CHAPTER 1 Wrist Arthroscopy Portals
Introduction
Since its inception, wrist arthroscopy has continued to evolve. The initial emphasis on viewing the wrist from the dorsal aspect arose from the relative lack of neurovascular structures as well as the familiarity of most surgeons with dorsal approaches to the radiocarpal joint. Anatomical studies provided a better understanding of both the interosseous ligaments as well as carpal kinematics, which led to the development of midcarpal arthroscopy. Innovative surgeons continued to push the envelope through the development of techniques for treating intracarpal pathology, which in turn culminated in a plethora of new accessory portals. This chapter explores the standard arthroscopic portals, as well as some of the more recent and special-use portals.1
Indications
Midcarpal arthroscopy is essential in making the diagnosis of scapholunate and lunotriquetral instability. The grading scale reported by Geissler et al.2 provides a means of staging the degree of instability in order to provide an algorithm for treatment. Midcarpal arthroscopy is also useful for the assessment and treatment of chondral lesions of the proximal hamate.3 The triquetro-hamate joint can also be accessed through another special-use midcarpal portal.4
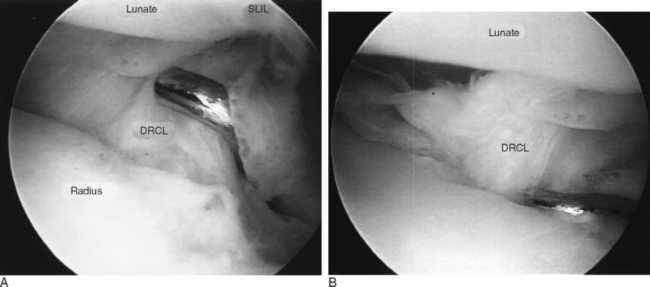
The clinical utility of volar portals has been recently elucidated.5–7 As kinematic and biomechanical studies have shed light on the role of the dorsal capsular structures and palmar subregions of the interosseous ligaments in maintaining carpal stability, it has become prudent to view the wrist from a palmar perspective. Volar portals for wrist arthroscopy have certain advantages over the standard dorsal portals for visualizing dorsal capsular structures as well as the palmar aspects of the carpal ligaments. The volar radial (VR) portal is relatively easy to use and is an ideal portal for evaluation of the dorsal radiocarpal ligament (DRCL) and the palmar subregion of the scapholunate interosseous ligament (SLIL). It facilitates the identification of and repair of DRCL tears.8,9 The VR portal also facilitates arthroscopic reduction of intra-articular fractures of the distal radius fractures by providing a clear view of the dorsal rim fragments.10
The volar radial midcarpal (VRM) portal may be considered an occasional accessory portal for visualizing the palmar aspects of the capitate and hamate in cases of avascular necrosis or osteochondral fractures.6 This portal facilitates visualization of the palmar aspect of the capitohamate interosseous ligament (CHIL), which is important in minimizing translational motion11 and has an essential role in providing stability to the transverse carpal arch.12
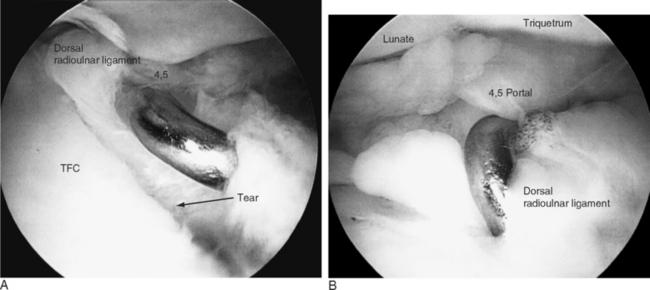
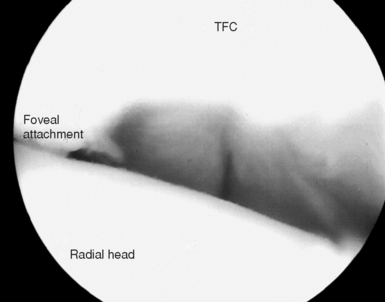
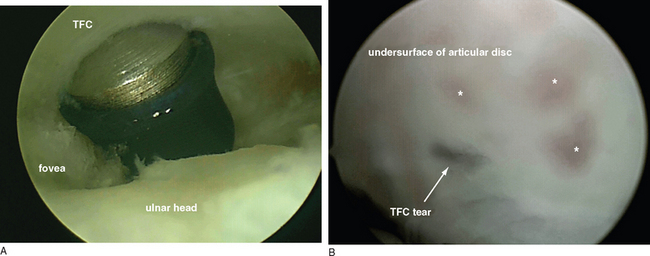
The volar ulnar (VU) portal provides unparalleled views of the dorsal radioulnar ligament and the dorsal ulnar wrist capsule, which contains the extensor carpi ulnaris subsheath (ECUS). Establishing the VU portal is more technically demanding but has potential use in the arthroscopic diagnosis and treatment of patients with ulnar sided wrist pain and suspected injuries to the ulnar sling mechanism. It is especially useful for visualizing and debriding palmar tears of the lunotriquetral ligament.13 It also aids in the repair or debridement of dorsally located TFC tears because the proximity of the 4/-,5 and 6R portals makes triangulation of the instruments difficult. The volar aspect of the distal radioulnar joint can be visualized through the VU portal to assess the foveal attachment of the triangular fibrocartilage in cases of suspected peripheral detachment of the TFC.7
Relevant Anatomy
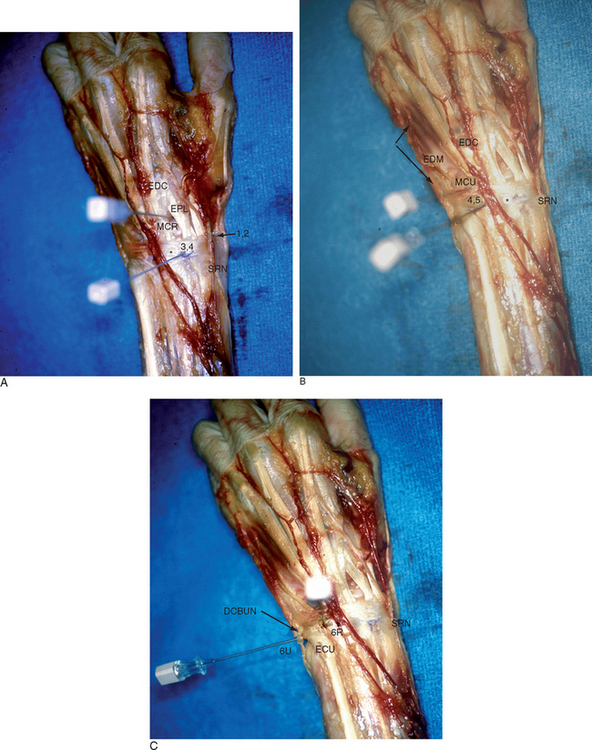
The standard portals for wrist arthroscopy are mostly dorsal (Figure 1.1a through c). This is in part due to the relative lack of neurovascular structures on the dorsum of the wrist as well as the initial emphasis on assessing the volar wrist ligaments. The dorsal portals, which allow access to the radiocarpal joint, are so named in relation to the tendons of the dorsal extensor compartments. For example, the 1-/,2 portal lies between the first extensor compartment tendons—which include the extensor pollicus brevis (EPB) and the abductor pollicus longus (APL)—and the second extensor compartment, which contains the extensor carpi radialis brevis and longus (ECRB/L).
Dorsal Cortals
Dorsal Radiocarpal Portals
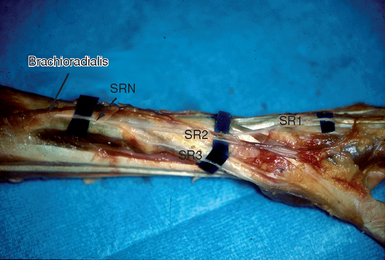
Abrams and co-workers performed anatomical dissections on 23 unembalmed fresh cadaver extremities and measured the distances between the standard dorsal portals and the contiguous neurovascular structures.14 The 1-/,2 portal was found to be the most perilous. The radial sensory nerve exits from under the brachioradialis approximately 5 cm proximal to the radial styloid and bifurcates into a major volar and a major dorsal branch at a mean distance of 4.2 cm proximal to the radial styloid15 (Figure 1.2). Branches of the superficial radial nerve (SRN) that were radial to the portal were within a mean of 3 mm (range 1 to 6 mm), whereas branches that were ulnar to the portal were at a mean of 5 mm (range 2 to 12 mm).
The radial artery was found at an average of 3 mm radial to the portal (range 1 to 5 mm). Either partial or complete overlap of the lateral antebrachial cutaneous nerve (LABCN) with the SRN occurs up to 75% of the time.16 In an anatomical study by Steinberg et al., the LACBN was present within the anatomical snuffbox in 9 of 20 (45%) specimens. Based on these findings, they recommended a more palmar, proximal portal in the snuffbox that was no more than 4.5 mm dorsal to the first extensor compartment and within 4.5 mm of the radial styloid.15
The dorsal cutaneous branch of the ulnar nerve (DCBUN) arises from the ulnar nerve an average of 6.4 cm (SD = 2.3 cm) proximal to the ulnar head and becomes subcutaneous 5 cm proximal to the pisiform. It crosses the ulnar snuffbox and gives off three to nine branches that supply the dorsoulnar aspect of the carpus, small finger, and ulnar ring finger.17 The mean distance of the dorsal cutaneous branch of the ulnar nerve (DCBUN) to the 6R portal was 8.2 mm (range 0 to 14 mm). Transverse branches of the DCBUN were found in 12 of 19 specimens and were noted to be within 2 mm of the portal (range 0 to 6 mm). The mean distance of branches of the dorsal cutaneous branch of the ulnar nerve (DCBUN) that were radial to the 6U portal was 4.5 mm (range 2 to 10 mm), whereas branches that were ulnar to the portal ranged from 1.9 to 4.8 mm on average. Any transverse branches of the DCBUN were generally proximal to the portal, at an average of 2.5 mm.
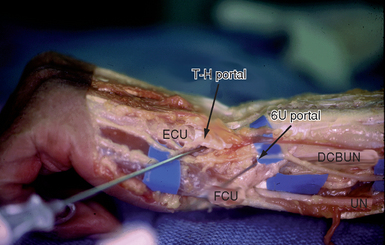
Triquetro-Hamate (TH) Portal
This portal enters the midcarpal joint at the level of the triquetro-hamate joint ulnar to the ECU tendon. The entry site is both ulnar and distal to the MCU. Branches of the DCBUN are most at risk (Figure 1.3).
Volar Portals
Volar Radial (VR) Portal
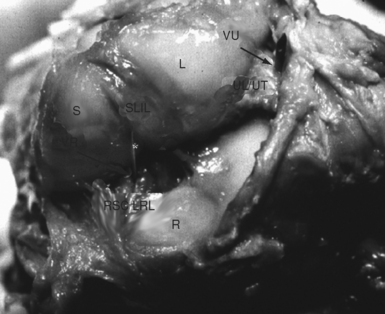
An anatomical study was performed on the arms of five fresh frozen cadavers to determine the safe landmarks for a volar radial (VR) portal after arterial injection studies to highlight the vascular anatomy.6 The proximal and distal wrist creases were marked. The volar skin was then removed and the flexor carpi radialis tendon (FCR) sheath was divided. The tendon was retracted ulnarly and a trochar was inserted into the radiocarpal joint at the level of the proximal wrist crease. The trochar was noted to enter the radiocarpal joint between the radioscaphocapitate ligament (RSC) and the long radiolunate ligament (LRL) in four specimens and through the LRL ligament in one specimen (Figure 1.5). The median nerve was 8 mm (range 6 to 10 mm) ulnar to the VR portal, whereas the palmar cutaneous branch passed 4 mm (range 3 to 5 mm) ulnar to the portal.
The radial artery was 5.8 mm (range 4 to 6 mm) radial to the portal and its superficial palmar branch was located 10.6 mm (range 6 to 16 mm) distal to the portal. The superficial radial nerve lay 15.6 mm (range 12 to 19 mm) radial to the portal. The portal was 12.8 mm (range 12 to 14 mm) distal to the border of the pronator quadratus, which roughly corresponds to the palmar radiocarpal arch.18 The palmar cutaneous branch was closest in proximity but always lies to the ulnar side of the FCR.19,20 The superficial palmar branch of the radial artery passed through the subcutaneous tissue over the tuberosity of the scaphoid and was out of harms way with an incision at the proximal wrist crease.21,22 When the trochar was placed through the floor of the FCR tendon sheath at the proximal palmar crease, the carpal canal was not violated. It was thus apparent that there was a safe zone comprising the width of the FCR tendon and at least 3 mm or more in all directions. This zone was free of any neurovascular structures.
Volar Radial Midcarpal (VRM) Portal
The volar aspect of the midcarpal joint was identified with a 22-gauge needle through the same skin incision and a blunt trochar was inserted. It was necessary to angle the trochar in a distal and ulnar direction (approximately 5 degrees) in order to access the midcarpal joint through the same skin incision. The trochar passed closer to (but still deep to) the superficial palmar branch of the radial artery, which coursed more superficially over the scaphoid tuberosity at that level. The distance between the volar radiocarpal and volar midcarpal entry sites averaged 11 mm (range 7 to 12 mm).
Volar Ulnar (VU) Portal
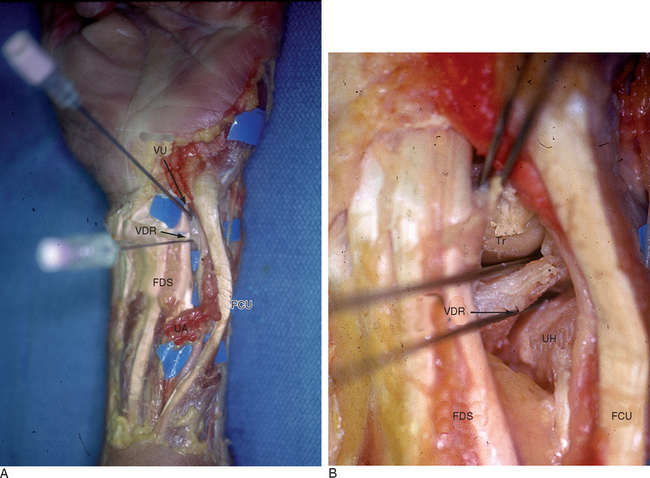
In a companion study, a volar ulnar (VU) portal was established via a 2-cm longitudinal incision made along the ulnar edge of the finger flexor tendons at the proximal wrist crease.13 The flexor tendons were retracted radially and a trochar was introduced into the radiocarpal joint. The ulnar styloid marked the proximal point of the VU portal, approximately 2 cm distal to the pronator quadratus. The portal was in the same sagittal plane as the ECU subsheath and penetrated the ulnolunate ligament (ULL) adjacent to the radial insertion of the triangular fibrocartilage. The ulnar nerve and artery were generally more than 5 mm from the trochar, provided the capsular entry point was deep to the ulnar edge of the profundus tendons.
The palmar cutaneous branch of the ulnar nerve (nerve of Henlé) was highly variable and not present in every specimen. This inconstant branch provides sensory fibers to the skin in the distal ulnar and volar part of the forearm to a level 3 cm distal to the wrist crease. Its territory may extend radially beyond the palmaris longus tendon.23 This branch tends to lie just to the ulnar side of the axis of the fourth ray, but it was absent in 43% of specimens in one study.24 Martin et al. demonstrated that there was no true internervous plane due to the presence of multiple ulnar-based cutaneous nerves to the palm, which puts them at risk with any ulnar incision.19 Because there is no true safe zone, careful dissection and wound spread technique should be observed.
Field of View
The following sections describe the typical field of view as seen through a 2.7-mm arthroscope under ideal conditions.25,26 Synovitis, fractures, ligament tears, and a tight wrist joint may limit the field of view (which necessitates the use of more portals to adequately assess the entire wrist).
1-/,2 Portal
Structures visualized are limited to the radial half of the wrist.
VR Portal
This portal is largely indicated to assess the palmar SLIL and the DRCL. It is also of use for arthroscopically assisted fixation of distal radius fractures due to the direct line of sight with the dorsal rim fragments.10
Relevant Clinical and Biomechanical Studies
The publications on the use of wrist arthroscopy through the standard dorsal portals are too numerous to list here. There are, however, a number of excellent reviews the reader is directed to.* A number of reports highlight the safety and clinical application of volar arthroscopy portals on the radial side of the wrist. Levy and Glickel27 described the use of an accessory volar portal after volar plating of a Barton’s fracture that was accessed through a standard carpal tunnel incision. Tham et al.28 used a volar radial portal in 14 cases (for synovectomy, radial styloidectomy, and fracture reduction). Bain and co-workers published their early experience with a volar portal in the European literature.29 They subsequently reported on the use of a volar portal for arthroscopic release of wrist contracture,30 as an adjunct for arthroscopic-assisted fixation of distal radius fractures,31 and for decompression of intraosseous ganglia of the lunate.32
Osterman described the use of a volar radial portal for arthroscopic release of dorsal wrist contractures.33 Doi et al. used a volar radial portal in 34 cases of arthroscopically assisted reduction of distal radius fractures.10 Abe et al. reported on the use of this portal for viewing the palmar aspects of the SLIL and LTIL ligaments in 230 cases.34,35 Del Piñal and co-workers recently reported on the use of a volar radial portal for an inside-out osteotomy technique for correction of malunited intra-articular distal radius fractures.36 Dr. Andrea Atzei and Riccardo Luchetti of Italy have used a palmar distal radioulnar joint portal that is ulnar to the TFCC. They presented their three year results at the FESSH meeting in 2005.37
Author’s Experience
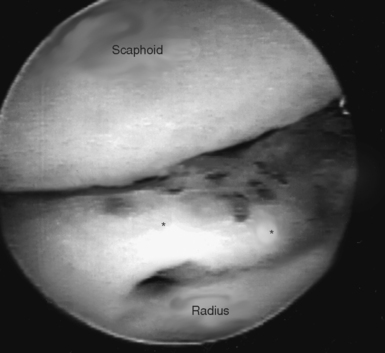
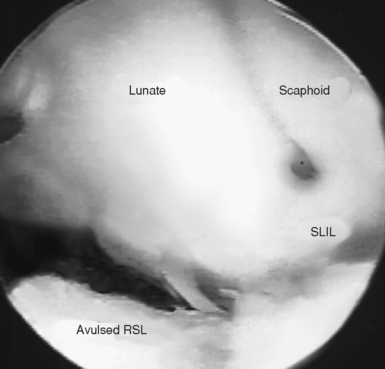
The volar radial portal has been used in 77 patients since 1998. Additional pathology was evident in 37 of the patients that was not visible from any standard dorsal portal. This included one case of hypertrophic synovitis of the dorsal capsule (Figure 1.7); one patient with an avulsion of the radioscapholunate ligament, which exposed the volar scapholunate cleft (Figure 1.8); two patients with tears restricted to the palmar region of the SLIL; and 35 patients with tears of the dorsal radiocarpal ligament. In five patients an isolated DRCL tear alone was responsible for chronic dorsal wrist pain (Figure 1.9a and b).
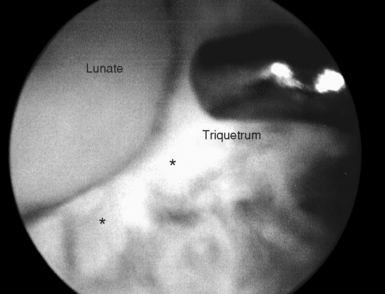
The midcarpal joint was accessed from the volar radial portal in three cases. In one patient with Preiser’s disease the use of the volar radial midcarpal portal (VRM) allowed a more complete assessment of the distal articular surface of the scaphoid. Another patient had an unrecognized osteochondral fracture of the capitate head following a perilunate dislocation. The VRM portal admirably demonstrated the intact dorsal portion of the SLIL in the patient with the palmar tear (Figure 1.10). Using the dorsal midcarpal portals, one patient was found to have a chondral defect on the proximal hamate, along with a midcarpal loose body (Figure 1.11a and b).
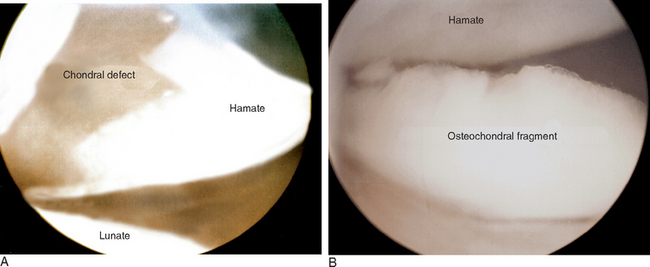
FIGURE 1.11 Dorsal midcarpal portal. (A) Chondral defect on proximal hamate. (B) Loose body in midcarpal joint.
The VU portal was used in 49 of these patients. The ulnar sided pathology included 13 tears of the LTIL ligament, 11 TFC tears, and 2 ulnolunate ligament tears. In one patient a TFC tear was found to extend into the dorsoulnar ligament (see Figure 1.12a and b). The VU portal facilitated debridement of the palmar region of the LTIL ligament through the 6R or 6U portals (Figure 1.13). In 2 of these patients unrecognized chondromalacia of the palmar aspect of the lunate was identified (see Figure 1.14). In 1 patient, the palmar aspect of the LTIL was found to be intact despite a large dorsal tear.
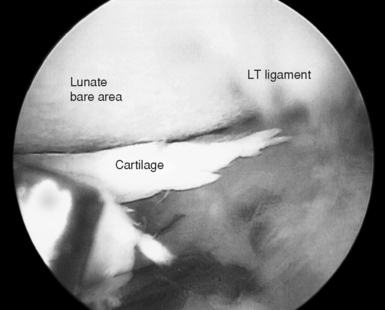
FIGURE 1.14 Unsuspected region of chondromalacia on the palmar surface of the lunate (LT = lunotriquetral).
(From Slutsky DJ. The use of a volar ulnar portal in wrist arthroscopy. The Journal of Arthroscopic and Related Surgery 2004;20(2): 158–63. Used with permission.)
The volar aspect of the DRUJ portal was used in six of these patients to rule out a peripheral detachment of the TFC (2 with ulnar styloid fracture/nonunion). This would normally require a formal open arthrotomy and a high index of clinical suspicion.41 The DRUJ was well visualized and the foveal attachment of the TFC was clearly identified (see Figure 1.15). In one patient with a TFC and LTIL tear, a wafer resection was performed by inserting the bur through the dorsal DRUJ portal while viewing through the VDRU. This allows for a more conservative TFC debridement since the ulnar head resection if performed underneath the TFC tear and not through it. The DRUJ wafer also facilitates preservation of the volar and dorsal radioulnar ligaments as well as the deep foveal attachment.
Equipment and Implants
Optional
There are a variety of commercially available suture repair kits, including the TFC repair kit by Arthrex or Linvatec (Conmed – Linvatec Corporation, Largo, FL). Ligament repairs can also be facilitated by use of a Tuohy needle, which is generally found in any anesthesia cart. Specially designed jigs have been made to facilitate repair of radial TFC tears,38 although Trumble et al. have described a method with meniscal repair needles passed through a suction cannula in the 6U portal.39
Methodology
It is useful to have a systematic approach to viewing the wrist. The structures that should be visualized as part of a standard exam include the radius articular surface, the proximal scaphoid and lunate, the SLIL and LTIL (palmar and dorsal for each), RSC, LRL, RSL, ULL, ULT, and the radial and peripheral TFCC attachments. It is my practice to establish the dorsal portals first but then to start the arthroscopic examination with the VR portal in order to visualize the palmar SLIL and the DRCL ligament to minimize any error from iatrogenic trauma to the dorsal capsular structures. This is followed by the VU portal to assess the palmar LTIL and dorsal radioulnar ligament, ECU subsheath, and radial TFC attachment.
Midcarpal Portals
The MCR portal is found 1 cm distal to the 3-/,4 portal. Flexing the wrist and firm thumb pressure help identify the soft spot between the distal pole of the scaphoid and the proximal capitate. The STT joint lies radially and can be seen by rotating the scope dorsally. The scapholunate articulation can be seen proximally and ulnarly, which can be probed for instability or step-off. Further ulnarly, the lunotriquetral articulation is visualized. Superiorly, oblique views of the proximal surface capitate and hamate as well as the CHIL are obtained. The continuation of the RSC ligament can occasionally be seen across the midcarpal space.
The MCU is found 1 cm distal to the 4-/,5 portal, and 1.5 cm ulnar and slightly proximal to the MCR portal (in line with the fourth metacarpal axis). This entry site is at the intersection of the lunate, triquetrum, hamate, and capitate with a type I lunate facet and directly over the lunotriquetral joint with a type II lunate facet4 (which allows preferential views of this articulation). Directly volar, the continuation of the volar ulnocarpal ligament can be assessed (which is especially important in midcarpal instability).
Volar Portals
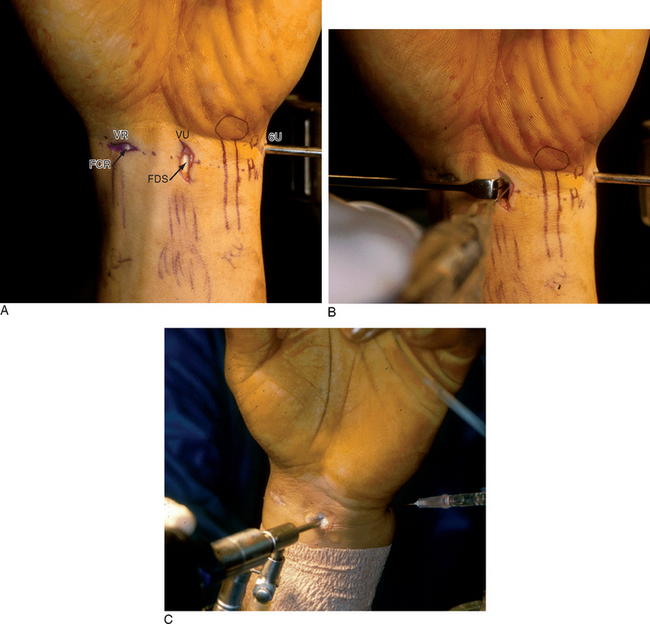
To establish the volar radial portal the surgeon is now seated, facing the volar aspect of the wrist. A 2-cm transverse or longitudinal incision is made in the proximal wrist crease overlying the flexor carpi radialis (FCR) tendon. It is not necessary to specifically identify the adjacent neurovascular structures, provided the anatomical landmarks are adhered to. The tendon sheath is divided and the FCR tendon is retracted ulnarly. The radiocarpal joint space is identified with a 22-gauge needle and distended with 5 cc of saline. Blunt tenotomy scissors or forceps are used to pierce the volar capsule. A blunt trochar is then introduced, followed by a 2.7-mm 30-degree angled arthroscope (Figure 1.16a through c). The midcarpal joint can be accessed through the same skin incision by angling the trochar 1 cm distally and approximately 5 degrees ulnarward. Outflow is established via an 18-gauge needle in the 6U portal or a cannula.
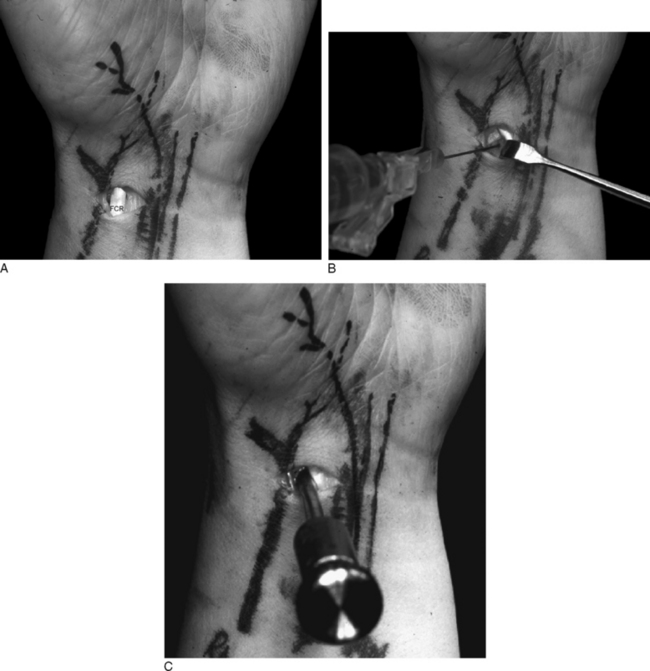
(From Slutsky DJ. Volar portals in wrist arthroscopy. JASSH 2002;2(4):225–32. Used with permission.)
The volar ulnar portal is established via a 2-cm longitudinal incision centered over the proximal wrist crease along the ulnar edge of the finger flexor tendons (Figure 1.17a through c). The tendons are retracted to the radial side and the radiocarpal joint space is identified with a 22-gauge needle. Blunt tenotomy scissors or forceps are used to pierce the volar capsule, followed by insertion of a cannula and blunt trochar, followed by the arthroscope. The ulnar nerve is protected by use of the cannula and a more radial entry site. The median nerve is protected by the adjacent flexor tendons. The palmar region of the LTIL can usually be seen slightly distal and radial to the portal. A hook probe is inserted through the 6R or 6U portal.
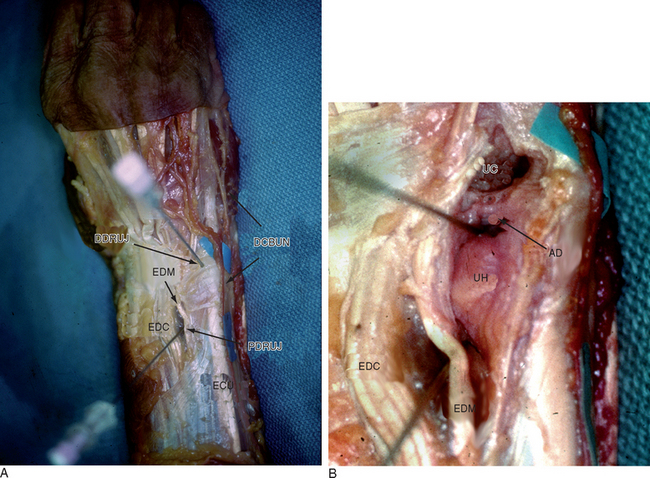
The dorsal radioulnar joint can be accessed through a proximal and distal portal.40 The proximal portal (PDRUJ) is located in the axilla of the joint, just proximal to the sigmoid notch and the flare of the ulnar metaphysis. This portal is easier to penetrate and should be used initially to prevent chondral injury from insertion of the trochar. The forearm is held in supination to relax the dorsal capsule, to move the ulnar head volarly, and to lift the central disc distally from the head of the ulna. Reducing the traction to 1 to 2 pounds permits better views between the ulna and the sigmoid notch by reducing the compressive force caused by axial traction.
The distal portal (DDRUJ) is identified 6 to 8 mm distally with the 22-gauge needle, and just proximal to the 6R portal. This portal can be used for outflow drainage or for instrumentation. It lies on top of the ulnar head but underneath the TFC. Hence, it cannot be used in the presence of a positive ulnar variance. The TFC has the least tension in neutral rotation of the forearm, which is the optimal position for visualizing the articular dome of the ulnar head, the undersurface of the TFC, and the proximal radioulnar ligament from its attachment to the sigmoid notch to its insertion into the fovea of the ulna. Because of the dorsal entry of the arthroscope, the course of the dorsal radioulnar ligament is not visible until its attachment into the fovea is encountered.25 Proximal surface tears of the TFC (which are usually caused by severe axial load) may be detected through this portal.
The volar DRUJ portal is accessed through the VU skin incision. A 1.9-mm small joint arthroscope is used since gaining access to the DRUJ can be difficult, especially in a small wrist. The joint is first identified by angling a 22-gauge needle 45° proximally, and then injecting the DRUJ with saline. It is useful to leave a needle or cannula in the ulnocarpal joint for reference during this step. Alternatively, a probe can be placed in the distal dorsal radioulnar joint portal and advanced through the palmar incision to help locate the joint space. Care is taken to situate the portal underneath the ulnar edge of the flexor tendons and to apply retraction in a radial direction alone, in order to avoid injury to the ulnar nerve and artery. Once the correct plane is identified, the volar DRUJ capsule is pierced with tenotomy scissors followed by a cannula with a blunt trochar and then the arthroscope. The dorsal distal DRUJ portal can be used for instrumentation such as a thermal probe or bur while viewing through the VDRU portal (Figure 1.18a and b).40
The Dry Technique of Wrist Arthroscopy
Dr. Francisco del Piñal of Santander, Spain, has pioneered a dry technique for diagnostic wrist arthroscopy.41 In his experience, this technique is as effective as the standard procedure but without the disadvantages of fluid extravasation, which minimizes the risk of compartment syndrome during the arthroscopic treatment of distal radius fractures. The hand is suspended from a custom-made traction bow that allows one to easily change the hand from a horizontal to a vertical position while maintaining a sterile field. The arthroscopy portals are made and instruments inserted as in the usual fashion, except for the fact that no irrigation fluid is used to distend the joint. To periodically dry the joint out, he uses neurosurgical patties cut into small triangles.
One must avoid getting too close with the tip of the scope when working with burs or osteotomes, in order to avoid splashes that might impede vision. Blood clots or debris are first wetted with 10 or 20 cc of saline through the side valve of the scope and then aspirated with a synoviotome. He has thus far carried out the dry technique in more than 100 wrist arthroscopies without any complications (personal communication, del Piñal June 2006). In my experience, it is still necessary to use fluid to make the diagnosis of a DRC ligament tear. Copious joint irrigation is also necessary whenever a thermal probe is used, to minimize the risk of heat necrosis of the articular cartilage.
1 Slutsky DJ. Wrist arthroscopy portals. In: Slutsky DJ, Nagel DJ, editors. Techniques in Hand and Wrist Arthroscopy. Philadelphia: Elsevier, 2007. (in press).
2 Geissler WB, Freeland AE, Savoie FH, McIntyre LW, Whipple TL. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365.
3 Harley BJ, Werner FW, Boles SD, Palmer AK. Arthroscopic resection of arthrosis of the proximal hamate: A clinical and biomechanical study. J Hand Surg [Am]. 2004;29:661-667.
4 Viegas SF. Midcarpal arthroscopy: Anatomy and portals. Hand Clin. 1994;10:577-587.
5 Slutsky DJ. Volar portals in wrist arthroscopy. Journal of the American Society for Surgery of the Hand. 2002;2:225-232.
6 Slutsky DJ. Wrist arthroscopy through a volar radial portal. Arthroscopy. 2002;18:624-630.
7 Slutsky DJ. Clinical applications of volar portals in wrist arthroscopy. Techniques in Hand and Upper Extremity Surgery. 2004;8:229-238.
8 Slutsky DJ. Arthroscopic repair of dorsal radiocarpal ligament tears. Arthroscopy. 2002;18:E49.
9 Slutsky DJ. Management of dorsoradiocarpal ligament repairs. Journal of the American Society for Surgery of the Hand. 2005;5:167-174.
10 Doi K, Hattori Y, Otsuka K, Abe Y, Yamamoto H. Intra-articular fractures of the distal aspect of the radius: Arthroscopically assisted reduction compared with open reduction and internal fixation. J Bone Joint Surg Am. 1999;81:1093-1110.
11 Ritt MJ, Berger RA, Kauer JM. The gross and histologic anatomy of the ligaments of the capitohamate joint. J Hand Surg [Am]. 1996;21:1022-1028.
12 Garcia-Elias M, An KN, Cooney WPd, Linscheid RL, Chao EY. Stability of the transverse carpal arch: An experimental study. J Hand Surg [Am]. 1989;14:277-282.
13 Slutsky DJ. The use of a volar ulnar portal in wrist arthroscopy. Arthroscopy. 2004;20:158-163.
14 Abrams RA, Petersen M, Botte MJ. Arthroscopic portals of the wrist: An anatomic study. J Hand Surg [Am]. 1994;19:940-944.
15 Steinberg BD, Plancher KD, Idler RS. Percutaneous Kirschner wire fixation through the snuff box: An anatomic study. J Hand Surg [Am]. 1995;20:57-62.
16 Mackinnon SE, Dellon AL. The overlap pattern of the lateral antebrachial cutaneous nerve and the superficial branch of the radial nerve. J Hand Surg [Am]. 1985;10:522-526.
17 Botte MJ, Cohen MS, Lavernia CJ, et al. The dorsal branch of the ulnar nerve: An anatomic study. J Hand Surg [Am]. 1990;15:603-607.
18 Gelberman RH, Panagis JS, Taleisnik J, Baumgaertner M. The arterial anatomy of the human carpus. Part I: The extraosseous vascularity. J Hand Surg [Am]. 1983;8:367-375.
19 Martin CH, Seiler JGIII, Lesesne JS. The cutaneous innervation of the palm: An anatomic study of the ulnar and median nerves. J Hand Surg [Am]. 1996;21:634-638.
20 DaSilva MF, Moore DC, Weiss AP, Akelman E, Sikirica M. Anatomy of the palmar cutaneous branch of the median nerve: Clinical significance. J Hand Surg [Am]. 1996;21:639-643.
21 Kamei K, Ide Y, Kimura T. A new free thenar flap. Plast Reconstr Surg. 1993;92:1380-1384.
22 Omokawa S, Ryu J, Tang JB, Han J. Vascular and neural anatomy of the thenar area of the hand: Its surgical applications. Plast Reconstr Surg. 1997;99:116-121.
23 Balogh B, Valencak J, Vesely M, et al. The nerve of Henle: An anatomic and immunohistochemical study. J Hand Surg [Am]. 1999;24:1103-1108.
24 McCabe SJ, Kleinert JM. The nerve of Henle. J Hand Surg [Am]. 1990;15:784-788.
25 Berger RA. Arthroscopic anatomy of the wrist and distal radioulnar joint. Hand Clin. 1999;15:393-413. vii.
26 Bowers WH. Arthroscopic anatomy of the wrist. In: McGinty J, editor. Operative Arthroscopy. New York: Raven Press; 1991:613-623.
27 Levy HJ, Glickel SZ. Arthroscopic assisted internal fixation of volar intraarticular wrist fractures. Arthroscopy. 1993;9:122-124.
28 Tham S, Coleman S, Gilpin D. An anterior portal for wrist arthroscopy: Anatomical study and case reports. J Hand Surg [Br]. 1999;24:445-447.
29 Bain GI, Pederini L. Procedure artroscopishe capsulari del polso. In: Pederini L, editor. Ortpedia E Chirugia Mini-invasiva. London: Springer-Verlag, 1999.
30 Verhellen R, Bain GI. Arthroscopic capsular release for contracture of the wrist: A new technique. Arthroscopy. 2000;16:106-110.
31 Mehta JA, Bain GI, Heptinstall RJ. Anatomical reduction of intra-articular fractures of the distal radius: An arthroscopically-assisted approach. J Bone Joint Surg [Br]. 2000;82:79-86.
32 Ashwood N, Bain GI. Arthroscopically assisted treatment of intraosseous ganglions of the lunate: A new technique. J Hand Surg [Am]. 2003;28:62-68.
33 Osterman AL, Bednar JM. The Arthroscopic Release of Wrist Contracture. Presented at the American Society for Surgery of the Hand. 55th Annual Meeting. Seattle, WA 2000.
34 Abe Y, Doi K, Hattori Y, Ikeda K, Dhawan V. Arthroscopic assessment of the volar region of the scapholunate interosseous ligament through a volar portal. J Hand Surg [Am]. 2003;28:69-73.
35 Abe Y, Doi K, Hattori Y, Ikeda K, Dhawan V. A benefit of the volar approach for wrist arthroscopy. Arthroscopy. 2003;19:440-445.
36 del Piñal F, Delgado J, Sanmartín M, Regalado J. Correction of malunited intra-articular distal radius fractures with an inside-out osteotomy technique. J Hand Surg (Am). 2006. (in press).
37 Atzei A, Luchetti R, Carità E, Papin Zorli I, Cugola L. Arthroscopically assisted faveal reinsertion of peripheral avulsions of the TFCC. J Hand Surg B. 2005;30:S1. :40
38 Trumble TE, Gilbert M, Vedder N. Isolated tears of the triangular fibrocartilage: Management by early arthroscopic repair. J Hand Surg [Am]. 1997;22:57-65.
39 Whipple TL. Arthroscopy of the distal radioulnar joint: Indications, portals, and anatomy. Hand Clin. 1994;10:589-592.
40 Slutsky DJ. Distal radioulnar joint arthroscopy and the volar ulnar portal. Techniques in Hand and Upper Extremity Surgery. 2007;11(1):1-7.
41 del Piñal F. Correction of malunited intra-articular distal radius fractures with an inside-out osteotomy technique. In: Slutsky DJ, Nagel DJ, editors. Techniques in Hand and Wrist Arthroscopy. Philadelphia: Elsevier, 2007. (in press).