28 Wrinkle Reduction with Nonablative Lasers
Nonablative laser treatments for wrinkle reduction (where the term lasers* refers to both lasers and intense pulsed light devices) are aimed at heating the dermis to cause mild injury, while leaving the epidermis intact. A reparative healing process ensues after treatment with collagen shrinkage and synthesis of new collagen and extracellular matrix, referred to as dermal collagen remodeling.1,2 Dermal thickness is increased and the skin is smoothed, resulting in clinical reduction of wrinkles. In addition to wrinkle reduction, collagen remodeling effects with nonablative lasers can also result in reduction of depression scars, pore size, and rough skin texture.
Laser Principles and Devices Currently Available
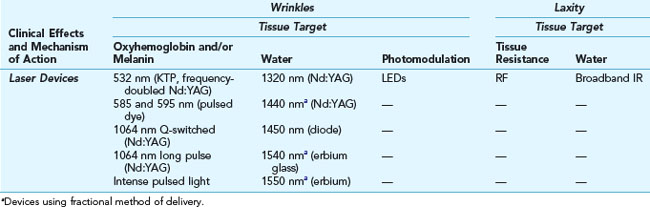
The mechanism by which most nonablative lasers effect collagen remodeling and wrinkle reduction is through focal thermal injury to the dermis while avoiding epidermal injury. Thermal injury can be induced through energy absorption in the skin by melanin, oxyhemoglobin, and/or water chromophores utilizing the principle of selective photothermolysis (see Chapter 19, Aesthetic Principles and Consultation).3 Other methods of inducing thermal injury include using radio-frequency energy, where tissue resistance to applied current heats the dermis. Some technologies utilize fractional methods of delivery that enhance the depth of laser penetration into the skin. Nonablative wrinkle reduction technologies can be broadly classified according to their clinical effects of wrinkle reduction or improvement in skin laxity, and this may be further refined based on the mechanism of action of the technology (see Table 28-1).
Wrinkle Reduction
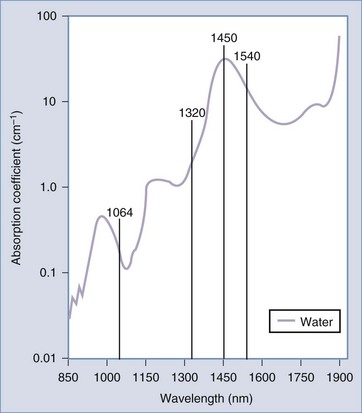
Many of the lasers used for nonablative wrinkle reduction target the water chromophore in tissue, including infrared (IR) wavelengths of 1320, 1440, 1450, 1540, and 1550 nm (1064 nm is also an IR wavelength but has less affinity for water). Figure 28-1 shows these wavelengths superimposed on the water absorption curve. By heating water, thermal energy is conducted to the dermal tissue, which stimulates the collagen remodeling process. All of these wavelengths have demonstrated clinical improvements in wrinkles.4–7
Some of the infrared lasers employ a fractional method of delivery (see Table 28-1), of which 1550 nm has the most data.8 Fractional lasers treat a portion or “fraction” of the skin by delivering laser energy in microscopic columns, called microthermal zones. Figure 19-10 in Chapter 19, Aesthetic Principles and Consultation, shows the pattern in the skin made by fractional laser devices. The untreated tissue between microthermal zones serves as a regenerative reservoir, which facilitates rapid wound healing.9 This type of treatment is termed nonablative fractional resurfacing. In addition to the collagen remodeling effects of wrinkle and scar reduction, fractional resurfacing with 1550 nm has also shown promise with reduction of dyschromic conditions such as melasma and poikiloderma of Civatte.10–12
Lasers that target oxyhemoglobin, melanin, and to a lesser degree water, such as 532 nm pulsed dye lasers (585 and 595 nm), and intense pulsed light devices (IPLs) have also been found to effect collagen remodeling and wrinkle reduction.13–15 However, the primary indication for these chromophore dependent lasers is reduction of vascular ectasias and/or pigmented lesions.
The Q-switched 1064 nm neodymium-doped yttrium aluminum garnet (Nd:YAG) laser was one of the first lasers to demonstrate nonablative reduction of wrinkles. Long-pulse 1064 nm Nd:YAG lasers are also used for reduction of wrinkles and results may be enhanced when combined with 532 nm.16–18 The long 1064 nm wavelength, as with other infrared lasers, allows for deep penetration to the dermis, which is desirable for collagen remodeling and, because it has little absorption by epidermal pigment, this wavelength is safe for all skin types. Studies with Q-switched 1064 nm lasers demonstrate histologic19,20 and clinical reduction of wrinkles, as well as other collagen remodeling effects, such as reduction of pore size, rough skin texture,21 and superficial acne scarring.22–24 Dermal collagen remodeling effects are due to both photothermal and photoacoustic vibration, which results from the inherent rapid, short (nanoseconds) pulses of Q-switched lasers.25 In addition to dermal remodeling, Q-switched 1064 nm lasers are also commonly used for tattoo removal,26 reduction of dermal pigmentation such as melasma,27–29 and reduction of fine dark hair.30 The diverse applications of Q-switched 1064 nm and other chromophore-dependent lasers offer a means to address many aesthetic skin complaints simultaneously.
Light-emitting diodes (LEDs) are a newer type of light-based device that emit a narrow range, or band, of wavelengths. They do not operate based on the theory of selective photothermolysis, but are instead based on the principle of photomodulation, whereby cellular activity is modulated through illumination with particular wavelengths of light.31 These devices have been used for mild wrinkle reduction32 and treatment of acne. Several LEDs are available that vary in wavelength and pulsing modes such as blue light devices (400 to 500 nm) which have superficial penetration, and red light devices (570 to 670 nm) which have deeper penetration. The main advantage of LEDs is their ease of use.
LEDs have also been used for skin rejuvenation as part of photodynamic therapy (PDT). PDT refers to selective tissue destruction through the use of a photosensitizing medication that is activated by a laser or light-based device (such as an LED or IPL).33 A topical photosensitizing medication such as aminolevulinic acid (Levulan®) is concentrated in particular tissues, such as sebaceous glands and actinically damaged cells. The photosensitizer is activated by a light source resulting in a cytotoxic reaction and destruction of the targeted areas.34 PDT is currently FDA approved for treatment of nonhyperkeratotic actinic keratoses, but is used off label to enhance the results with nonablative lasers for photorejuvenation and wrinkle reduction.35–37
Reduction of Skin Laxity
Skin laxity is treated with two main types of technologies: broadband infrared and radio-frequency (RF) devices.38 The improvements in laxity are believed to be due to collagen contraction initially, and later to collagen synthesis.39 Broadband infrared devices (such as the Cutera Titan™) emit wavelengths ranging from 1100 to 1800 nm with long pulse widths (of several seconds). Radio-frequency devices (such as Solta Thermage™) employ rapidly alternating current that creates heat when applied to the skin because of the skin’s resistance to the flow of current. Tissue heating with RF devices is controlled by several factors, including the type of electrodes used (e.g., monopolar or bipolar), fluence, and cooling times. These technologies have been shown to improve laxity in many areas of the body including the periocular region, nasolabial folds, jowls, neck, and abdomen.40–45 In addition to treatment of wrinkles and skin laxity, RF devices are also used for cellulite reduction.46 RF treatments have traditionally been associated with more discomfort than IR treatments, however, new techniques utilizing multiple passes with lower fluences have improved tolerability.47
Patient Selection
Patient selection for wrinkle reduction treatments with nonablative lasers is based on the degree of wrinkling present and patient expectations. Patients with mild to moderate static wrinkles and laxity (Glogau types I through III) are appropriate candidates (see Chapter 19, Aesthetic Principles and Consultation, for a description of Glogau types). Patients with deep static wrinkles and/or severe laxity (Glogau type IV) and those who desire more rapid and dramatic results may be better candidates for more aggressive procedures such as ablative laser resurfacing or surgery.
Products Currently Available
See the Resources section at the end of the chapter for a list of laser manufacturers.
Advantages of Nonablative Lasers for Wrinkles
Anatomy
Wrinkles result from many factors including skin changes with epidermal hypocellularity, loss of dermal matrix components including collagen, glycosaminoglycans, elastin, and atrophy of subcutaneous adipose tissue. Thinning of the skin combined with repetitive contraction of underlying musculature can etch wrinkles into the skin to form static lines.48
Nonablative laser treatments are aimed at reducing mild to moderate static wrinkles. Most of these technologies do so by producing papillary dermal injury, at an approximately 100 to 200 µm (0.1 to 0.2 mm) depth in the skin.49,50 Fractional nonablative laser treatments for wrinkles (e.g., fractional 1550 nm) penetrate up to 300 to 400 µm (0.3 to 0.4 mm).9 Nonablative lasers for laxity (e.g., RF lasers) penetrate to the reticular dermis, up to 1 to 3 mm.51
Procedure Preparation
Nonablative Lasers for Wrinkles: Steps and Principles
General Treatment Technique
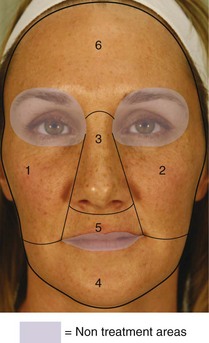
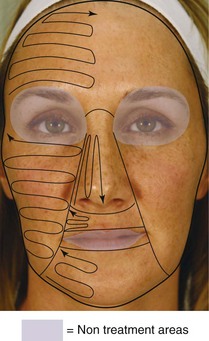
FIGURE 28-2 Nonablative Laser Safety Zone and sequence for wrinkle reduction treatments on the face.
(Copyright Rebecca Small, MD.)
Planning and Designing
Safety Zone
The area within which lasers may be used for wrinkle reduction treatments on the face is called the Nonablative Laser Safety Zone (Figure 28-2). Laser treatments are performed outside of the orbit: above the supraorbital ridge (above the eyebrows) and below the inferior orbital rim, to reduce the risk of ocular injury.
Performing the Procedure
Results
Treatments are performed in a series, and most nonablative wrinkle reduction lasers show improvements approximately 3 months after the initial treatment, with continued improvements up to 6 months following the last treatment. It is extremely important to inform patients that reduction of mild to moderate wrinkles with nonablative lasers is slow and results vary based on the technology used and with individual patients. Studies of nonablative lasers consistently show histologic improvements with increased numbers of fibroblasts and collagen deposition.23,52 However, clinical improvements are less predictable and do not always correlate with histologic changes. Figures 28-8 through 28-14 show before and after photos for some of the nonablative wrinkle reduction technologies discussed in the chapter.
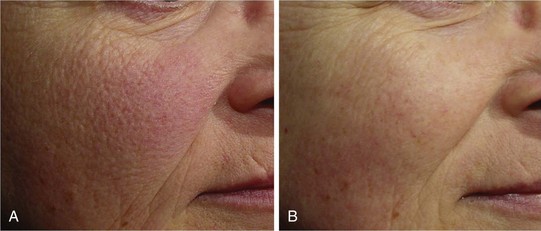
FIGURE 28-8 Facial wrinkles (A) before and (B) after a series of six treatments with a long-pulse 1064 nm Nd:YAG laser.
(Courtesy of Cutera, Brisbane, CA; laser genesis; photograph by K. Smith.)
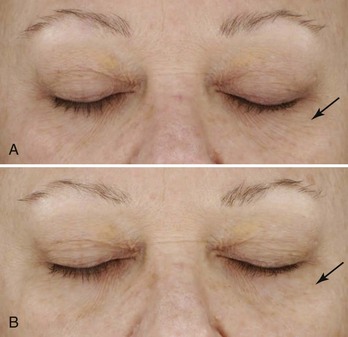
FIGURE 28-9 Infraocular wrinkles (A) before and (B) after a series of treatments with a Q-switched 1064 nm Nd:YAG laser.
(Courtesy of HOYA ConBio, Fremont, CA; laser toning by D. Goldberg, MD, using RevLite.)
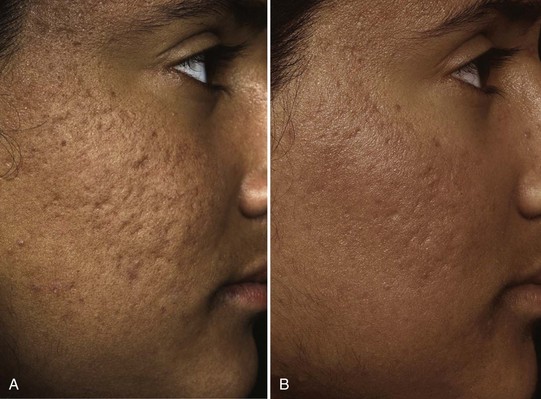
FIGURE 28-11 Acne scars (A) before and (B) after nonablative fractional resurfacing treatments using a 1550 nm laser.
(Courtesy of Solta, Hayward, CA; Z. Rahman, MD, using Fraxel Re:store™.)

FIGURE 28-12 Skin laxity of the lower face (A) before, (B) 6 months after, and (C) 3 years after a series of RF laser treatments.
(Courtesy of Solta, Hayward, CA; F. Mayoral, MD, using Thermage™.)

FIGURE 28-13 Skin laxity of the neck (A) before and (B) after a series of RF laser treatments.
(Courtesy of Solta, Hayward, CA; R. Euwer, MD, using Thermage™.)
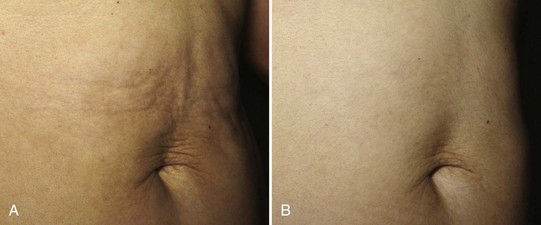
FIGURE 28-14 Skin laxity of the abdomen (A) before and (B) after a series of broadband IR laser treatments.
(Courtesy of Cutera, Brisbane, CA; J. Calkin, MD, using Titan™.)
Figure 28-8 shows results of nonablative wrinkle reduction treatments for facial rhytids (A) before and (B) after a series of six treatments with a long-pulse 1064 nm Nd:YAG laser (Cutera Laser Genesis™).
Figure 28-9 shows results of nonablative wrinkle reduction treatments for infraocular rhytids (A) before and (B) after a series of treatments with a Q-switched 1064 nm Nd:YAG laser (HOYA ConBio RevLite™).
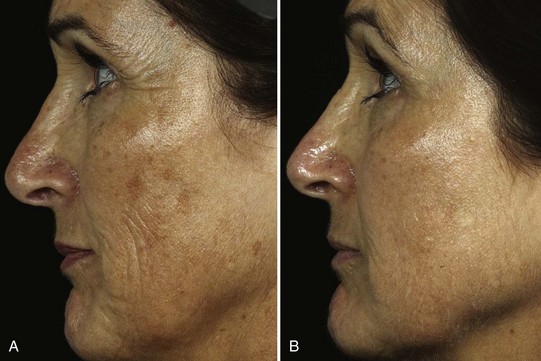
Figure 28-10 shows wrinkle reduction treatments for cheek rhytids and crow’s feet, as well as hyperpigmentation reduction (A) before and (B) after fractional resurfacing treatments using a 1550 nm laser (Solta Fraxel Re:store™).
Figure 28-11 shows results of nonablative collagen remodeling treatments for acne scars (A) before and (B) after fractional resurfacing treatments using a 1550 nm laser (Solta Fraxel Re:store™).
Figure 28-12 shows results of nonablative skin laxity reduction treatments of the lower face (A) before, (B) after 6 months, and (C) after 3 years following a series of RF treatments (Solta Thermage™).
Figure 28-13 shows results of nonablative skin laxity reduction treatments of the neck (A) before and (B) after a series of RF laser treatments (Solta Thermage™).
Figure 28-14 shows results of nonablative skin laxity reduction treatments of the abdomen (A) before and (B) after a series of broadband infrared treatments (Cutera Titan™).
Follow-Up
Nonablative laser treatments for wrinkle reduction typically require a series of six treatments at monthly intervals for demonstrable improvements, although fewer treatments may be required for fractional lasers. It is generally accepted that results persist for 1 to 2 years. Figure 28-12 shows recurrence of lower face laxity 3 years after RF treatment. Patients may, therefore, want to consider repeating a treatment series every 2 years. Alternatively, because these treatments are so well tolerated and results are cumulative, some providers recommend performing nonablative laser treatments as part of regular skin maintenance at monthly to quarterly intervals.
Complications

FIGURE 28-15 Petechiae of the neck with a nonablative laser wrinkle reduction treatment.
(Copyright Rebecca Small, MD.)

FIGURE 28-16 Preauricular urticaria with a nonablative laser wrinkle reduction treatment.
(Copyright Rebecca Small, MD.)
Petechiae may be seen with high fluences particularly in thin-skinned areas such as the neck (Figure 28-15). Purpura may occur with shorter wavelength lasers, particularly pulsed dye lasers, and when short pulse widths and/or high fluences are utilized during treatment.53 Petechiae typically take 3 to 5 days to resolve and purpura can take up to 2 weeks. Utilizing larger spot sizes, lower fluences, and skin compression can reduce the incidence of purpura with devices that are prone to purpura formation.54
Rarely, urticaria may be seen with lasers (Figure 28-16).55 This may be treated with cold compresses and an oral antihistamine (e.g., cetirizine 10 mg), which may be continued daily until resolved. Once identified, these patients may be pretreated for subsequent treatments with an antihistamine 1 hour prior to procedure.
Pigmentary complications of hyperpigmentation and hypopigmentation are rare, but may be seen in darker Fitzpatrick skin types (IV through VI) and patients with a recent tan. These complications are more common with devices that utilize short wavelengths (e.g., 532 nm and pulsed dye lasers) and with laser parameters of short pulse widths and/or high fluences. Inadequate epidermal cooling as well as overly aggressive cooling can also result in pigmentary changes. Hyperpigmentation is usually transient (and rarely may be permanent), lasting on the order of months. Postinflammatory hyperpigmentation has been reported with nonablative fractional devices56,57 and has been observed as a result of epidermal injury due to overcooling by the cryogen sprays used with some infrared devices.58 If PIH occurs, patients may use a topical lightening agent such as hydroquinone (4 to 8%) twice daily along with an exfoliating product (such as lactic or glycolic acid) and/or a retinoid. (See Chapter 24, Skin Care Products, for more about treatment of PIH.) The use of a lightening agent for 1 month prior to treatment may reduce the risk of PIH, particularly in darker Fitzpatrick skin types. Hypopigmentation is a more significant complication and, although often temporary, may be permanent.
A burn and/or scar may also occur, particularly with devices that utilize short wavelengths (e.g., 532 nm and pulsed dye lasers),59,60 aggressive treatment parameters of short pulse widths, and high fluences or inadequate epidermal cooling. In addition, overtreatment can occur when treating above bony prominences because these areas are more prone to the buildup of heat, particularly with the lasers for skin laxity. Routine moist wound care should be used for these complications with application of an antibiotic ointment and bandage until healed. Tattoos and permanent make-up have concentrated ink pigments and treatment over these may result in a full-thickness skin burn.
Herpes simplex and varicella zoster may be reactivated in the treatment area. Pretreatment prophylaxis with an oral antiviral medication can reduce this risk (see the Procedure Preparation section earlier in this chapter).
Alteration to dermal filler is controversial. Although some evidence suggests that lasers do not affect dermal fillers in tissue,61 other studies recommend using lasers as a treatment for undesired collections of dermal fillers to render them more moldable and reduce their appearance in the skin.62,63 The author does treat over facial areas with fillers using nonablative lasers but not with ablative lasers.
Current Developments
Combination therapy utilizing nonablative lasers with other minimally invasive aesthetic procedures in the same visit is emerging as a new approach to skin rejuvenation64 (see Chapter 31, Combination Cosmetic Treatments). For example, the author combines a Q-switched 1064 nm nonablative laser treatment for dermal collagen remodeling, with superficial exfoliating procedures such as microdermabrasion and superficial chemical peels, on the same day to enhance wrinkle reduction results without increasing downtime or side effects.
Recent technological improvements in Q-switched devices, such as flat-topped beam profiles, have reduced tissue “hot spots” and the associated risk of petechiae. In addition, novel pulsing modes (e.g., photoacoustic technology pulse) have been developed that allow for greater peak power without additional patient discomfort.23
Fractional delivery of energy is a very promising new method of nonablative laser treatments. In addition to reduction of wrinkles and improvements in dyschromia, fractional 1550 nm skin resurfacing treatments have also demonstrated good success with scar reduction.12,65,66 Modifications to some of the newer 1550 nm fractional devices may reduce the incidence of postinflammatory hyperpigmentation.8
Newer approaches to reduction of skin laxity combine monopolar with bipolar radio-frequency, where the RF current travels more superficially in the skin.67 Some devices combine radio-frequency with light-based technologies for nonablative skin rejuvenation (termed ELOS™, electro-optical synergy).68
Photomodulation with LEDs is a relatively new, non–thermally mediated method of mild skin rejuvenation. Studies have yet to determine which pulsing modes are most efficacious and compare the different wavelengths. Combining LEDs, or other nonablative laser and light-based modalities, with photosensitizing medications for photodynamic therapy enhances rejuvenation results.36,69 Combination therapy with PDT and exfoliation treatments, such as microdermabrasion, to enhance penetration of photosensitizing medications may further improve results.70
Financial Considerations
Nonablative laser treatments for wrinkles are not reimbursable by insurance companies. The charges for treatments vary, and are largely determined by local prices. Individual treatment prices range from $200 to $500 for a single treatment to a large area such as the face, and $150 to $300 for a small area such as the neck. However, because wrinkle reduction treatments are most effective with a series of treatments, packages of treatments (usually six) may be offered so that patients achieve the best possible results. Box 28-1 lists the applicable ICD-9 codes.
1. Liu H, Dang Y, Wang Z, et al. Laser induced collagen remodeling: a comparative study in vivo on mouse model. Lasers Surg Med. 2008;40(1):13-19.
2. Goldberg DJ. Nonablative resurfacing. Clin Plast Surg. 2000;27(2):287-292. xi
3. Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524-527.
4. Lloyd JR. Effect of fluence on efficacy using the 1440 nm laser with CAP technology for the treatment of rhytids. Lasers Surg Med. 2008;40(6):387-389.
5. Goldberg DJ. Full-face nonablative dermal remodeling with a 1320 nm Nd:YAG laser. Dermatol Surg. 2000;26(10):915-918.
6. Fournier N, Dahan S, Barneon G, et al. Nonablative remodeling: a 14-month clinical ultrasound imaging and profilometric evaluation of a 1540 nm Er:glass laser. Dermatol Surg. 2002;28(10):926-931.
7. Paithankar DY, Clifford JM, Saleh BA, et al. Subsurface skin renewal by treatment with a 1450-nm laser in combination with dynamic cooling. J Biomed Opt. 2003;8(3):545-551.
8. Narurkar VA. Nonablative fractional resurfacing for total body rejuvenation. J Drugs Dermatol. 2008;7(4):352-355.
9. Manstein D, Herron GS, Sink RK. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers Surg Med. 2004;34:426-438.
10. Rahman Z, Alam M, Dover JS. Fractional laser treatment for pigmentation and texture improvement. Skin Therapy Lett. 2006;11(9):7-11.
11. Tannous Z. Fractional resurfacing. Clin Dermatol. 2007;25(5):480-486.
12. Tierney EP, Kouba DJ, Hanke CW. Review of fractional photothermolysis: treatment indications and efficacy. Dermatol Surg. 2009;35(10):1445-1461.
13. Zelickson BD, Kilmer SL, Bernstein E, et al. Pulsed dye laser therapy for sun damaged skin. Lasers Surg Med. 1999;25(3):229-236.
14. Goldberg DJ. New collagen formation after dermal remodeling with an intense pulsed light source. J Cutan Laser Ther. 2000;2(2):59-61.
15. Carniol PJ, Farley S, Friedman A. Long-pulse 532-nm diode laser for nonablative facial skin rejuvenation. Arch Facial Plast Surg. 2003;5(6):511-513.
16. Dayan SH, Vartanian AJ, Menaker G, et al. Nonablative laser resurfacing using the long-pulse (1064-nm) Nd:YAG laser. Arch Facial Plast Surg. 2003;5(4):310-315.
17. Dayan S, Damrose JF, Bhattacharyya TK, et al. Histological evaluations following 1,064-nm Nd:YAG laser resurfacing. Lasers Surg Med. 2003;33(2):126-131.
18. Lee MW. Combination visible and infrared lasers for skin rejuvenation. Semin Cutan Med Surg. 2002;21(4):288-300.
19. Goldberg DJ, Silapunt S. Histologic evaluation of a Q-switched Nd:YAG laser in the nonablative treatment of wrinkles. Dermatol Surg. 2001;27(8):744-746.
20. Cisneros JL, Rio R, Palou J. The Q-switched neodymium (Nd):YAG laser with quadruple frequency. Clinical histological evaluation of facial resurfacing using different wavelengths. Dermatol Surg. 1998;24(3):345-350.
21. Lee MC, Hu S, Chen MC, et al. Skin rejuvenation with 1,064-nm Q-switched Nd:YAG laser in Asian patients. Dermatol Surg. 2009;35(6):929-932.
22. Goldberg DJ, Silapunt S. Q-switched Nd:YAG laser: rhytid improvement by non-ablative dermal remodeling. J Cutan Laser Ther. 2000;2(3):157-160.
23. Berlin AL, Dudelzak J, Hussain M, et al. Evaluation of clinical, microscopic, and ultrastructural changes after treatment with a novel Q-switched Nd:YAG laser. J Cosmet Laser Ther. 2008;10(2):76-79.
24. Friedman PM, Jih MH, Skover GR, et al. Treatment of atrophic facial acne scars with the 1064-nm Q-switched Nd:YAG laser: six-month follow-up study. Arch Dermatol. 2004;140(11):1337-1341.
25. Yaghmai D, Garden JM, Bakus AD, et al. Photodamage therapy using an electro-optic Q-switched Nd:YAG laser. Lasers Surg Med. 2009;42(8):699-705.
26. Kilmer SL, Lee MS, Grevelink JM, et al. The Q-switched Nd:YAG laser effectively treats tattoos. A controlled, dose-response study. Arch Dermatol. 1993;129(8):971-978.
27. Cho SB, Kim JS, Kim MJ. Melasma treatment in Korean women using a 1064-nm Q-switched Nd:YAG laser with low pulse energy. Clin Exp Dermatol. 2009;34(8):e847-850.
28. Cho SB, Park SJ, Kim JS, et al. Treatment of post-inflammatory hyperpigmentation using 1064-nm Q-switched Nd:YAG laser with low fluence: report of three cases. J Eur Dermatol Venereol. 2009;23(10):1206-1207.
29. Anderson RR, Margolis RJ, Watenabe S, et al. Selective photothermolysis of cutaneous pigmentation by Q-switched Nd:YAG laser pulses at 1064, 532, and 355 nm. J Invest Dermatol. 1989;93(1):28-32.
30. Bakus AD, Garden JM, Yaghmai D, Massa MC. Long-term fine caliber hair removal with an electro-optic Q-switched Nd:YAG laser. Laser Surg Med. 2010;42(8):706-711.
31. Weiss RA, McDaniel DH, Geronemus RG, et al. Clinical experience with light-emitting diode (LED) photomodulation. Dermatol Surg. 2005;31(9 Pt 2):1199-1205.
32. Goldberg DJ, Amin S, Russell BA, et al. Combined 633-nm and 830-nm LED treatment of photoaging skin. J Drugs Dermatol. 2006;5(8):748-753.
33. Kennedy JC, Pottier RH, Pross DC. Photodynamic therapy with endogenous protoporphyrin IX: basic principles and present clinical experience. J Photochem Photobiol B. 1990;6(1–2):143-148.
34. Dover JS, Bhatia AC, Stewart B, et al. Topical 5-aminolevulinic acid combined with intense pulsed light in the treatment of photoaging. Arch Dermatol. 2005;141(10):1247-1252.
35. Uebelhoer NS, Dover JS. Photodynamic therapy for cosmetic applications. Dermatol Ther. 2005;18(3):242-252.
36. Alster TS, Tanzi EL, Welsh EC. Photorejuvenation of facial skin with topical 20% 5-aminolevulinic acid and intense pulsed light treatment: a split-face comparison study. J Drugs Dermatol. 2005;4(1):35-38.
37. Bjerring P, Christiansen K, Troilius A, et al. Skin fluorescence controlled photodynamic photorejuvenation (wrinkle reduction). Lasers Surg Med. 2009;41(5):327-336.
38. Kaufman J. Lasers and light devices. In: Baumann L, editor. Cosmetic Dermatology. New York: McGraw-Hill; 2009:212-220.
39. Dierickx CC. The role of deep heating for noninvasive skin rejuvenation. Lasers Surg Med. 2006;38(9):799-807.
40. Carniol PJ, Dzopa N, Fernandes N, et al. Facial skin tightening with an 1100–1800 nm infrared device. J Cosmet Laser Ther. 2008;10(2):67-71.
41. Goldberg DJ, Hussain M, Fazeli A, et al. Treatment of skin laxity of the lower face and neck in older individuals with a broad-spectrum infrared light device. J Cosmet Laser Ther. 2007;9(1):35-40.
42. Chan HH, Yu CS, Shek S, et al. A prospective, split face, single-blinded study looking at the use of an infrared device with contact cooling in the treatment of skin laxity in Asians. Lasers Surg Med. 2008;40(2):146-152.
43. Sukal SA, Geronemus RG. Thermage: the nonablative radiofrequency for rejuvenation. Clin Dermatol. 2008;26(6):602-607.
44. Sadick NS, Makino Y. Selective electro-thermolysis in aesthetic medicine: a review. Lasers Surg Med. 2004;34(2):91-97.
45. Alam M, Dover JS. Nonablative laser and light therapy: an approach to patient and device selection. Skin Therapy Lett. 2003;8(4):4-7.
46. Manuskiatti W, Wachirakaphan C, Lektrakul N, et al. Circumference reduction and cellulite treatment with a TriPollar radiofrequency device: a pilot study. J Eur Dermatol Venereol. 2009;23(7):820-827.
47. Dover JS, Zelickson B. Results of a survey of 5,700 patient monopolar radiofrequency facial skin tightening treatments: assessment of a low-energy multiple-pass technique leading to a clinical end point algorithm. Dermatol Surg. 2007;33(8):900-907.
48. Branson DF. Dermal undermining (scarification) of active rhytids and scars: enhancing the results of CO(2) laser skin resurfacing. Aesth Surg J. 1998;18(1):36-37.
49. Goldberg DJ, Whitworth J. Laser skin resurfacing with the Q-switched Nd:YAG laser. Dermatol Surg. 1997;23(10):903-906.
50. Chernoff WG. Nonexfoliating laser rejuvenation of facial rhytids. In: Keller GS, Lacombe VG, Lee PK, Watson JP, editors. Lasers in Aesthetic Surgery. New York: Thieme; 2001:139-148.
51. Zelickson B, Ross EV, Strasswimmer J. Definition and proposed mechanisms of non-invasive skin tightening. In: Alam M, Dover J, editors. Non-Surgical Skin Tightening and Lifting. Philadelphia: Elsevier; 2009:3-7.
52. Goldberg DJ. Non-ablative subsurface remodeling: clinical and histologic evaluation of a 1320-nm Nd:YAG laser. J Cutan Laser Ther. 1999;1(3):153-157.
53. Travelute AC, Carniol PJ, Hruza GJ. Laser treatment of facial vascular lesions. Facial Plast Surg. 2001;17(3):193-201.
54. Galeckas KJ, Ross EV, Uebelhoer NS. A pulsed dye laser with a 10-mm beam diameter and a pigmented lesion window for purpura-free photorejuvenation. Dermatol Surg. 2008;34(3):308-313.
55. England R. Immediate cutaneous hypersensitivity after treatment of tattoo with Nd:YAG laser: a case report and review of the literature. Ann Allergy Asthma Immunol. 2002;89:215-217.
56. Chan HH, Manstein D, Yu CS, et al. The prevalence and risk factors of post-inflammatory hyperpigmentation after fractional resurfacing in Asians. Lasers Surg Med. 2007;39(5):381-385.
57. Fisher GH, Geronemus RG. Short-term side effects of fractional photothermolysis. Dermatol Surg. 2005;31(9 Pt 2):1245-1249.
58. Lee SJ, Park SG, Kang JM, et al. Cryogen-induced arcuate shaped hyperpigmentation by dynamic cooling device. J Eur Dermatol Venereol. 2008;22(7):883-884.
59. Gaston DA, Clark DP. Facial hypertrophic scarring from pulsed dye laser. Dermatol Surg. 1998;24(5):523-525.
60. Wlotzke U, Hohenleutner U, bd-El-Raheem TA, et al. Side-effects and complications of flashlamp-pumped pulsed dye laser therapy of port-wine stains. A prospective study. Br J Dermatol. 1996;134(3):475-480.
61. Shumaker PR, England LJ, Dover JS, et al. Effect of monopolar radiofrequency treatment over soft-tissue fillers in an animal model: part 2. Lasers Surg Med. 2006;38(3):211-217.
62. Lemperle G, Rullan PP, Gauthier-Hazan N. Avoiding and treating dermal filler complications. Plast Reconstr Surg. 2006;118(3 Suppl):92S-107S.
63. Hirsch RJ, Narurkar V, Carruthers J. Management of injected hyaluronic acid induced Tyndall effects. Lasers Surg Med. 2006;38(3):202-204.
64. Effron C, Briden ME, Green BA. Enhancing cosmetic outcomes by combining superficial glycolic acid (alpha-hydroxy acid) peels with nonablative lasers, intense pulsed light, and trichloroacetic acid peels. Cutis. 2007;79(1 Suppl Combining):4-8.
65. Alster TS, Tanzi EL, Lazarus M. The use of fractional laser photothermolysis for the treatment of atrophic scars. Dermatol Surg. 2007;33(3):295-299.
66. Behroozan DS, Goldberg LH, Dai T, et al. Fractional photothermolysis for the treatment of surgical scars: a case report. J Cosmet Laser Ther. 2006;8(1):35-38.
67. Mayoral FA. Skin tightening with a combined unipolar and bipolar radiofrequency device. J Drugs Dermatol. 2007;6(2):212-215.
68. Hammes S, Greve B, Raulin C. Electro-optical synergy (ELOS) technology for nonablative skin rejuvenation: a preliminary prospective study. J Eur Dermatol Venereol. 2006;20(9):1070-1075.
69. Gold MH, Bradshaw VL, Boring MM, et al. Split-face comparison of photodynamic therapy with 5-aminolevulinic acid and intense pulsed light versus intense pulsed light alone for photodamage. Dermatol Surg. 2006;32(6):795-801.
70. Nootheti PK, Gold MH, Goldman MP. Photodynamic therapy for photorejuvenation. In: Goldman MP, editor. Photodynamic Therapy. Philadelphia: Saunders/Elsevier; 2008:125-135.
Costello G. Lasers and pulsed-light devices: skin tightening (Chap 51). In Pfenninger JL, Fowler GC, editors: Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed, Philadelphia: Mosby/Elsevier, 2011.
Small R. Non-ablative modalities for wrinkles. In: Small R, editor. A Practical Guide to Cosmetic Lasers. Philadelphia: Lippincott, 2012.
Stampar M. Non-ablative radiowave skin tightening (Chap 52). In Pfenninger JL, Fowler GC, editors: Pfenninger and Fowler’s Procedures for Primary Care, 3rd ed, Philadelphia: Mosby/Elsevier, 2011.





 % two times per day for 3 to 4 days or until redness resolves. Patients are instructed to contact their provider if erythema persists for more than 5 days because postinflammatory hyperpigmentation (PIH) can occur with prolonged erythema (see complications below). Patients should avoid direct sun exposure for 1 to 2 days after treatment to help minimize the risk of pigmentary changes and use a broad-spectrum sunscreen (SPF 30 with zinc or titanium) daily.
% two times per day for 3 to 4 days or until redness resolves. Patients are instructed to contact their provider if erythema persists for more than 5 days because postinflammatory hyperpigmentation (PIH) can occur with prolonged erythema (see complications below). Patients should avoid direct sun exposure for 1 to 2 days after treatment to help minimize the risk of pigmentary changes and use a broad-spectrum sunscreen (SPF 30 with zinc or titanium) daily.




