CHAPTER 19 Wrist Arthroscopy: Setup, Anatomy, and Portals
Wrist arthroscopy has been used since it was first described by Chen in 1979.1 In the early stages of development, it provided only partial evaluation of the articular surfaces, and it was not used therapeutically. Few investigators routinely used arthroscopic techniques.2 It was not until 1986, when Whipple advocated distraction techniques and precise portal placement, that the exposure necessary to perform an extensive evaluation of the wrist joint became an option.3 Even then, diagnosis was the primary function, and therapeutic indications were minimal. Since that time, innovations in wrist arthroscopy have expanded treatment indications and promoted widespread acceptance.
Diagnostic and operative forms of arthroscopy have advanced our understanding of wrist anatomy and function, and arthroscopic techniques have facilitated the repair of previously unrecognized pathology. Continued advances in instrumentation and technology will improve the ability to perform challenging and innovative procedures as the principles of open surgical procedures become adapted to arthroscopy.4
Wrist arthroscopy allows close visual examination of the carpal articular surfaces and wrist ligaments, which is often inadequate with open procedures and which can be performed in a less invasive manner than traditional arthrotomy.5 The extremely close evaluation of details provides many benefits and increases appreciation of the subtle differences between normal and pathologic anatomy.6 This fact alone underscores the importance of a thorough understanding of arthroscopic anatomy.
ANATOMY
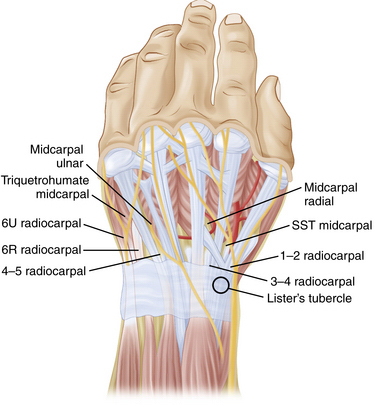
The wrist is made up of the eight carpal bones, each with multiple articular surfaces and the intrinsic and extrinsic ligaments, and a triangular fibrocartilage complex (TFCC) that is surrounded by tendons and neurovascular structures (Fig. 19-1).7,8 A thorough understanding of the relationship between the surface anatomy of the wrist and these underlying structures is essential to perform accurate arthroscopic portal placement and adequate arthroscopy. Understanding these relationships helps to prevent injury to the cutaneous nerves, tendons, and vascular structures and can minimize the risk to the articular surfaces in the wrist. It also facilitates the use of instruments during procedures, enabling the completion of increasingly complicated arthroscopic wrist procedures.
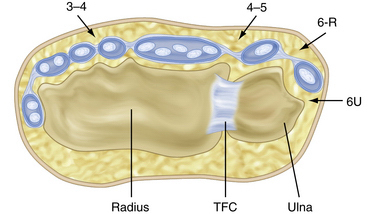
FIGURE 19-1 Cross-sectional anatomy of the dorsal compartments.
(Modified from Geissler WB, Freeland AE, Weiss AP, Chow JC. Techniques of wrist arthroscopy. Instr Course Lect. 2000:49:225-237.)
The extensor retinaculum is an obliquely oriented structure that spans the dorsal distal radius and ulna. It overlies the 12 extensor tendons, which are partitioned into six compartments to prevent bowstringing of the extensor tendons.4 The extensor pollicis longus (EPL) is the only tendon in the third compartment, and it is easily palpated, especially after application of traction. This structure passes just ulnar to Lister’s tubercle and should be appropriately marked. The area bordered by the EPL and extensor pollicis brevis together and the extensor carpi radialis longus (ECRL) define the margins of the anatomic snuffbox. The extensor digitorum communis (EDC) is just ulnar to the EPL. The extensor carpi ulnaris (ECU) and the ECRL and ECRB tendons are easily palpated and should be marked. The intersection of these tendons and the bony structures allows accurate identification and precise placement arthroscopy portals (Fig. 19-2).
PATIENT EVALUATION
History and Physical Examination
A thorough history and physical examination are essential before proceeding with arthroscopic evaluation of the wrist. It has been said that if no diagnosis can be made after a thorough clinical assessment, little additional information can be obtained from arthoscopy.9 A meticulous history helps focus the examiner on the cause and directs the physical examination to the suspected pathology. The examiner must determine the activities that exacerbate or lessen the problem, the functional loss, and the ability of the patient to perform daily activities, including work and leisure activities. The mechanism of injury should be ascertained.
Physical examination is the most accurate method for diagnosing pathology.2 A systematic approach to the wrist examination is essential. All joints must be carefully inspected, palpated, and appropriately stressed with the use of provocative tests. Areas of swelling, tenderness, or pain can focus attention on the specific pathology. Examination includes palpation of the tendons and evaluation of the patient’s neurologic and vascular status.
Diagnostic Imaging
Occasionally, the diagnosis remains unclear after an adequate history, physical examination, and routine radiographic studies have been completed. Further diagnostic studies may be indicated. Computed tomography (CT) is useful for evaluating osseous and articular morphology. Magnetic resonance imaging (MRI) provides important information about the soft tissues of the wrist and the vascularity of bones. The most definitive study is magnetic resonance arthrography, which begins with a radiocarpal injection followed by a distal radioulnar joint injection.10
TREATMENT
Indications and Contraindications
Wrist arthroscopy provides an accurate complement to the probable diagnosis obtained from the physical examination. Arthroscopy is useful for evaluation of patients with wrist pain and motion loss when noninvasive studies have failed to provide a diagnosis, and it is more sensitive than arthrography for evaluating pathology.8 Diagnosis of interosseous ligaments tears and the degree of carpal instability can be accurately determined using arthroscopy. It is also useful in patients with well-defined pathology, such as nonunions, Kienbock’s disease, and scapholunate or lunotriquetral dissociations, for which evaluation of the articular surfaces is of prognostic and therapeutic importance.
Although once used almost exclusively for diagnostic purposes, the therapeutic indications for wrist arthroscopy continue to expand. Arthroscopic treatment is indicated for loose body removal, synovectomy, intra-articular adhesion release, lavage of a septic wrist, débridement of chondral lesions, hypertrophic or torn ligaments, and tears of the TFCC. It has also been used for dorsal ganglion excision and provides a useful adjunct in the reduction of distal radius and scaphoid fractures. Bone excision procedures, such as radial styloidectomy and partial resection of the distal ulna (i.e., wafer procedures), have been performed arthroscopically. Arthroscopy has been described for advanced procedures, such as proximal row carpectomy, excision of the proximal pole of the scaphoid, lunate excision in Kienbock’s disease, and capitolunate arthrodesis.7,8
Conservative Management
Before arthroscopy, nonoperative measures should usually be exhausted. Temporary immobilization and anti-inflammatory medication may be helpful. Diagnostic and therapeutic injections frequently provide some benefit. A physical therapy regimen for wrist range of motion and strengthening may prove definitive for some wrist pathology.
Arthroscopic Technique
Setup
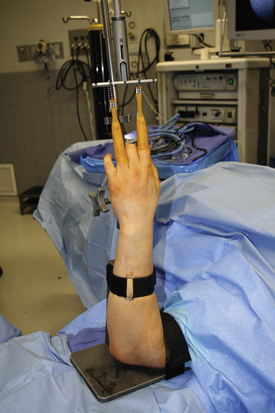
A significant improvement in wrist arthroscopy came with the innovation of wrist distraction. This key element enhanced the surgeon’s ability to perform arthroscopic procedures in the confined wrist joint. Distraction is essential to improve visualization and provide adequate space for maneuverability during wrist arthroscopy, because distention of the joint alone does not provide adequate room for instrumentation.2 Several options exist to provide the necessary distraction. A dedicated sterile or nonsterile traction tower is a popular choice. Alternatives include the use of horizontal traction with a pulley and weight system and a nonsterile traction boom device (Figs. 19-3 to 19-5).
We prefer a sterile traction tower with nylon finger traps. It provides convenient application of wrist distraction in flexion, extension, and radial and ulnar deviation. This system allows adjustability to the distraction force and the position of the wrist, and it permits easy conversion to open procedures if necessary. The traction tower system maintains the wrist in a stable position for portal preservation during the exchange of instruments.2
The arm is placed in an abducted position, and the upper arm is secured to the traction tower. A nonsterile tourniquet is applied, and the arm and hand are prepared and draped with the forearm in a vertical position (Fig. 19-6). We use sterile soft nylon finger traps to secure the index and long finger to the tower for most procedures. Soft traps increase the surface area and distribute the force better than wire devices. For patients with poor or fragile skin, additional fingers in the traps can decrease the force to the skin.2 To improve visualization for ulnar-sided pathology, we frequently use the index and ring fingers (Fig. 19-7). Most procedures require 5 to 10 pounds of traction.
Equipment
Other small joint arthroscopy equipment is available and necessary for mastery of wrist arthroscopy. Equipment includes a small joint shaver (2.7 or 2.9 mm) with multiple tips, a wrist probe (1.7 or 2.0 mm), and many of the smaller versions of large joint arthroscopic instruments.5,7 As arthroscopy has advanced, more specialized equipment has become available, including TFCC repair kits, retrograde retrievers, ablation shrinkage devices, and fracture fixation devices. Spinal needles and passing sutures are helpful tools that have been adapted from other arthroscopic repair techniques.
Clear physiologic crystalloid solution, such as lactated Ringer’s solution, is preferable because it can be rapidly absorbed into the tissues and can prevent overdistention. Irrigant can be introduced through the sheath of the arthroscope or by separate inflow and outflow portals. Gravity inflow has proved adequate in our practice. Pinch chambers can introduce small boluses of irrigant to clear the visual field.2 Fluid pumps that can precisely control the pressure in the joint are available. However, pressurized injection increases the risk of fluid extravasation into subcutaneous tissue and is usually unnecessary.
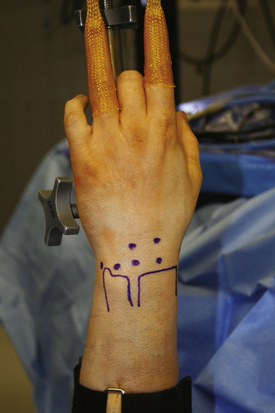
Portals
Precise portal placement is essential for performing a complete wrist arthroscopy and for minimizing iatrogenic injury to the wrist joint and surrounding structures. Placing the portals in an incorrect manner can result in damage to neurovascular structures and the articular cartilage. All portals and surface landmarks should be marked on the skin. Marking portals after the application of traction helps to prevent distortion and improperly placed portal sites (Fig. 19-8).
Radiocarpal Portals.
Radiocarpal portals include the 3-4, 4-5, 6-R, 6-U, and 1-2 portals. Radiocarpal portals show smooth carpal articulations, whereas the midcarpal portals show more irregular articulations.5 Portals are named according to the interspace between extensor compartments. The 3-4 portal divides the third and fourth extensor compartments. The 6-R and 6-U portals are named by their relationship to the ECU, with the 6-R on the radial aspect and the 6-U on the ulnar aspect.7 Palpation between these compartments demonstrates soft spots of the wrist, which provide the least traumatic entry points into the joint.
The 3-4 Portal.
The 3-4 portal is usually the first portal established, and it is the primary viewing portal. It is bordered on the radial side by the EPL and ECRB, on the ulnar side by the EDC, on the proximal side by the distal radius, and on the distal side by the scapholunate ligament. The 3-4 portal is established 1 cm distal to Lister’s tubercle, and it is located by palpating the distal edge of the radius between the ulnar border of the ECRB and the radial margin of the EDC in line with the radial border of the long finger. This is the soft spot between the third and fourth compartments.7 A spinal needle is then inserted parallel to the radial articular surface at about 10 degrees, matching the palmar tilt (Fig. 19-9).
This portal is the workhorse of standard wrist arthroscopy and provides a broad view of most of the radiocarpal joint on the volar side. The portal is relatively safe, with the sensory branch of the radial nerve (SBRN) a mean distance of 16 mm and a mean distance from the radial artery of 26.3 mm.11
The 4-5 Portal.
The 4-5 portal is bordered on the radial side by EDC, on the ulnar side by the extensor digiti quinti (EDQ), proximally by the attachment of the radius and the TFCC, and distally by the lunate. It is established 1 cm ulnar and slightly more proximal to the 3-4 portal because of the inclination of the radius.7 It can be found by palpating the soft spot directly ulnar to the EDC. A spinal needle should then be placed just proximal to the lunate. Entry through this portal places instruments directly adjacent to the midportion of the TFCC.12 The 4-5 portal is typically the main working portal for instrumentation on the ulnar side of the wrist. It may also be used as a viewing portal for ulnar sided structures. This portal has minimal neurovascular risk unless there is an aberrant branch of the SBRN.11
The 6-R Portal.
Frequently used as an alternative to the 4-5 portal, the 6-R portal is bordered radially by the EDQ, ulnarly by the ECU, proximally by the TFCC, and distally by the lunotriquetral joint. It enters the wrist joint just distal to the ulnar attachment of the TFCC. This portal is found by using the proximal border of the triquetrum rather than distal ulna as a surface landmark to avoid damaging the TFCC. It is establish under arthroscopic guidance by introducing a needle just radial to the ECU. The 6-R portal is typically used for instrumentation or for outflow. It also provides visualization of the TFCC and the ulnolunate, ulnotriquetral, and interosseous lunotriquetral ligaments. The 6-R has a mean distance of 8.2 mm from the dorsal sensory branch of the ulnar nerve (DBUN).11
The 6-U Portal.
The 6-U portal is established volar to the ECU tendon, but because of its proximity to the DBUN, it is not routinely used. The skin incision may be placed as far volar as the dorsal border of the ECU tendon. The portal enters the wrist joint through the prestyloid recess between the ECU tendon and the ulnar styloid. The portal is distal to the TFCC and dorsal ulnar to the ulnotriquetral ligament. The 6-U portal is typically used for the inflow or outflow cannula. It may be used as an accessory portal for viewing ulnar-sided structures or for instrumentation during TFCC repairs. The mean distance of the portal to the DBUN is 4.5 mm, but the nerve can have multiple branches in some patients.11
The 1-2 Portal.
The 1-2 portal is not used frequently. It is established between the first and second extensor compartments 1 to 2 mm distal to the radial styloid. This portal is placed by finding the soft spot between the first extensor compartment containing the abductor pollicis longus and extensor pollicis brevis and the second compartment with the ECRL and ECRB tendons along the far ulnar part of the anatomic snuffbox. It is located just proximal to the waist of the scaphoid. The radial artery is located at the volar and radial aspect of the anatomic snuffbox. This necessitates placement of this portal as far dorsal as possible to avoid injury to the artery.12
The 1-2 portal provides access to the radial styloid, scaphoid, and articular surface of the distal radius, but it allows only a limited view of the lunate.4 There is significant risk with the placement of this portal. Two branches of the SBRN are a mean distance of 3 mm radial and 5 mm ulnar to the portal, and the radial artery is a mean distance of 3 mm radial to the portal.11
Midcarpal Portals.
Midcarpal evaluation should be done as a routine part of wrist arthroscopy. The four midcarpal portals include the midcarpal radial, midcarpal ulnar, triquetrohamate, and triscaphe portals. The most commonly used are the radial and ulnar midcarpal portals. The less common ones are the triscaphe and the triquetrohamate portals. The very limited room in the midcarpal space requires extra care when entering the joint. Once established, these portals should be maintained to minimize the difficulty in re-establishing them due to fluid extravisation.7 Normally, there is no communication between the radiocarpal and midcarpal spaces.
Evaluation of wrist instability with midcarpal arthroscopy is better than with radiocarpal arthroscopy alone. Studies show that instability of the scapholunate or lunotriquetral ligament diagnosed with radiocarpal arthroscopy was always seen on midcarpal arthroscopy, but instability seen by midcarpal arthroscopy was not always noticed when performing radiocarpal arthroscopy alone. Grading of the instability was equal to or greater than that done by midcarpal examination.13
Visualization of the scaphoid-trapezoid-trapezium (STT) joint, the midcarpal extrinsic ligaments, the capitohamate joint, and the articular surfaces of the midcarpal bones is improved with midcarpal arthroscopy. Midcarpal arthroscopy can be mastered quickly and adds little time to wrist arthroscopy. It has a low morbidity rate and should be used routinely for a thorough evaluation of the wrist.13
Midcarpal Radial Portal.
The radial midcarpal portal is the most commonly used midcarpal portal. It is bordered radially by the ECRB, ulnarly by the EDC, proximally by the scapholunate ligament, and distally by the capitate. It should be established in line with the radial border of the third metacarpal, 1 cm distal to the 3-4 portal. A soft spot may be palpated on the radial side of the proximal capitate between the base of the third metacarpal and the dorsal margin of the distal radius. The arthroscope enters between the capitate and scaphoid. This allows evaluation of the midcarpal space and the scapholunate, lunotriquetral, and STT articulations. This portal is relatively safe, with branches of the SBRN found radially at a mean distance of 15.8 mm.11
Midcarpal Ulnar Portal.
The midcarpal ulnar portal is bordered radially by the EDC, ulnarly by the EDQ, proximally by the lunotriquetral joint, and distally by the capitate hamate joint. It is in line with the center of the fourth metacarpal. As with the radial midcarpal portal, it is placed approximately 1 cm distal to the 4-5 portal and at about the same level as the radial midcarpal portal. This portal enters through capitate-hamate-triquetral-lunate interval. It is used primarily for instrumentation within the midcarpal joint. There is minimal risk when making this portal because the SBRN branches are usually remote to this portal.11
Triscaphe Portal.
The triscaphe portal (STT) is on the radial side of the midcarpal space. It is established ulnar to the EPL or radial to the abductor pollicis longus in line with the radial margin of the second metacarpal at the level of the distal pole of the scaphoid. The STT-R portal provides an additional view and access to the STT joint.14 Staying ulnar to EPL helps to avoid the radial artery. The ulnar aspect of the ECRL tendon can be used to check the location of this portal, because the EPL is quite mobile at the level of the STT joint. Care must be taken to prevent displacing the tendon radially while establishing the STT portal to protect the radial artery. The STT joint can be entered directly through this portal, and it is used primarily for instrumentation in this joint.12 Care should be taken to avoid the small terminal branches of the SBRN.
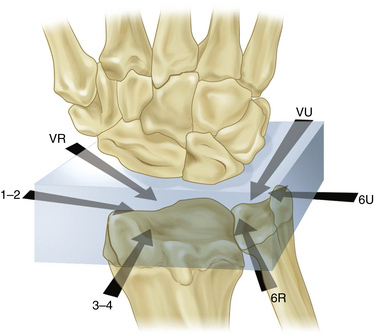
Volar Portals.
Volar portals have become increasingly popular to complete the view of diagnostic wrist arthroscopy and to provide access for procedures that are not feasible from the dorsal entry sites. Bain and colleagues suggested a box approach to wrist arthroscopy (Fig. 19-10).4 By using portals around the circumference of the wrist, visualization and access to all surfaces within the wrist are improved.15 The viewing and working portals can then be adjusted for the specific diagnostic or therapeutic procedure.4 The volar portals allow improved treatment for dorsal pathology, such as dorsal rim fractures of the distal radius, dorsal rheumatoid synovial proliferation, and volar segment tears of the scapholunate and lunotriquetral interosseous ligaments.15
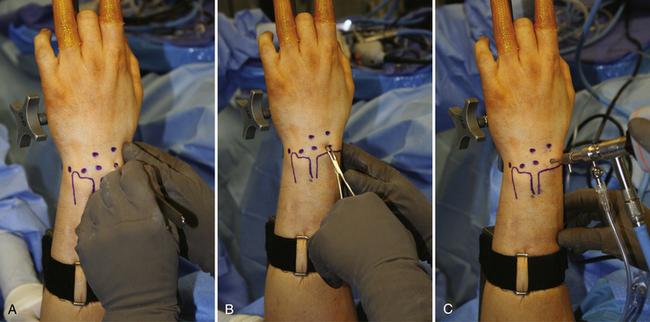
FIGURE 19-10 Box concept using dorsal and volar portals as the viewing and working portals to encircle the wrist.
(Modified from Bain GI, Munt J, Turner PC. New advances in wrist arthroscopy. Arthroscopy. 2008:24:355-367.)
Volar Radial Portal.
To place the volar radial (VR) portal, a mini-open technique is used over the flexor carpi radialis on the radial side of the volar proximal wrist crease. An anatomic study found that there was a safe zone that included the width of the flexor carpi radialis and at least 3 mm in all directions at this level from the palmar cutaneous branch of median nerve (ulnarly) and the radial artery (radially).16 Because of this safe zone, a 2-cm transverse incision can be made over the flexor carpi radialis tendon. The transverse incision provides superior cosmesis while maintaining minimal risk for the volar structures. The tendon sheath is divided, the radial artery is retracted radially, and the flexor carpi radialis and median nerve are retracted ulnarly. The radiocarpal joint is identified with a spinal needle, and the portal is opened with a blunt instrument. This portal is used to assess the dorsal aspect of the scapholunate interosseous ligament and the dorsal radiocarpal ligament.16
Volar Ulnar Portal.
Placement of the volar ulnar portal uses a mini-open technique. A 2-cm longitudinal incision is centered over the proximal wrist crease along the ulnar edge of the common flexors. The interval between the flexor carpi ulnaris and common flexor tendons is then used. The common flexors are retracted radially, and the flexor carpi ulnaris and the ulnar nerve are retracted ulnarly. The joint space is identified with a spinal needle, and the capsule is again opened bluntly. Because there is no true safe zone for the volar ulnar portal, it requires a careful dissection and spread technique (Fig. 19-11).17 This portal provides access for reduction of a distal radius fracture and a view of the dorsal articular surfaces and dorsal ligaments.
Distal Radioulnar Portals.
The distal radioulnar joint (DRUJ) is difficult to examine, and arthroscopy is not frequently used in these cases. The proximal and distal DRUJ portals are named according to their location proximal or distal to the ulnar head. The DRUJ portals are bordered radially by the EDC and ulnarly by the ECU. The joint is entered from at the base of the DRUJ, bordered by the radius and ulna. The proximal portal is placed in this line just proximal to the DRUJ. The forearm is supinated to relax the dorsal capsule, and the arthroscope is then introduced between the radius and ulna underneath the TFCC and proximal to the articular surface. The radioulnar articular surfaces can then be seen. Pronation and supination increase the available surface area during examination.
The distal portal is not always accessible. Use of this portal allows the surgeon to examine the distal articular surface of the ulna and the undersurface of the TFCC. The DRUJ portal uses a mini-open approach. It is located just proximal to the TFCC, and care must be taken to stay below the TFCC to prevent injury to this structure. There is some risk to the posterior interosseous nerve.8 There is minimal risk to sensory nerves, with the closest 17.5 mm distally.11
Neurovascular Structure Risk
Because of the absence of major neurovascular structures, most wrist arthroscopy uses the dorsum of the wrist. Only the deep branch of the radial artery and the superficial dorsal sensory branches of the radial, ulnar, and lateral antebrachial cutaneous nerves are located on the dorsal side of the wrist.8 Injury to these structures can cause numbness and, at worst, a painful neuroma and complex regional pain syndrome. Certain portals have an increased risk of iatrogenic neurovascular injury. The greatest risk to the radial artery and dorsal radial and ulnar sensory nerve branches occur with the 1-2, 6R, and 6-U portals. The midcarpal, 3-4, 4-5, and distal radioulnar joint portals are relatively safe.
Risk does exists even in safe portals because aberrant sensory nerve branches can be dangerously close.11 This usually necessitates incisions that are longitudinal and are made by pulling only the skin over a blade and bluntly spreading through the subcutaneous tissue. When piercing the capsule, only a blunt trocar should be used. This technique helps protect structures between the dermis and capsule from injury.11
Diagnostic Arthroscopy
The details of the diagnostic arthroscopy are covered in a later chapter, but we include some thoughts about evaluating the wrist. To perform an adequate diagnostic arthroscopy requires familiarity with the normal-appearing structures. This includes the ability to differentiate normal from pathologic structures. The appearance of the normal, white, smooth articular cartilage must be differentiated from the more yellow fibrocartilage.
The surgeon should be able to identify cracked and fibrillated tissue and eburnated bone. Ligaments should have a white or yellow appearance and should be taut when probed, especially under traction. Pathologic ligaments may become attenuated with fraying due to injury or degeneration. Inflammation may cause the synovium to become hypertrophic and reddish. A discolored or brown tinge to synovial fluid likely represents a pathologic problem. Joints should be congruous without step-offs, and ligaments should be tight without the ability to pass a probe from the radiocarpal joint.12
Dry Wrist Arthroscopy
A newer technique that uses wrist arthroscopy without irrigation has been tried. Proponents claim that there are benefits to arthroscopy without water, including limiting loss of vision and compartment syndrome. Another possible advantage is the ability to do open procedures without soft tissue infiltration. The investigators also suggest the possibility of less pain and swelling after surgery.18 No prospective studies have evaluated these reported benefits, and this technique is still in its early stages.
COMPLICATIONS
Complications during and after wrist arthroscopy are rare. Most physicians report rates of less than 2%.4,5 A study of 210 patients reported only two (0.9%) major complications and nine (4.3%) minor complications, all of which resolved with observation. The most common complication was dorsal ulnar sensory neuropraxia, and it was associated with open procedures.19 Complications can be the result of traction and arm positioning or related to establishment of portals. They can be procedure-specific complications or general arthroscopic complications. Major complications include compartment syndrome, permanent nerve injury, postsurgical joint infection, vascular injury, complex regional pain syndrome, permanent stiffness, and tendon rupture.19
Most complications can be prevented if the risks are understood and simple precautions are used when performing the surgery. Large instrumentation within a small joint space predisposes to iatrogenic injuries to nerves, the radial artery, and extensor tendons. The EPL and EDQ are the tendons most at risk during wrist arthroscopy. Flexible nylon finger traps help prevent skin damage for patients with friable skin.4 Using a spinal needle ensures an adequate pathway, and blunt trocars help to minimize risk to the articular surfaces.
Excessive extravasation of fluid may occur in recently injured patients with torn capsules or if the inflow cannula is placed extra-articularly. If extravasation occurs, the causative factor should be addressed, or the arthroscopic portion of the procedure should be stopped. Pressure diminishes quickly when the inflow is halted, and elevating the extremity is usually all that is necessary for correction. Physiologic solutions allow better fluid absorption in the soft tissues and further decrease the risk of extravasation.7 Whipple reports the risk of compartment syndromes is minimal to none because, even in the case of intra-articular fractures, extravasated fluid is rapidly absorbed by clysis and does not increase compartment pressures long enough to compromise circulation. Caution is advised if pressure pumps are used.20
Postoperative infection is uncommon. If there is any evidence of superficial infection, oral antibiotics are usually sufficient. If a deep intra-articular infection develops, irrigation, arthroscopic débridement, and intravenous antibiotic therapy are usually required.21
PEARLS& PITFALLS
CONCLUSIONS
Wrist arthroscopy provides an accurate supplement to a complete wrist examination. Although once used as a tool for diagnosis only, this is no longer the case. As technology advances, arthroscopy can be used in more complicated cases, and our ability to master new and advanced procedures will continue to improve. Although simple to learn and relatively easy to master, arthroscopy requires a thorough understanding of surgical principles and anatomy to perform procedures successfully. With adherence to standard precautions, wrist arthroscopy will continue to prove beneficial in the management of disorders of the wrist.
1. Chen YC. Arthroscopy of the wrist and finger joints. Orthop Clin North Am. 1979;10:723-733.
2. Whipple TL, Cooney WP3rd, Osterman AL, Viegas SF. Wrist arthroscopy. Instr Course Lect. 1995;44:139-145.
3. Whipple TL, Marotta JJ, Powell JH3rd. Techniques of wrist arthroscopy. Arthroscopy. 1986;2:244-252.
4. Bain GI, Munt J, Turner PC. New advances in wrist arthroscopy. Arthroscopy. 2008;24:355-367.
5. Haisman JM, Matthew B, Scott W. Wrist arthroscopy: standard portals and arthroscopic anatomy. J Am Soc Surg Hand. 2005;5:175-181.
6. Berger RA. Arthroscopic anatomy of the wrist and distal radioulnar joint. Hand Clin. 1999;15:393-413. vii
7. Geissler WB, Freeland AE, Weiss AP, Chow JC. Techniques of wrist arthroscopy. Instr Course Lect. 2000;49:225-237.
8. Gupta R, Bozentka DJ, Osterman AL. Wrist arthroscopy: principles and clinical applications. J Am Acad Orthop Surg. 2001;9:200-209.
9. Jones WA, Lovell ME. The role of arthroscopy in the investigation of wrist disorders. J Hand Surg Br. 1996;21:442-445.
10. Maizlin ZV, Brown JA, Clement JJ, et al. MR arthrography of the wrist: controversies and concepts. Hand (N Y). 2009;4:66-73.
11. Abrams RA, Petersen M, Botte MJ. Arthroscopic portals of the wrist: an anatomic study. J Hand Surg Am. 1994;19:940-944.
12. Bettinger PC, Cooney WP3rd, Berger RA. Arthroscopic anatomy of the wrist. Orthop Clin North Am. 1995;26:707-719.
13. Hofmeister EP, Dao KD, Glowacki KA, Shin AY. The role of midcarpal arthroscopy in the diagnosis of disorders of the wrist. J Hand Surg Am. 2001;26:407-414.
14. Carro LP, Golano P, Farinas O, et al. The radial portal for scaphotrapeziotrapezoid arthroscopy. Arthroscopy. 2003;19:547-553.
15. Abe Y, Doi K, Hattori Y, et al. A benefit of the volar approach for wrist arthroscopy. Arthroscopy. 2003;19:440-445.
16. Slutsky DJ. Wrist arthroscopy through a volar radial portal. Arthroscopy. 2002;18:624-630.
17. Slutsky DJ, Nagle DJ. Wrist arthroscopy: current concepts. J Hand Surg Am. 2008;33:1228-1244.
18. del Pinal F, Garcia-Bernal FJ, Pisani D, et al. Dry arthroscopy of the wrist: surgical technique. J Hand Surg Am. 2007;32:119-123.
19. Beredjiklian PK, Bozentka DJ, Leung YL, Monaghan BA. Complications of wrist arthroscopy. J Hand Surg Am. 2004;29:406-411.
20. Whipple TL. Precautions for arthroscopy of the wrist. Arthroscopy. 1990;6:3-4.
21. Botte MJ, Cooney WP, Linscheid RL. Arthroscopy of the wrist: anatomy and technique. J Hand Surg Am. 1989;14:313-316.