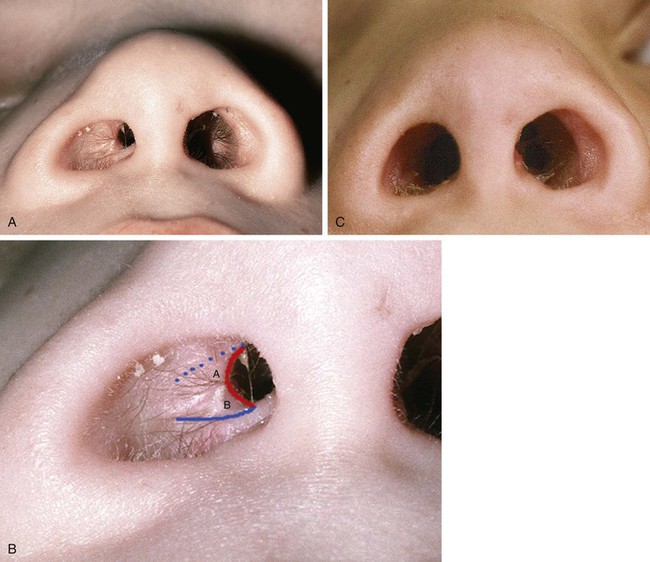
An 8-year-old child underwent a combined craniofacial approach, including facial degloving, to remove a large maxillary, orbital, and skull base tumor. This resulted in a significant stenosis of the anterior aspect of the right nasal airway (Fig. 14-24A). The constricted nasal vestibule was caused by a contracted web of scar extending from the inferolateral nasal wall to the apex of the vestibule. For correction of the deformity, it was necessary to remove scar tissue and to eliminate the web. Accordingly, a three-dimensional Z-plasty was designed, as marked in Figure 14-24B. The flap labeled A, designed on the posterior aspect of the stenotic scar, was interchanged with the flap labeled B, marked on the anterior aspect of the stenotic scar. The vertically oriented scar web was made the central limb of the Z-plasty to lengthen this dimension after transposition of the Z-plasty flaps. It was necessary to excise scar tissue deep to the flaps. The postoperative result at 4 months is shown in Figure 14-24C.
Case 8
A patient presented with a torn right earlobe, or cleft, after ear piercing (Fig. 14-25A, B). A three-dimensional Z-plasty was designed for repair with the central limb positioned along the skin covering the interior of the cleft. The cleft scar and the skin covering the scar were excised, and the triangular flaps of the Z-plasty were transposed (Fig. 14-25C). Figure 14-25D shows the wound closure. Note that the central limb of the designed Z-plasty was oriented perpendicular to the inferior margin of the earlobe to minimize notching once the Z-plasty flaps were transposed. The 4-month postoperative result is shown in Figure 14-25E.
Case 9
A 3-year-old boy presented with bilateral congenital macrostomia (Fig. 14-26A). To reduce the size of the oral stoma and to close the lateral clefts of skin, mucosa, and soft tissue at the oral commissures, the borders of the clefts were excised to create a fresh wound. The mucosa and muscle layers of the clefts were approximated to reduce the horizontal width of the mouth. Repair of the skin wounds in a straight-line closure would have created scars perpendicular to the melolabial creases. To better align the skin closure line, Z-plasties of the skin wound were designed (Fig. 14-26B). The Z-plasties facilitated the creation of scars of the cheek skin that paralleled RSTLs (Fig. 14-26C, D).
Case 10
After trauma, a patient developed substantial loss of soft tissue of the left oral commissure and upper lip. Scar contracture and tethering of the lower lip due to scarring across the inferior labial sulcus also occurred (Fig. 14-27A). The patient underwent three scar revision surgical procedures, each of which used Z-plasties as part of the surgical approach. The first surgical stage consisted of a left commissuroplasty to lateralize the deformed commissure. The cheek skin was incised laterally to the desirable position for the new commissure, which is marked with an asterisk in Figure 14-27B. Scar tissue was removed and a Z-plasty was designed to transpose mucosa from the inner aspect of the left upper lip to the superior area of the constructed commissure. Flap A was interchanged with flap B, providing a mucosal lining for the commissure. An identical procedure was also performed on the lower lip, harvesting mucosa from the inner aspect of the lower lip and transferring it in the form of a Z-plasty to the inferior aspect of the oral commissure. Six months postoperatively, the patient had a reasonable restoration of the left commissure (Fig. 14-27C).




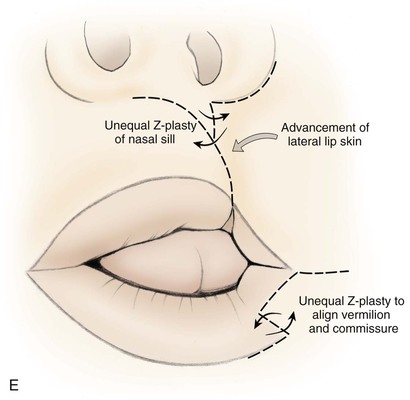



FIGURE 14-27 A, Upper and lower lip tissue deficiencies after gunshot wound. B, First-stage commissuroplasty. After horizontal lateral skin incision to site of planned new commissure (*), upper lip mucosal Z-plasty was used to transfer flap A to lateralized commissure. C, Six months after first stage. D, Second-stage scar revision. Z-plasty at superior limit of upper lip scar and advancement of lateral lip skin medially. Z-plasty designed to correct distorted vermilion of lower lip. E, Illustration demonstrating second stage. F, Second stage completed and wounds closed. Note improvement in position of lower lip vermilion border and commissure. G, Third stage. Z-plasty of upper and lower lip scars. H, One year after third stage.
The patient continued to have a foreshortened upper lip, disruption of the vermilion border of the lower lip, and trap-door deformity of the lower lip scar. A second surgical procedure was planned in which a Z-plasty was used to correct a depressed scar below the nasal sill. The entire vertical scar of the upper lip was excised, and the lip skin lateral to the scar was advanced medially to increase the availability of skin in the area of the resected scar. A Z-plasty was also performed on the lower lip in an effort to correct distortion of the left commissure (Fig. 14-27D, E). Figure 14-27F shows the suture line immediately after the second surgical stage. Note the improved alignment of the left commissure and vermilion of the lower lip as a result of the Z-plasty.
Six months after the second surgical stage, it was evident that there was a persistent contracted vertical scar of the upper lip causing distortion of the vermilion border. A third surgical procedure was performed to correct the contracted upper lip scar and to treat the trap-door deformity of the lower lip scar that had not been addressed by the previous two procedures. The third surgical stage consisted of two Z-plasties of the upper lip scar and a single Z-plasty of the inferior aspect of the lower lip scar. The lower lip Z-plasty disrupted the curvilinear scar that was the primary cause of the trap-door deformity. The large Z-plasty at the superior aspect of the upper lip scar served to lengthen the contracted scar and better align the vermilion border. A second smaller Z-plasty designed in the scar line at the vermilion border of the upper lip served to improve the continuity of the vermilion (Fig. 14-27G). The final outcome 1 year postoperatively is shown in Figure 14-27H. Z-plasties performed in three separate surgical procedures were instrumental in lengthening the upper lip scar, correcting the trap-door deformity of the lower lip scar, and realigning the vermilion borders of both lips.
Case 11
Figure 14-28A shows a patient with an incomplete cleft palate who underwent double opposing Z-plasty palatoplasty (Furlow palatoplasty) repair. This technique was first described by Furlow in 198616 and has been widely used for repair of the soft palate and reconstruction of the levator sling. In patients with cleft palate deformity, the soft tissue musculature may be hypoplastic and has abnormal orientation and insertion into the posterior hard palate. Capitalizing on Z-plasty principles, the Furlow palatoplasty technique allows transverse reorientation of the musculature for reconstruction of the levator sling. In addition, this allows lengthening of the palate in cases of velopharyngeal insufficiency associated with submucous cleft palate.
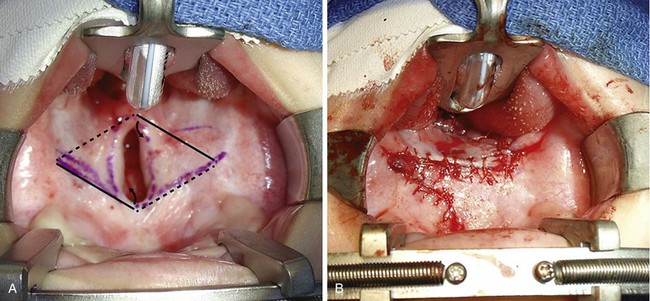
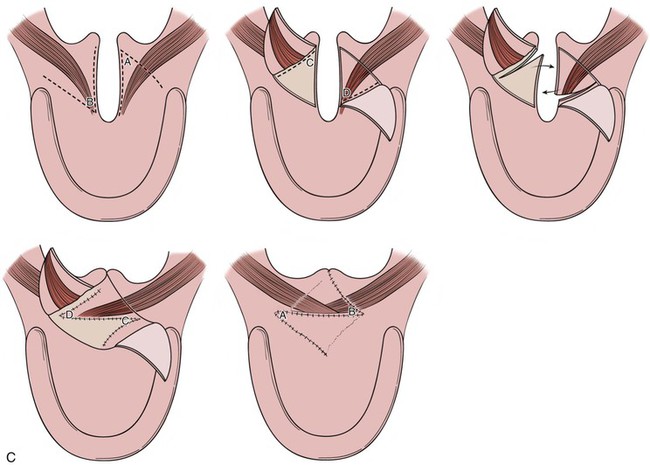
FIGURE 14-28 A, Incomplete cleft palate. Solid lines indicate incisions for oral flaps and dashed lines indicate nasal mucosal incisions. Curved arrows show direction of oral flap elevation. B, Immediate postoperative result after completed Furlow palatoplasty repair. C, Sequence of illustrations outlining the steps in double opposing Z-plasty repair of a cleft palate (Furlow palatoplasty).
Two opposing Z-plasties were designed on the soft palate as mirror images of each other. Although the elevation of flaps may vary on the basis of the dominant hand of the surgeon, the palatal musculature is always elevated as part of the posteriorly based myomucosal flap (with the oral or nasal mucosa attached). In this case, the left posteriorly based oral flap was elevated as a myomucosal flap, and the right anteriorly based oral flap was elevated with mucosa only. After elevation of the two oral side flaps, the nasal flaps were incised and elevated. The two myomucosal flaps were transposed posteriorly; the two mucosal flaps were transposed anteriorly. The immediate postoperative result is shown in Figure 14-28B.
References
1. Borges, AF. Z-plasty. In: Borges AF, ed. Elective incisions and scar revision. Boston: Little Brown, 1973.
2. Davis, WE, Renner, GJ. Z-plasty. In: Thomas JR, Holt GR, eds. Scar revision. St. Louis: Mosby–Year Book, 1989.
3. Berger, P. Autoplastie par dédoublement de la palmure et échange de lambeaux. In: Berger P, Banzat S, eds. Chirurgie orthopédique. Paris: G Steinheil, 1904.
4. Fricke, JC. Bildung neuer Augenlider (Blepharoplastik): nach Zerstörung und dadurch hervorgebrachten Auswärtswendungen derselben. Hamburg: Perthes & Basse; 1829.
5. Horner, WE. Clinical report on the surgical department of the Philadelphia Hospital. Am J Med Sci. 1837; 21:99.
6. Serre, M. Traité sur l’art de restaurer les difformités de la face: selon la méthode par déplacement, ou méthode française. Montpellier, France: L Castel; 1842.
7. Denonvilliers, CP. Blepharoplasie. Bull Soc Chir. 1856; 7:213.
8. McCarthy, JG. Introduction to plastic surgery. In: McCarthy JG, ed. Plastic surgery, vol 1, General principles. Philadelphia: WB Saunders, 1990.
9. Limberg, AA. Design of local flaps. In: Gibson T, ed. Modern trends in plastic surgery. London: Butterworth, 1966.
10. Jankauskas, A, Cohen, IK, Grabb, WC. Basic technique of plastic surgery. In: Grabb WC, Aston SJ, eds. Plastic surgery. Boston: Little Brown, 1991.
11. Davis, JS, Kitlowsky, EA. The theory and practical use of the Z-incision for the relief of scar constriction. Ann Surg. 1939; 109:1001.
12. Furnas, DW, Fischer, GW. The Z-plasty: biomechanics and mathematics. Br J Plast Surg. 1971; 24:144.
13. Converse, JM, Smith, B. Naso-orbital fractures and traumatic deformities of the medial canthus. Plast Reconstr Surg. 1966; 38:156.
14. Walike, J, Larrabee, WF. Repair of the cleft earlobe. Laryngoscope. 1985; 95:876.
15. Frodel, JL. Z-plasty. Facial Plast Surg Clin North Am. 1998; 6:149.
16. Furlow, LT. Cleft palate repair by double opposing Z-plasty. Plastic Reconstr Surg. 1986; 78:6.