CHAPTER 13 Wound local anesthetic infusions
Crile, a surgeon from Cleveland, USA, was the first to describe, in 1913, the benefit of local anesthesia application to the surgical wound in providing analgesia and decreasing morbidity and mortality. Capelle, in 1935, described the use of an infusion apparatus to deliver local anesthesia to the wound.1 In 1950, Blades and Ford used a fine catheter to deliver local anesthetic to thoracotomy wounds.
Over the past 20 years, numerous papers have reported the use of local anesthesia in wounds of major abdominal incisions, gynecological and obstetric procedures, orthopedic operations, plastics procedures and mastectomy, among others. These studies have confirmed a decrease in pain scores at rest and during activity. They have, in addition, been associated with a decreased incidence of side-effects.2
Rationale for using local anesthetic infusion
Postoperative pain arises from the interaction of three factors:
Local anesthetics can be used peri-operatively to affect all three of the above.4 In addition, because these systems are relatively simple to use they can and have been used in the home setting postoperatively.5
Potential problems
It would appear that local anesthetic infusions have very few side-effects and as a result their risk–benefit ratio is positive.2
Positioning
The fact that surgeons place catheters has the added advantage of making them more aware of postoperative pain and empowering them to assist its palliation. Postoperative pain has up to recently not been seen as a complication in surgical terms. The incidence of post-surgical chronic pain is higher than many surgeons appear to realize.6
Orthopedic procedures
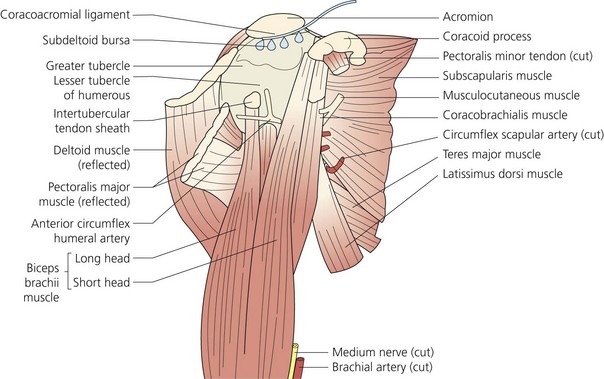
Shoulder surgery
Arthroscopic surgery
Wound catheter techniques decrease opioid requirements without significant side-effects.
Subacromial catheter placement is recommended (Fig. 13.1) but intra-articular catheters have also been used. A flow rate of 2–5 mL/hr is adequate.
Joint surgery
Total knee replacement
More recently, a high dose local infiltration technique has been described. This combines the use of local anesthetics together with an anti-inflammatory agent and adrenaline in the tissues around the wound and also the use of an intra-articular catheter.7
Abdominal surgery
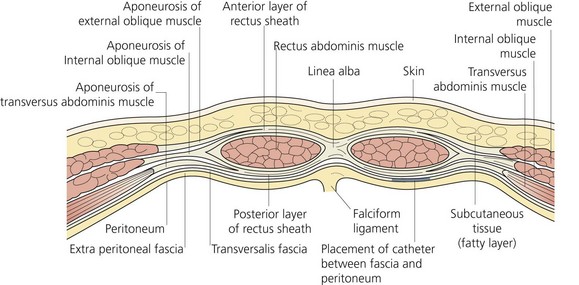
Laparotomy with mid-line incision8
This is a common surgery and is associated with severe postoperative pain, especially if the wound is above the umbilicus. Incisions below the umbilicus tend to be less painful. Nevertheless, the incisions for open laparotomy can be long, and therefore a fenestrated catheter is recommended. It would appear that subfascial placement is more effective than subcutaneous (Fig. 13.2).9 The length of catheter can be adjusted for the size of the incision. A bolus is suggested prior to infusion.
Laparoscopic cholecystectomy
The current recommended technique for this surgery is the use of a 20-mL bolus in the gallbladder bed and in the trocar sites, followed by intermittent 10-mL boluses intraperitoneally. An epidural catheter is sufficient here. Infusions do not appear to add any benefit.10
Breast surgery
Postoperative use of continuous indwelling catheters has been shown to be of benefit in many types of breast surgery, including mastectomy, plastic/cosmetic procedures and axillary clearance.11
A study placing the catheter parallel and inferior to the axillary vein has been shown to be effective for axillary surgery.12
The use of a bolus injection prior to infusion of c.4 mL/hr for 48 hours is also recommended.
Cardiothoracic surgery
Current evidence suggests that the use of two fenestrated catheters, one placed in the subfascial plane above the sternum and the other subcutaneous in the wound, is effective in reducing pain at rest, and opioid consumption.13
Flow rates of 2 mL/hr in each catheter are recommended for at least 48 hours.
Gynecological/obstetrical surgery
Cesarian section
Cesarian section through a Pfannenstiel incision is associated with less postoperative pain when local anesthetic is perfused via a fenestrated catheter placed either above or below the fascia.14 The optimal position is as yet undetermined. Diclofenac alone infused to the wound was found to be superior to intravenous diclofenac.15
Infusion rates of 4–6 mL/hr should suffice unless the wound is very wide.
This technique is especially beneficial in these patients, as early mobilization is preferable.
Abdominal hysterectomy
This procedure has also been shown to be associated with less postoperative pain and decreased opioid consumption when a wound infusion of local anesthesia has been used.16 Placement of the catheter above the fascia has been more effective than below the fascia, which is at variance with other abdominal surgeries when subfascial placement of the catheter has been more effective. Further studies will confirm the optimal catheter position.
Equipment
The basic system is a pump (Figs 13.3 and 13.4) and a catheter. Sterile equipment and aseptic technique are essential to minimize the risk of infection.
Drugs
There is some concern over possible cytotoxic effects of local anesthetics on articular chondrocytes or osteoblasts; however, this needs further evaluation.17
1 Capelle W. Die Bedentung des Wundschmerzes und seiner Ausschaltung fur dan Ablauf der Atmung bei Laparotomierte. Dtsch Z Chir. 1935;246:466.
2 Liu SS, Richman JM, Thirlby RC, Wu CL. Efficacy of continuous wound catheters delivering local anaesthetic for post operative analgesia: a quantitative and qualitative systematic review of randomised controlled trials. J Am Coll Surg. 2006;203:914-932.
3 Kehlet H, Jensen TS, Woolf CJ. Persistent post surgical pain: risk factors and prevention. Lancet. 2006;367:1618-1625.
4 Strichartz GR. Novel ideas of local anaesthetic actions on various ion channels to ameliorate post operative pain. BJA. 2008;101(1):45-47.
5 Rawal N, Axellson K, Hylander J, et al. Postoperative patient-controlled local anaesthetic administration at home. Anaesth Analg. 1998;86:86-89.
6 McRae WA. British Journal of Anaesthesia. 2001;87(1):88-98.
7 Röstlund T, Kehlet H. High dose local infiltration analgesia after hip and knee replacement-what is it, why does it work and what are the future challenges? Acta Orthop. 2007;78:159-161.
8 Beaussier M, E’Ayoubi H, Schiffer E, et al. Continuous preperitoneal infusion of robivicaine provides effective analgesia and accelerates recovery after colorectal surgery. A randomised double-blind, placebo-controlled study. Anaesthesiology. 2007;107:155-159.
9 Fredman B, Zohar E, Tarabyk A, et al. Bupivicaine wound installation via an electronic patient-controlled device and a double catheter system does not decrease postoperative pain or opioid requirement after major abdominal surgery. Anaesth Analg. 2001;92:189-193.
10 Gupta A, Thöm S, Axelsson K, et al. Postoperative pain relief using intermittent injections of 0.5% ropivacaine through a catheter after laparoscopic cholecystectomy. Anaesth Analg. 2002;95:450-456.
11 Rawal N, Gupta A, Helsing M, et al. Pain relief following breast augmentation surgery: a comparison between incisional patient-controlled regional analgesia and traditional oral analgesia. Eur J Anaesthesiol. 2006;23:1010-1017.
12 Schell SR. Patient outcomes after axillary node dissection for breast cancer: use of postoperative continuous local anaesthesia infusion. J Surg Res. 2006;134:124-132.
13 Dowling R, Theilmeier K, Ghaly A, et al. Improved pain control after cardiac surgery: Results of a randomised double blind clinical trial. J Thorac Cardiovasc Surg. 2003;26:127-128.
14 Ranta PO, Ala-Koko TI, Kukkonen JE, et al. Incisional and epidural analgesia after caesarian delivery: a prospective, placebo-controlled, randomised clinical study. Int J Obstetric Analgesia. 2006;15:189-194.
15 Lavand’homme PM, Roelants F, Waterloos H, de Kock MF. Postoperative pain analgesic effects of continuous wound infiltration with diclofenac after elective Caesarian delivery. Anaesthesiology. 2007;106:220-225.
16 Gupta S, Maheshwari R, Dulara SC. Wound instillation of 0.25% bupivacaine as continuous infusion following hysterectomy. Middle East J Anaesth. 2005;18:595-610.
17 Karpi JC, Chu CR. Lidocaine exhibits dose-and time-dependent cytotoxic effects on bovine articular chondrocyes in vitro. Am J Sports Med. 2007;35:1621-1634.