Chapter 12 Wolff-Parkinson-White Preexcitation Patterns
Wolff-Parkinson-White Pattern: Preexcitation and Bypass Tracts
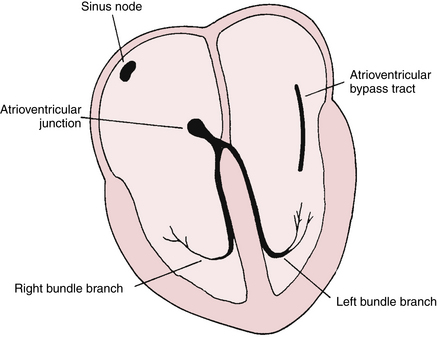
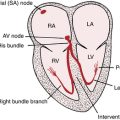
The WPW pattern is a distinctive and important ECG abnormality caused by preexcitation of the ventricles. Normally the electrical stimulus travels to the ventricles from the atria via the atrioventricular (AV) junction. The physiologic lag of conduction through the AV junction results in the normal PR interval of 0.12 to 0.2 sec. Consider the consequences of having an extra pathway between the atria and ventricles that would bypass the AV junction and preexcite the ventricles. This situation is exactly what occurs with the WPW pattern: an atrioventricular bypass tract connects the atria and ventricles, circumventing the AV junction (Fig. 12-1).
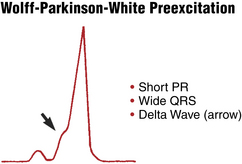
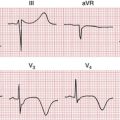
Preexcitation of the ventricles with the classic WPW pattern produces the following characteristic triad of findings on the ECG (Figs. 12-2 to 12-4):
1. The QRS complex is widened, giving the superficial appearance of a bundle branch block pattern. However, the wide QRS is caused not by a delay in ventricular depolarization but by early stimulation of the ventricles. The T wave is also usually opposite in polarity to the wide QRS in any lead, similar to what is seen with bundle branch blocks (“secondary T wave inversions”).
2. The PR interval is shortened (often but not always to less than 0.12 sec) because of the ventricular preexcitation.
3. The upstroke of the QRS complex is slurred or notched. This is called a delta wave.
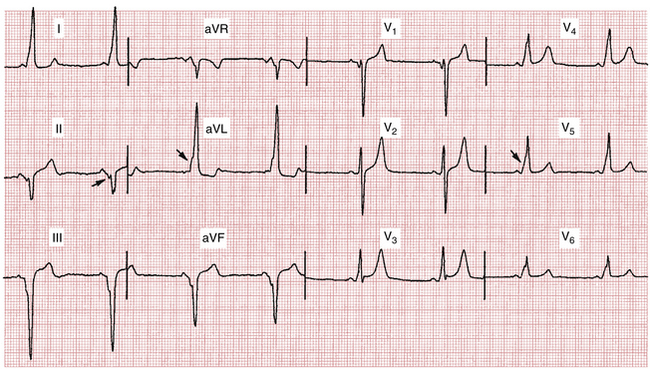
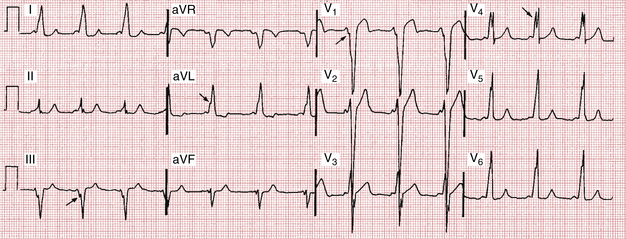
Figures 12-2 and 12-3 show the WPW pattern, with its classic triad of a widened QRS complex , a short PR interval, and a delta wave. Notice that the pattern superficially resembles a bundle branch block pattern because of the widened QRS complexes.
If the bypass tract hooks into the posterior region of the ventricles, the ECG usually shows positive delta waves in most of the precordial leads and negative delta waves in the inferior limb leads (resembling an inferoposterior infarct; see Fig. 12-3).
With right free wall preexcitation, the QRS complexes are predominantly negative in V1 and V2, resembling a left bundle branch block (LBBB). The delta waves are typically byphasic or slightly positive in V1/V2 and positive in V6 (Fig. 12-4). The QRS axis is horizontal or leftward.
Anteroseptal bypass tracts, the rarest WPW variant, may be associated with negative delta waves in leads V1 and V2 (resembling an anteroseptal infarct). The frontal plane axis is more vertical.
Clinical Significance
The major significance of WPW preexcitation is twofold:
1. Individuals with this pattern are prone to arrhythmias, especially paroxysmal supraventricular tachycardia (PSVT) (see Fig. 12-4) and atrial fibrillation. In the latter instance, if the rate becomes extremely fast, atrial fibrillation may lead to ventricular fibrillation with sudden cardiac arrest. Fortunately, this occurrence is very rare. These important topics, introduced briefly in this chapter, are discussed further in Chapters 14 and 20.
2. The WPW ECG is often mistaken for either a bundle branch block, due to the wide QRS, or for an MI, due to the negative delta waves simulating pathologic Q waves (see Fig. 12-3).
The WPW abnormality predisposes patients to develop PSVT because of the presence of the extra conduction pathway. For example, a premature impulse traveling down the AV junction may recycle up the accessory pathway and then back down the AV junction, and so on. This type of recirculating impulse is an example of reentry. The important topic of reentry and PSVT is discussed further in Chapter 14.
When PSVT develops in a patient with the WPW preexcitation pattern, the QRS complex generally becomes narrow (Fig. 12-5). The widened QRS seen with WPW syndrome during normal sinus rhythm occurs because the stimulus travels concomitantly down the bypass tract and down the AV junction, resulting in a type of hybrid or fusion beat. When PSVT occurs, the impulse usually travels down the AV junction and back up the bypass tract in a retrograde fashion, resulting in a loss of the delta wave. (The delta wave and wide QRS will only be seen when an impulse travels down the bypass tract.)
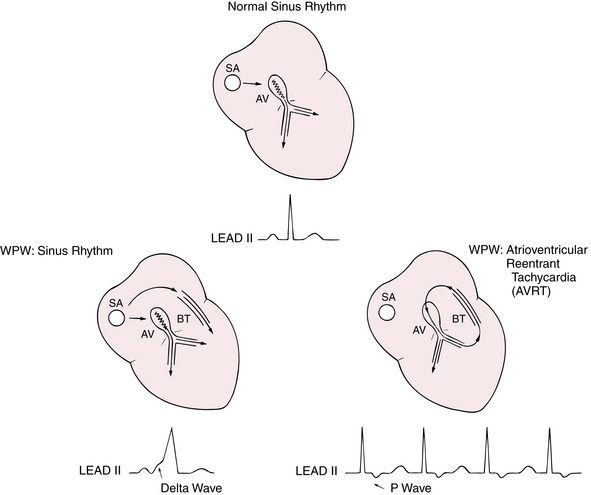
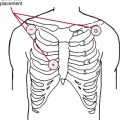
Figure 12-5 Conduction during sinus rhythm in the normal heart (top) spreads from the sinoatrial (SA) node to the atrioventricular (AV) node and then down the bundle branches. The jagged line indicates physiologic slowing of conduction in the AV node. With the Wolff-Parkinson-White (WPW) syndrome (bottom left), an abnormal accessory conduction pathway called a bypass tract (BT) connects the atria and ventricles. With WPW, during sinus rhythm the electrical impulse is conducted quickly down the bypass tract, preexciting the ventricles before the impulse arrives via the AV node. Consequently, the PR interval is short and the QRS complex is wide, with slurring at its onset (delta wave). WPW predisposes patients to develop an atrioventricular reentrant tachycardia (AVRT) (bottom right) in which a premature atrial beat may spread down the normal pathway to the ventricles, travel back up the bypass tract, and recirculate down the AV node again. This reentrant loop can repeat itself over and over, resulting in a tachycardia. Notice the normal QRS complex and often negative P wave in lead II during this type of bypass-tract tachycardia (see Chapter 14).
Of note, some patients with bypass tracts do not show the classic WPW pattern during sinus rhythm but may develop reentrant types of PSVT. These patterns associated with a concealed bypass tract are described in Chapter 14.
Another rare preexcitation variant is related to a slowly conducting bypass tract that typically connects the right atrium with the right bundle branch or right ventricle. These “atriofascicular” or “atrioventricular” fibers are sometimes referred to as Mahaim fibers. The 12-lead ECG in sinus rhythm may be normal or may show a normal PR interval with a subtle delta wave. If PSVT develops, the impulse goes down the bypass tract, stimulates the right ventricle before the left, and then reenters up the AV node. This sequence will produce an LBBB pattern during the tachycardia.
Treatment
Not all individuals with the WPW pattern have associated arrhythmias. Occasionally, the WPW pattern will be discovered in asymptomatic subjects who have an ECG ordered as part of a routine examination or for other indications. The major concern is the risk of the sudden onset of atrial fibrillation leading to ventricular fibrillation. Fortunately, the risk of sudden death from this mechanism is extremely low in completely asymptomatic subjects with the WPW patterns. Individuals in whom a WPW pattern is discovered as an incidental finding, therefore, usually do not require specific intervention. Disappearance of the WPW pattern during exercise (with the appearance of a normal QRS with sinus tachycardia) is particularly reassuring. Electrophysiologic evaluation and prophylactic ablation therapy in asymptomatic subjects are sometimes considered in special circumstances, for example, with competitive athletes, pilots, and those with a family history of sudden death.
Overview: Differential Diagnosis of Wide QRS Complex Patterns
1. Bundle branch blocks (intrinsic conduction delays) including the classic RBBB and LBBB patterns
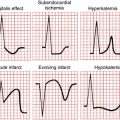
2. “Toxic” conduction delays caused by some extrinsic factor, such as hyperkalemia or drugs (e.g., quinidine, propafenone, flecainide and other related antiarrhythmics, as well as phenothiazines, and tricyclic antidepressants)
3. Beats arising in the ventricles, which may be ventricular escape beats or ventricular premature beats (Chapter 16), or electronic ventricular pacemaker beats (Chapters 7 and 21)
Differentiation among these four possibilities is usually straightforward. The ECG effects of RBBB and LBBB have already been described in Chapter 7. Hyperkalemia produces widening of the QRS complex, often with loss of P waves (Chapter 12). Widening of the QRS complex in any patient who is taking an antiarrhythmic or a psychotropic agent should always suggest possible drug toxicity. Pacemakers generally produce an LBBB pattern with a pacemaker spike before each QRS complex. (An important exception is biventricular pacing used in the treatment of chronic heart failure (CHF) in which an RBBB pattern is usually seen in conjunction with the left ventricular component of pacing; see Chapter 21.) The WPW pattern is recognized by the triad of a short PR interval, a wide QRS complex, and a delta wave, as discussed in this chapter.