CHAPTER 22 Wrist blocks
Clinical anatomy
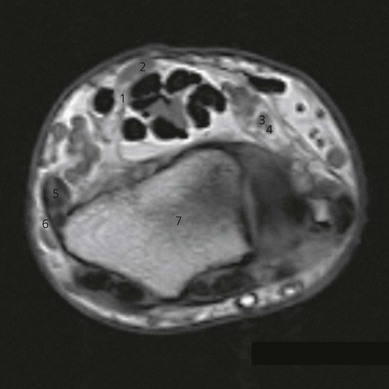
The hand is innervated by the three nerves that pass through the wrist (Fig. 22.1).
The median nerve approaches the wrist between the palmaris longus (if present) and the flexor carpi radialis. It can also lie beneath the palmaris longus (Fig. 22.2). The median nerve provides sensation to the lateral half of the palm, flexor aspect of the thumb, index finger, middle finger, and radial side of the ring finger.
The ulnar nerve, in the middle of the forearm between the flexor digitorum profundus and the flexor carpi ulnaris, gives off a dorsal and a ventral cutaneous branch. At the wrist, the ulnar nerve lies between the ulnar artery and the lateral border of the flexor carpi ulnaris (Fig. 22.2), which inserts on the pisiform bone. Near the pisiform bone, it passes superficial to the flexor retinaculum and ends by dividing into superficial and deep branches. The ulnar nerve provides sensation for the ulnar half of the back and front of the hand, little finger, and ulnar side of the ring finger.
The radial nerve at the wrist lies between the flexor carpi radialis and the radial artery (Fig. 22.3). The radial nerve provides sensation for the radial half of the dorsum of the hand, back of the thumb, and part of the dorsum of the index finger.
Surface anatomy
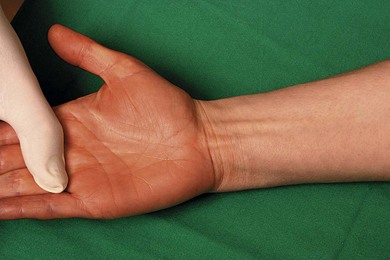
Bony landmarks include the ulnar styloid and the radial styloid carpal bones. Other landmarks include the wrist crease, flexor carpi radialis, palmaris longus, and flexor carpi ulnaris tendons (Fig. 22.4). These tendons can be accentuated by having the patient flex the wrist while making a fist. The radial artery can be palpated lateral to the tendon of the flexor carpi radialis, and the ulnar artery lateral to the flexor carpi ulnaris tendon.
Sonoanatomy
The examination begins with the patient supine, the arm abducted, the forearm and wrist in supination (Fig. 22.5). A systematic survey should be performed from superficial to deep and medial to lateral. A high frequency ultrasound transducer is used with a transverse orientation.
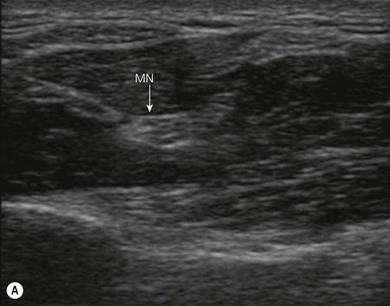
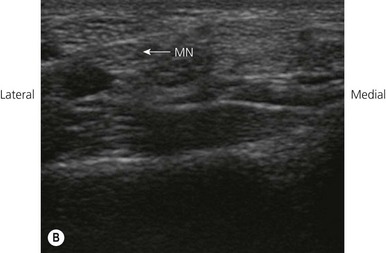
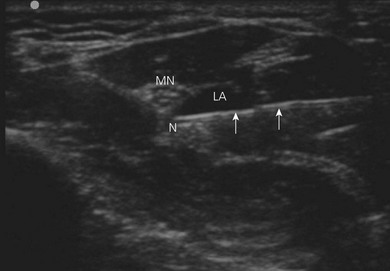
The median nerve passes distally in the volar aspect of the forearm between the flexor digitorum superficialis and the flexor digitorum profundus muscles (Fig. 22.6A). Approximately 5 cm proximal to the flexor retinaculum, the median nerve courses around the radial or lateral edge of the flexor digitorum superficialis, where its position becomes more superficial. Just proximal to the carpus, the nerve lies between the tendons of the flexor digitorum superficialis and the flexor carpi radialis, partially deep to the tendon of palmaris longus (if it is present; Fig. 22.6B). The nerve then passes deep to the flexor retinaculum into the carpal tunnel of the wrist.
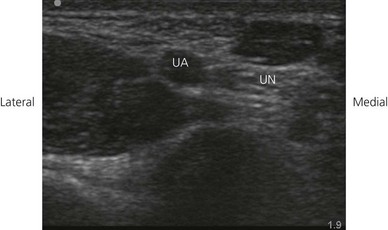
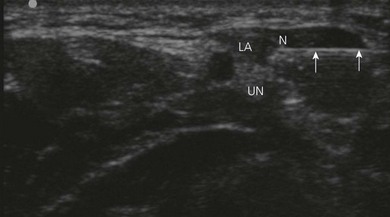
The ulnar nerve at the wrist lies within the Guyon canal, an oblique fibro-osseous tunnel, formed by the flexor retinaculum and palmar carpal ligaments, that lies within the proximal part of the hypothenar eminence. The canal contains the ulnar nerve, the ulnar artery with its venae comitantes, and loose fibrofatty tissue. On transverse sonograms, the ulnar nerve appears as a rounded structure with a location medial to the artery (Fig. 22.7).
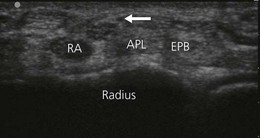
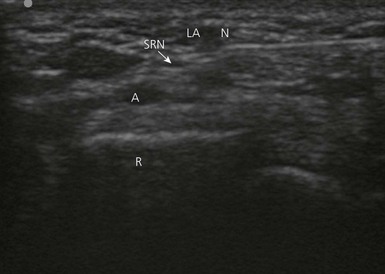
Keeping the patient’s wrist halfway between pronation and supination, place the ultrasound transducer over the lateral aspect of the radial styloid to examine the first compartment of the extensor tendons – abductor pollicis longus (ventral) and extensor pollicis brevis (dorsal). Look at the radial artery and the sensory branch of the radial nerve, the first encroaching deep, the second superficial to the first compartment (Fig. 22.8). Scanning from proximal to distal, note the radial nerve and its branches snapping from ventral to dorsal over these tendons.
Technique
Landmark-based approach
Median nerve block
Needle insertion for median nerve block is 2 cm cephalad from the wrist crease between the tendons of the flexor carpi radialis and palmaris longus, if present (Fig. 22.9). The needle and syringe are held like a pencil between the thumb and index fingers, with a cephalad needle orientation.
Ulnar nerve block
Needle insertion for ulnar nerve block is 2 cm cephalad from the wrist crease lateral to the flexor carpi ulnaris or medial to the artery. For ulnar nerve block, ventral and medial approaches can be used. The needle and syringe are held like a pencil between the thumb and index fingers; needle orientation is cephalad for the ventral approach (Fig. 22.10).
The patient is instructed to indicate when they feel a paresthesia in the palm and fingers. On obtaining a paresthesia, the needle is withdrawn slightly. Absence of paresthesia is checked prior to injecting 3 mL of local anesthetic. The ulnar nerve at the wrist may also be blocked by injection medial and deep to flexor carpi ulnaris (Fig. 22.11). The medial approach is preferable because ulnar artery damage is less likely, and both dorsal and palmar cutaneous branches may be blocked from the same needle insertion point.
Radial nerve block
Needle insertion for radial nerve block is at the level of the wrist crease (Fig. 22.12). For radial nerve block at the wrist, a 30-mm 22-G needle is used. A subcutaneous injection is made from the radial styloid across the tendon of the extensor pollicis brevis to the middle of the dorsal surface of the wrist (Fig. 22.13). The needle is redirected, infiltrating now across the tendon of the extensor pollicis brevis to the ventral surface of the wrist and over the radial artery. A paresthesia is not sought because the radial nerve is now superficial fibers only. Local anesthetic solution is massaged in to improve the subcutaneous spread. Local anesthetic (8–10 mL) is injected.
Ultrasound-guided approach
Intravenous access, electrocardiogram (ECG), pulse oximetry and blood pressure monitoring are established. Maximized comfort for the operator and patient is an important step in pre-procedure preparation. For ultrasound-guided nerve blocks at the wrist, the patient is placed in the supine position, the arm abducted, the forearm and wrist in supination (Fig. 21.5). The operator sits adjacent to the side to be blocked. The ultrasound screen, transducer, needle, and plane of imaging should all be placed in one view for the operator. For ultrasound-guided nerve blocks at the wrist the ultrasound screen is placed at the elbow level on the side to be blocked (Fig. 22.14). Room lights may be turned down to enhance image viewing. The operating lights can be used to maintain some working lighting in the background.
The median nerve is identified just proximal to the wrist crease. A 15-mm 25-G needle is inserted parallel to the axis of the beam of the ultrasound transducer (Fig. 22.15). The needle is slowly advanced under ‘real-time’ imaging to bring the needle tip to rest adjacent to the median nerve. The needle is readjusted to allow complete encirclement of the nerve with local anesthetic (5 mL). Local anesthetic appears as a hypoechoic image (Fig. 22.16).
The ulnar nerve is identified adjacent to the pisiform bone in the wrist. A 15-mm 25-G needle is inserted parallel to the axis of the beam of the ultrasound transducer (Fig. 22.17). The needle is slowly advanced under ‘real-time’ imaging to bring the needle tip to rest adjacent to the ulnar nerve. The needle is readjusted to allow complete encirclement of the nerve with local anesthetic (5 mL). Local anesthetic appears as a hypoechoic image (Fig 22.18).
Branches of the superficial radial nerve are identified in the subcutaneous tissue in proximity to the radial artery at the wrist. A 15-mm 25-G needle is inserted parallel to the axis of the beam of the ultrasound transducer (Fig 22.19). The needle is slowly advanced under ‘real-time’ imaging to bring the needle tip to rest adjacent to the nerve. Local anesthetic appears as a hypoechoic image (Fig. 22.20).
Adverse effects
Clinical pearls
Gebhard RE, Al-Samsam T, Greger J, et al. Distal nerve blocks at the wrist for outpatient carpal tunnel surgery offer intraoperative cardiovascular stability and reduce discharge time. Anesth Analg. 2002;95:351-355.
Klezl Z, Krejca M, Simcik J. Role of sensory innervation variations for wrist block anesthesia. Arch Med Res. 2001;32:155-158.
Loewy J. Sonoanatomy of the median, ulnar and radial nerves. Can Assoc Radiol J. 2002;53(1):33-38.
Macaire P, Singelyn F, Narchi P, Paqueron X. Ultrasound- or nerve stimulation-guided wrist blocks for carpal tunnel release: a randomized prospective comparative study. Reg Anesth Pain Med. 2008;33(4):363-368.
Thompson WL, Malchow RJ. Peripheral nerve blocks and anesthesia of the hand. Mil Med. 2002;167:478-482.