Chapter 103 Wilderness and Endurance Events
Perhaps the earliest record of an endurance event may be traced back to ancient Greece in the 5th century BC. The Persians invaded Greece in 490 BC, landing in Marathon, a small town about 26 miles from Athens. Seriously outnumbered by the Persians, the Athenians sent messengers to cities throughout Greece requesting assistance. Legend has it that after the battle, a man named Pheidippides was sent from Marathon to Athens to bring word of the Greek victory. He covered the 26-plus miles on foot, only to drop dead after proclaiming “Niki!” (Victory). Debate continues among historians about what really occurred. For instance, there is evidence that Pheidippides was actually sent from Marathon to request help and that news of the victory was delivered by a man named Eukles.16 Although the exact details remain unclear, when the modern-day Olympic games were inaugurated in Greece in 1896, the legend of Pheidippides served as inspiration for the marathon. That first marathon covered a distance of 40 km (24.85 miles), the distance from Marathon Bridge to Olympic Stadium.47
During the next 28 years, the marathon continued to evolve. In the United States, the Boston Athletic Association held its first marathon on April 19, 1897, to commemorate the famous ride of Paul Revere on that date in 1775. For the Olympic Games in London in 1908, the marathon distance was changed to 26 miles, the distance from Windsor Castle to White City Stadium, with an additional 385 yards added so that the race would finish in front of the royal family’s viewing box. Finally, in the 1924 Olympic Games in Paris, the distance was set at 26.2 miles, establishing the modern-day marathon distance.47 Today, there are hundreds of marathons held throughout the world each year.
Types of Events
Adventure Races
Adventure racing, as we know it today, began in the early 1980s with the first large, well-organized events, including the Coast-to-Coast, started in New Zealand in 1980, and the Alaska Wilderness Classic, started in 1983. These were followed by other well-known events, including New Zealand’s Raid Gauloises and the Southern Traverse, begun in 1989 and 1991, respectively. The Eco-Challenge introduced adventure racing to the United States in 1995. The Primal Quest, started in 2002 in Telluride, Colorado, brought adventure racing more into the mainstream of American sports through network television coverage. In addition to these expedition-length races, there are countless shorter races throughout the world. In the United States, the U.S. Adventure Race Association (USARA) serves as the governing body for adventure racing (http://www.usara.com).
Cycling
USA Cycling, the governing body for mountain biking in the United States, sanctioned more than 50 mountain bike events in 2010 (http://www.usacycling.org); however, this represents only a small fraction of the events held annually.
Marathons
Marathons are perhaps the most popular endurance events. Standard marathons cover 26.2 miles (42 km), whereas ultra-marathons may be 100 miles (160 km) or more. In 2008, there were an estimated 445 marathons held in the United States, with approximately 425,000 finishers (http://www.runningusa.org). In 2010, there were 80 ultra-marathons scheduled in North America, with an estimated 3790 finishers through July 2010 (http://www.run100s.com).
USA Track and Field (USATF; http://www.usatf.org) is the national governing body of long-distance running and is a member of the International Association of Athletics Federations (IAAF; http://www.iffa.org), which sets the rules of competition for all officially sanctioned long-distance running events in the United States and throughout the world. However, the vast majority of marathons in the United States are non-USATF events. Only 73 of the 445 marathons held in the United States in 2008 were certified by the USATF (http://www.runningusa.org/node/16585).
USATF rules of competition allow for sanctioned medical assistance for participants by authorized official event personnel. Current rules do not stipulate specific penalties or disqualification for acceptance of medical assistance, as long as it does not alter the scheduled time of competition for any athlete, interfere with other athletes in the competition, or incorporate the use of illegal or banned substances, technology, or devices that may give the athlete an unfair competitive advantage. A medical official may choose to remove an athlete from competition if the official feels it is medically necessary for the safety of the athlete or for the safety of other athletes in the competition. The use of intravenous fluids or other medications during competition (as long as they are not banned substances) are not specifically listed as grounds for disqualification, but they may be subject to review. Additional rules about clothing, shoes, and athlete interactions with race officials, if breached, may result in disqualification (http://www.usatf.org/about/rules/2010/2010rules.pdf).
Triathlons
Triathlons, which consist of swimming, cycling, and running, are held in various lengths: sprint length (a 400- to 800-m [0.25-mile to 0.5-mile] swim, a 16- to 24-km [10- to 15-mile] bike, and a 5-km [3.1-mile] run); international or Olympic length (1500-m [0.9-mile] swim, 38- to 43-km [24- to 27-mile] bike, 10-km [6-mile] run); and “Ironman” or ultra-triathlon (4-km [2.4-mile] swim, 180-km [112-mile] bike, 34-km [26.2-mile] run) that may last many hours, or days in the case of staged races. USA Triathlon (USAT) is the governing body for triathlons in the United States (http://www.usatriathlon.org).
Most races allow for medical assistance by official event personnel, although rules among events vary and often intentionally leave room for individual interpretation. For example, the rules for the 2010 Ironman Triathlon did not specifically state whether IV fluid administration would be considered grounds for disqualification (http://www.ironmanusa.com/usat-wtc-faq.pdf). Although many unsanctioned events use USAT rules as guidelines, medical providers and participants must be sure to understand the rules of the specific race in which they are involved. It is often helpful to have medical providers participate in development of these rules.
Medical Support for Wilderness and Endurance Events
Mass Gatherings
Information from the study of mass gatherings serves as a background for provision of medical support for wilderness and endurance events. A significant amount of variation exists in the literature concerning the definition of a mass gathering. In some cases, it has been defined as an event with more than 1000 participants; in others, an event is not considered a mass gathering unless there are more than 25,000 participants.7,30
Provision of medical support for any event begins with development of a medical support plan. Several authors have described this process for mass gatherings.8,23,26 The basic goals are to provide rapid access and triage, stabilization and transport of seriously injured or ill patients, and on-site care for minor injuries and illnesses.7 Nine important elements of planning are attendance or crowd size, personnel, medical triage and facilities, communication, transportation, medical records, public information and education, mutual aid, and data collection.23
General recommendations have been made about location and staffing of on-site medical facilities at mass gatherings. One group of investigators recommends that advanced life support (ALS) units be in place so that the response time from collapse to ALS care is 5 minutes or less for all participants under all conditions.41 Others have suggested the goals of basic first aid in 4 minutes, ALS care in 8 minutes, and evacuation to a medical facility within 30 minutes.38 For staffing, it has been suggested that the minimum staffing for every 10,000 participants be a two-person team consisting of registered nurses, emergency medical technicians, or paramedics or a combination of these.
In terms of on-site medical care provision, events may be divided into four categories, classes, or types. Category I events are those in which spectators remain seated for a set period of time or for the duration of the event. Common examples include stadium sporting events and concerts. In category II events, such as golf tournaments, Mardi Gras/Carnival celebrations, and state fairs, spectators are mobile and may become participants in the events. A large geographic area and participants often outnumbering spectators characterize category III events, which include charity walks, bicycle rides, marathons, and triathlons.33 In addition, because of the extreme nature and the unique challenges in providing medical support for adventure races and similar endurance events, several authors have labeled these events as category IV events.5,48,49,51 In general, categories III and IV events do not meet the participant number criterion of mass gatherings.
Most of the existing investigations of medical support involve categories I and II events, with a smaller number of investigations of category III and category IV events. Generally, investigations of categories I and II events have included frequency and type of injuries and illnesses treated, rate of utilization of on-site medical services, and rate of transfer to local care facilities. Their focus has been to determine what factors influence the type and frequency of injuries and illnesses with a goal of better anticipating needs and thus establishing appropriate guidelines and standards of care. Much of the information in these investigations is anecdotal and descriptive; several studies have concluded that there is no standard of care for emergency medical services at mass gatherings.2,7,38,41
The incidence of true medical emergencies at mass gatherings appears to be relatively small. In one large study, 75% of medical encounters involved respiratory illnesses, heat-related injuries, and minor problems, such as sunburn, blisters, and headache. Asthma was the most common reason for required acute medical intervention.3
The relationship between attendance (crowd size) and utilization of on-site medical services is unclear. Several studies have found that overall utilization grew with attendance but that utilization rate did not increase and, in some cases, actually decreased, with larger attendance.2,8,54 Rate of utilization of on-site medical services varies widely among events, ranging from 0.14 to 90 patients per 1000 participants, with most events reporting 0.5 to 2 patients per 1000 participants.2,7,41
Crowd (participant) demographics, event type, and availability of alcohol and drugs may also be used to help estimate utilization of medical resources. As one might predict, studies demonstrate that when alcohol is readily available, there is an increase in medical problems related to intoxication.2,30 One might expect to treat medical problems related to drug and alcohol use during a rock concert. In contrast, during a Papal visit, one might expect less intoxication but more cardiac-related problems.26
In the end, a number of factors may influence the utilization rate and type of medical care required, including the type and duration of the event, weather, availability of alcohol and drugs, and demographics of the crowd, including average age, density, and mood.2,3,30
Wilderness And Endurance Events
Wilderness and endurance events often occur in rough and remote terrain where communication may be very difficult, transport time to definitive care prolonged, and technical search and rescue required. In some wilderness events, the entire course is set, whereas in others, there is no set course between checkpoints and transition areas. In events with no set course, the exact location of each team may be unknown. In addition, many of these events are not staged, resulting in hundreds of miles separating lead teams from the back of the pack (Figure 103-1). Categories III and IV events present additional challenges in the provision of medical care and represent a new and important area of event and wilderness medicine.
Development of a Medical Support Plan
Provision of medical support for any event begins with development of a medical support plan. The importance of early planning, organization, and good communication cannot be overemphasized.52 For any event, the medical support plan should be based on anticipation of need. This begins with estimation of both number of patients and type of injuries and illnesses that will require treatment in both the best-case and worst-case scenarios. It is often helpful to review utilization of medical resources for similar events that have been held.26 In addition, as previously described, a number of factors that influence utilization of medical resources should be considered.
Development of a medical support plan should be done under direction of the event’s medical director. The primary responsibilities of the medical director are the health and safety of participants. The medical director may be a physician, paramedic, emergency medical technician, nurse, or other medical professional. Ideally, this individual should have prior experience as a medical director for similar events and will serve as care provider, planner, advisor, educator, and liaison with the community.19 It is essential that the director be familiar with the location of the event, including the capability of local emergency medical services (EMS), local health care facilities, and in the case of category IV events such as adventure races, local search and rescue (SAR) system. Medical support plan development should begin several months to several years before the event, depending on event complexity.
Development of a medical support plan begins with careful review of the course, including its location, disciplines required, time of year, and the climate conditions, including precipitation, temperature, and humidity. In this way, the occurrence and type of injuries, illnesses, endemic diseases, and environmental emergencies, such as dehydration, heat and cold illness, and altitude illness, can be roughly anticipated. High temperature and relative humidity can have a major effect on utilization of on-site medical resources. Both of these factors are associated with increases in demand for on-site medical services; however, humidity has a larger effect than does temperature. In mass gatherings, availability of water also influenced the incidences of dehydration and heat illness.2,7,26 For any event, it is important to know the likely temperature and humidity and to plan accordingly.
In general, the medical support plan should be comprehensive and outline all aspects of medical support, including a complete list of medical supplies, equipment, and personnel (Box 103-1). Treatment and transfer protocols should be clearly outlined, assigning any penalties for receiving medical care and establishing indications for medical disqualification or withdrawal from the event. It is important that the medical support plan be based on estimates of the type and frequency of injuries and illnesses expected in both the best and worst case scenarios.
BOX 103-1
Suggested Medical Equipment and Supplies for Wilderness and Endurance Events
Modified from Townes DA: Wilderness medicine: Strategies for provision of medical support for adventure racing. Sports Med 35:557, 2005.
The basic goal of the medical support plan should be to provide definitive treatment for minor illnesses and injuries, establish initial stabilization, and facilitate transfer for more severe illnesses and injuries49 (Figure 103-2). Again, it is fundamental that the medical support plan be based on anticipation of need. For the event medical director, adventure races and other category IV events present the greatest challenge in medical support plan development, often occurring in sparsely populated rural or very remote, rugged wilderness terrain. Unfortunately, there is relatively little information available for these events to assist the medical director in developing the medical support plan; anticipating medical needs thus remains a challenge. Available information demonstrates that medical providers should be prepared to treat a wide variety of injuries and illnesses.14,51
Personnel, Equipment, Supplies, And Logistics
Equipment and Supplies
The medical support plan should include a list of all medical supplies. The list should be available at each medical tent or station. In this way, an inventory can be maintained, and personnel will not waste time looking for items that are not available. A sample supply list is shown in Box 103-1. Substitutions, adjustments, additions, and subtractions should be made based on the event. It is useful to have all supplies packaged in durable carts, with the location of supplies standardized so that each cart is as similar as possible (Figure 103-3). This allows personnel to move from one medical station to another and easily locate supplies. Supplies should be packaged in clear plastic bags and labeled (with an index card inside the bag) to aid in organization, especially when supply carts are moved over rough terrain from one point to another on the course. Equipment and supply needs should be anticipated and adjustments made in the number of supplies at each medical station. Examples include anticipating that foot care supplies will be in high demand after a long trek, but less so after a kayaking section of the course; or predicting that skin lubricant or antifungal creams will be in higher demand during the latter part of the endurance event. Cycling events and mountain biking sections of adventure races events may have a higher need for bandaging and wound cleanings and care supplies, due to the higher potential for large abrasions sustained from falls while cycling.
Acceptance Of Medical Care
One area of controversy among medical personnel, event organizers, and athletes involves penalties for acceptance of medical support during an endurance event. The administration of intravenous fluid (IVF) is a commonly cited example. If the acceptance of IVF results in disqualification, athletes may push themselves too hard in an attempt to remain in the event. If IVF is administered without penalty, racers may request it at every opportunity to gain a theoretical competitive advantage. The authors and several race directors of both categories III and IV events use an “IVF rule” intended to allow fair and safe competition. This should be tailored for each individual event. For example, the IVF rule used during the Primal Quest expedition-length adventure race is shown in Box 103-2. As more events are held and investigations undertaken, such rules may be refined.
BOX 103-2
Intravenous Fluid Rule Used During the Primal Quest, 2002-2008
From Townes DA: Medical Support Plan: Primal Quest 2002. Unpublished.
EMS and SAR
It is essential to identify local ground and air ambulance services, search and rescue services, care facilities, and hospitals and trauma centers (and their capabilities) for each location along the course (Figure 103-4). Expedition-length adventure races may cover multiple hospital, trauma center, and EMS and SAR jurisdictions. At each medical station, there should be a folder containing the location and contact information for the resources specific to that medical station. It should also include the location and description of the medical station that will be readily understood by local providers. For example, when requesting a local ambulance, it will be more efficient to describe “Spring Valley Camp Ground, off of County Road 14” rather than “medical tent 5.” In this way, any medical personnel, even those without local knowledge, are able to quickly and accurately request the services and communicate accurately. It is also important to determine whether a national emergency network such as 9-1-1 is available and whether it can by accessed with an out-of-area cellular phone. The importance of working with local providers cannot be overemphasized. It is strongly recommended that a member of the local EMS community act as a liaison between the race and the local medical community. This individual is often helpful in determining what EMS, SAR service, or care facility should be utilized.
Injuries and Illnesses
by Event Type
Cycling Events
The most common reasons to need medical care during cycling events include dehydration, heat illness, and soft tissue injuries. During the 1996 California AIDS Ride,17 heat-related illness accounted for 31% of all encounters, followed by pulmonary complaints (12%), and orthopedic problems (9%). During the 2001 Midwest AIDS Ride,50 dehydration accounted for 35% of encounters, followed by orthopedic problems (27%), skin and soft tissue problems (10%), ophthalmologic problems (6%), gastrointestinal problems (6%), respiratory problems (4%), head and neck problems (3%), allergic reactions (3%), cardiac problems (2%), psychiatric problems (<1%), and other problems (4%). The most common orthopedic problem was overuse injury of the knee, primarily due to iliotibial band (ITB) syndrome.17,50 Fortunately, major trauma is rare. This is likely in part because of mandatory helmet use and protection from traffic provided by these events.
Triathlons
The overall injury rate for triathlons has been calculated at 13% to 25% of participants.25 Each of the three disciplines is associated with a fairly unique set of injuries.
The swimming section of triathlon events has the greatest potential for mortality. It is essential to have sufficient rescue boats with qualified personnel in the water. Fortunately, the swimming section is associated with the fewest overall problems, accounting for only 3% of medical visits in one study.25 Other than drowning, hypothermia is perhaps the greatest risk during the swimming section. Mandatory use of wetsuits may reduce this incidence. Blunt trauma from kicking and corneal irritation or abrasion from trauma, goggles, and defogging solutions are not uncommon. In addition, man-of-war stings, sea urchin punctures, coral lacerations, and aspiration have all been reported.44 Leptospirosis has also been described in triathlon participants.11
The biking section is associated with trauma, including fractures, sprains, and abrasions, or “road rash.” Biking accounts for 7% to 10% of triathlon injuries.25 Occurrence of significant injury is reduced by rules that require helmet use and do not allow drafting.
The running section at the end of the triathlon is associated with the largest demand for medical assistance. In fact, 75% of medical care is delivered in the last 8 hours of the event, with a full 75% directly at the finish. Many of these injuries and illnesses are due to dehydration and electrolyte abnormalities.25
Marathons
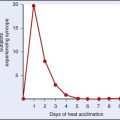
In a 12-year study of the Twin Cities Marathon in Minneapolis, Minnesota, 90% of medical encounters occurred at the finish line. The most common reason was exercise-associated collapse (59%), followed by skin problems (21%), musculoskeletal problems (17%), and other medical problems (3%).35 The mechanism of collapse at the end of a marathon may be due to postural hypotension from inadequate venous return secondary to decreased skeletal muscle massage on stopping.32 Sudden cardiac deaths have been reported during marathons, but they are exceedingly rare.29 About one-half of these cases have occurred in individuals with cardiac disease.13 Heat illnesses, including heat exhaustion and heat stroke, occur in participants who are not properly acclimatized, especially during events in warmer climates.
Adventure Races
Injuries and illness are common during adventure races. Many are minor, and relatively few result in withdrawal from an event.4,46,51 Most injuries involve skin and soft tissues.4,14,51 In a survey of 223 adventure race athletes, 73% reported at least one injury (acute or chronic) during the 18 months before the survey.14 This is comparable with overall (acute and chronic) injuries reported during orienteering and standard triathlons, although lower than in ultra-endurance triathlons, in which injury rates as high as 90% have been reported. In the survey, 44% of advanced, 35% of intermediate, and 19% of beginner racers reported acute injuries. Chronic injuries were more common, reported in 59%, 54%, and 56% of athletes, respectively.14 Acute injuries are considerably more common during adventure races when compared with triathlons. Some of the difference has been attributed to lower extremity injuries sustained during maneuvering over unstable terrain and the inherent risks of mountain biking. In the survey, the most common site of acute injury was the ankle, followed by arm and shoulder, knee, and lower back.14
In a prospective cohort study of injuries and illness treated during the Primal Quest expedition-length adventure race held in 2002 in Telluride, Colorado, 243 medical encounters and 302 distinct injuries and illnesses were reported among the 248 athletes who participated. Of the 179 (59%) injuries and 123 (41%) illnesses reported, skin and soft tissue injuries were the most common (48%), with blisters on the feet representing the single most frequent reason to utilize on-site medical resources (32.8%).51 A complete list of injuries and illness by type, number, and frequency is given in Table 103-1.
TABLE 103-1 Injuries and Illness During the Primal Quest, 2002
| Type of Injury/Illness | Number of Cases (n = 302) | Percentage of Cases |
|---|---|---|
| Skin/soft tissue | 145 | 48.0 |
| Respiratory | 55 | 18.2 |
| Altitude (AMS/HAPE) | 36 | 11.9 |
| Orthopedic | 29 | 9.6 |
| Dehydration | 21 | 7.0 |
| Gastrointestinal | 6 | 2.0 |
| HEENT | 5 | 1.7 |
| Genitourinary | 3 | 1.0 |
| Other | 2 | <1.0 |
From Townes DA, Talbot TS, Wedmore IS, et al: Event medicine: Injury and illness during an expedition-length adventure race, J Emerg Med 27:161, 2004.
Although injury was more common overall, illness resulted in more medical withdrawals from the event. Of the 28 athletes who withdrew for medical reasons, 60% withdrew because of illness. Respiratory illness, including upper respiratory infection (URI), bronchitis, and reactive airway disease–asthma, were the most common (32.1%) medical reasons to withdraw, followed by dehydration (25.0%), altitude illness (14.3%), skin and soft tissue problems (14.3%), orthopedic problems (10.7%), and genitourinary problems (3.6%).4 In a similar study, the only medical withdrawal from a 2-day wilderness multisport event was due to reactive airway disease in the setting of a viral respiratory infection.4
Reactive airway disease–asthma appears to be a common cause of illness during adventure races. The relatively high incidence observed may be partially explained by changes in respiratory function in adventure race participants. This has been demonstrated by several investigations. In one study of 2 consecutive years of a wilderness multisport endurance event, measurements of oxygen saturation (SaO2), forced expiratory volume in 1 second (FEV1), and forced vital capacity (FVC) were taken before and after the event and at 45-minute intervals during the event. During the event, there was a progressive decline in both FEV1 and FVC from the normal baseline observed at the start. At the finish, the FEV1 had declined 25% and 22% and FVC had declined 14% and 22%, respectively, for the 2 years. Changes in SaO2 were less dramatic.37 In a similar study of 25 adventure race athletes, a mean decrease in FEV1 of 15.1% and FVC of 13.0% was observed between the start and finish of the event. Fourteen (56%) of these athletes had a decrease in FEV1 and FVC of more than 10%, and 7 (28%) had a decrease of more than 20%.36 Decline in respiratory function has been described in other endurance athletes but to a lesser degree.21,27,28 Possible explanations for these findings include bronchospasm, airway inflammation, muscle fatigue, and pulmonary edema.
Complicating the understanding of reactive airway disease–asthma observed during adventure races is the fact that many events have sections that occur at high altitude. In an investigation of the 2002 Primal Quest, the incidence of altitude illness requiring medical treatment was 14.1%. Most cases were acute mountain sickness (AMS) (13.3%), and only 0.81% of cases were high-altitude pulmonary edema, but the potential role of altitude illness in exacerbating or alleviating other respiratory problems remains a concern.46
Previous studies have demonstrated improvement in asthma at high altitude. Explanations offered for this observation include reduction in pollen and pollution, and increase in cortisol levels at high altitude.1,6 Other studies have found that exercise at altitude may exacerbate AMS.34 Further studies are necessary to fully understand the interaction between reactive airway disease–asthma, respiratory tract infections, and altitude illness during adventure races.
In addition, injuries and illnesses due to environmental exposure are common during adventure races. A study of Australia’s Winter Classic, a 2-day event, found that 21% of participants developed symptoms consistent with exposure.4 During the Primal Quest in 2003, 25% of medical withdrawals were attributed to dehydration or heat illness.51
specific injuries and illnesses
Endemic Disease
In the 1997 Raid Gauloises held in Lesotho and Natal, South Africa, 13 French athletes were diagnosed with African tick-bite fever. This rickettsial disease is caused by Rickettsia africae and transmitted by Amblyomma ticks. Signs and symptoms included fever, headache, multiple inoculation scars, regional lymphadenopathy, and rash.15
The most widely publicized outbreak was of leptospirosis during the Eco-Challenge-Sabah 2000 adventure race held in Malaysian Borneo.9,10,39,44 Of the 304 athletes competing, 189 were contacted, of which 80 met the case definition for leptospirosis. No deaths were reported. Risk factors identified were kayaking or swimming in the Segama River, swallowing water from the Segama River, and spelunking (caving). Swimming in the Segama River was the only risk factor independently associated with illness. Of the 20 athletes who reported taking doxycycline for prophylaxis of malaria or leptospirosis, four (20%) developed symptoms of leptospirosis. When this rate was compared with those not taking doxycycline and adjusted for exposure, doxycycline use was determined to be protective; however, the difference was not significant.39 Leptospirosis infections have also been attributed to participation in an adventure race in Guam, triathlons in Illinois and Wisconsin, and white-water rafting in Costa Rica.11,12,20
Myiasis, an infection of humans by fly larvae, has also been reported during an adventure race. In 2001, during a race in the Para jungle region of Brazil, an athlete fell and sustained a wound that was infected with a third-stage larva of the New World screwworm fly, Cochliomyia hominivorax. Although most cases of myiasis are generally benign, infection by invasive species like the screwworm may result in extensive tissue damage, pain, and even death because the larvae have powerful oral hooks that can invade cartilage and bone.40
Major Trauma
Major trauma has occurred during wilderness and endurance events, resulting in significant injuries and death.24 Fortunately, the incidence is low, but because of potential morbidity and mortality, the medical support plan should include equipment, supplies, and personnel to provide initial stabilization and treatment of major trauma. It should also include a protocol for evacuation and transport developed in close conjunction with local EMS and, in the case of adventure races, local SAR. Obtaining the appropriate personnel and equipment may require a significant financial commitment by the race organization. The medical director must emphasize the importance of these resources and insist on them, even though they may go unused. Examples include full-time paramedic-staffed ALS ambulances, helicopters, and other rescue vehicles. Litters and Gamow chambers can represent a significant expense for some events. The medical support plan should outline the location of these limited resources and their movement during the event. For example, it may be necessary to “leapfrog” ambulances from one location to another during the event to use them most effectively. This planning should be done before the start of the event.
Foot Care
Foot-related problems (see Chapter 29), particularly blisters, are perhaps the most common reason to seek medical care during wilderness and endurance events (Figure 103-5). In one investigation during an adventure race, blisters on the feet were the most common reason to need care, accounting for 53% of all medical encounters.51
There seem to be as many different techniques for prevention and treatment of blisters as there are feet. Athletes use duct tape, antiperspirants, petroleum jelly, and multiple newer products designed specifically for blister prevention. In a text dedicated to the subject, the authors list 159 ways to prevent blisters.53 Despite the variety of preventive methods, susceptibility to blisters varies. Although some athletes remain blister-free with little effort, others suffer from blisters no matter what measures are taken.
Dehydration and Hyponatremia
Dehydration and hyponatremia are common during wilderness and endurance events, especially marathons and triathlons, and members of the medical team should be familiar with their recognition, diagnosis, and treatment (Figure 103-6). During the Hawaii Ironman Triathlon, dehydration was the most common reason to receive on-site medical care, and hyponatremia the most common electrolyte disturbance. Dehydration with hyponatremia is rare in races lasting less than 4 hours but becomes more common in races lasting longer than 8 hours.22
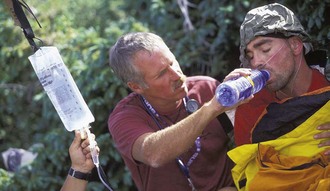
FIGURE 103-6 Dehydration and hyponatremia are common in wilderness and endurance events.
(Courtesy Tim Holstrom.)
Hyponatremia is defined as serum sodium less than 135 mEq/L associated with malaise, disorientation, hyperreflexia, nausea, and fatigue. More severe cases may result in seizures, stupor, coma, and death. Seizures have been reported in a triathlete with serum sodium of 116 mEq/L, and rapid neurologic deterioration and encephalopathy in ultra-marathon runners.18,43,45
Hyponatremia occurs when free water intake exceeds free water loss. In the endurance athlete, this is thought to occur in two distinct ways, although there is some debate about the exact etiology of exercise-associated hyponatremia. Several authors have suggested that hyponatremia is a result of net water gain during exercise secondarily associated with sodium loss through sweat.22 Others have attributed it to salt depletion due to massive sweat losses associated with net dehydration.22 Additional studies have demonstrated that hyponatremia may occur in the setting of dehydration or overhydration.42
In a study of 605 participants in the New Zealand triathlon, 58 (18%) were found to be hyponatremic. Of these, 18 were symptomatic, and 11 were severely hyponatremic, defined as having serum sodium of less than 130 mmol/L. Post-race serum sodium concentration was inversely related to weight change during the event. That is, athletes with hypernatremia were dehydrated, while athletes with severe hyponatremia were generally overhydrated. The relationship between mild hyponatremia and hydration status was less clear. Some athletes with mild hyponatremia were dehydrated, whereas others were overhydrated. It would appear that the mechanisms for mild hyponatremia in the endurance athlete include fluid overload, large salt losses through sweat, or a combination of the two.42
Whatever the mechanism, it is important to be aware of both dehydration and hyponatremia in triathlon participants. Recommendations to help reduce the incidence of dehydration and hyponatremia include the following: (1) athletes should have 0.5 L of fluid intake for each pound lost during an event, (2) during races lasting more than 4 hours, athletes should use some form of sodium replacement (1 g/hr), (3) athletes from cooler climates should give themselves a week to acclimatize and should increase salt intake by 10 to 25 g/day, and (4) IVF therapy for races longer than 4 hours should be 5% dextrose in normal saline; for races less than 4 hours, either 5% dextrose in normal saline or 5% dextrose in 0.5 normal saline.22 Studies of marathon runners have suggested that replacement of sodium at a rate of 20 mEq/hr and potassium at 8 mEq/hr will maintain normal blood levels.31
1 Allegra L, Cogo A, Legnani D, et al. High altitude exposure reduces bronchial responsiveness to hypo-osmolar aerosol in lowland asthmatics. Eur Respir J. 1995;8:1842.
2 Arbon P. The development of conceptual models for mass-gathering health. Prehosp Diast Med. 2004;19:208.
3 Arbon P, Bridgewater FH, Smith C. Mass gathering medicine: A predictive model for patient presentation and transport rates. Prehosp Diast Med. 2001;16:150.
4 Borland ML, Rogers IR. Injury and illness in a wilderness multisport endurance event. Wilderness Environ Med. 1997;8:82.
5 Burdick TE, Brozen R. Wilderness event medicine. Wilderness Environ Med. 2003;14:236.
6 Cogo A, Basnyat B, Legnani D, et al. Bronchial asthma and airway hyperresponsiveness at high altitude. Respiration. 1997;64:444.
7 De Lorenzo RA. Mass gathering medicine: A review. Prehosp Diast Med. 1997;12:68.
8 De Lorenzo RA, Gray BC, Bennett PC, et al. Effect of crowd size on patient volume at a large, multipurpose, indoor stadium. J Emerg Med. 1989;7:379.
9 Department of Health and Human Services, Centers for Disease Control and Prevention. Update: Outbreak of acute febrile illness among athletes participating in Eco-Challenge-Sabah 2000—Borneo, Malaysia, 2000. JAMA. 2001;285:728.
10 Department of Health and Human Services, Centers for Disease Control and Prevention. Update: Outbreak of acute febrile illness among athletes participating in Eco-Challenge-Sabah 2000—Borneo, Malaysia, 2000. MMWR. 2001;19:21.
11 Department of Health and Human Services, Centers for Disease Control and Prevention. Update: Leptospirosis and unexplained acute febrile illness among athletes participating in triathlons—Illinois and Wisconsin, 1998. MMWR. 1998;47:673.
12 Department of Health and Human Services, Centers for Disease Control and Prevention. Outbreak of leptospirosis among white-water rafters—Costa Rica, 1996. MMWR. 1997;46:577.
13 Drory Y, Kramer M, Lev B. Exertional sudden death. Med Sci Sports Exerc. 1990;23:147.
14 Fordham S, Garbutt G, Lopes P. Epidemiology of injuries in adventure racing athletes. Br J Sports Med. 2004;38:300.
15 Fournier PE, Roux V, Caumes E, et al. Outbreak of Rickettsia africae infections in participants of an adventure race in South Africa. Clin Infect Dis. 1998;27:316.
16 Perseus Project Database, Tufts University. Frequently asked questions about the ancient Olympic games. http://www.perseus.tufts.edu/Olympics/faq10.html.
17 Friedman LJ, Rodi SW, Krueger MA, et al. Medical care at the California AIDS Ride 3: Experiences in event medicine. Ann Emerg Med. 1998;31:219.
18 Frizzell RT, Lang GH, Lowance DC, et al. Hyponatremia and ultra-marathon running. JAMA. 1986;255:772.
19 Gonzalez D. Medical coverage of endurance events. Prim Care. 1991;18:867.
20 Haddock RL, Gilmore JW, Pimentel F. A leptospirosis outbreak on Guam associated with an athletic event. Pac Health Dialog. 2002;9:186.
21 Hill NS, Jacoby C, Farber FW. Effect of an endurance triathlon on pulmonary function. Med Sci Sports Exerc. 1991;21:1260.
22 Hiller DB. Dehydration and hyponatremia during triathlons. Med Sci Sports Exerc. 1989;21:S219.
23 Hnatow DA, Gordon DJ. Medical planning for mass gatherings: A retrospective review of the San Antonio Papal Mass. Prehosp Disast Med. 1991;6:443.
24 Jhung L. Fateful journey. Adventure Sports. 2004;Nov/Dec:24.
25 Laird RH. Medical care at ultra-endurance triathlons. Med Sci Sports Exerc. 1989;21:S222.
26 Leonard RB. Medical support for mass gatherings. Emerg Med Clin North Am. 1996;14:383.
27 Mahler DA, Lake J. Lung function after marathon running at warm and cold ambient temperatures. Am Rev Respir Dis. 1981;124:154.
28 Mahler DA, Lake J. Pulmonary dysfunction in ultra-marathon runners. Yale J Biol Med. 1981;54:243.
29 Maron BJ, Poliac LC, Roberts WO. Risk of sudden cardiac death associated with marathon running. J Am Coll Cardiol. 1996;28:428.
30 Milsten AM, Maguire BJ, Bissell RA, et al. Mass-gathering medical care: A review of the literature. Prehosp Diast Med. 2002;17:151.
31 Newmark SR, Toppo FR, Adams G. Fluid and electrolyte replacement in the ultra-marathon runner. Am J Sports Med. 1991;19:389.
32 Noakes T. Fluid replacement during marathon running. Clin J Sport Med. 2003;13:309.
33 Norberg M. EMS and mass gatherings. Emerg Med Serv. 1990;19:46. 54-56, 91
34 Roach RC, Maes D, Sandoval D, et al. Exercise exacerbates acute mountain sickness at simulated high altitude. J Appl Physiol. 2000;88:581.
35 Roberts WO. A 12-year profile of medical injury and illness for the Twin Cities Marathon. Med Sci Sports Exerc. 2000;32:1549.
36 Rogers IR, Inglis S, Speedy D, et al. Changes in respiratory function during a wilderness multisport endurance competition. Wilderness Environ Med. 2001;12:13.
37 Rogers IR, Speedy D, Hillman D, et al. Respiratory function changes in a wilderness multisport endurance competition: A prospective case study. Wilderness Environ Med. 2002;13:135.
38 Saunders AB, Criss E, Steckl, et al. An analysis of medical care at mass gatherings: Effect of crowd size on patient volume at a large, multipurpose, indoor stadium. Ann Emerg Med. 1986;15:515.
39 Sejvar J, Bancroft E, Winthrop, et al. for the Eco-Challenge Investigation Team: Leptospirosis in “Eco-Challenge” athletes, Malaysian Borneo, 2000. Emerg Infect Dis. 2003;9:702.
40 Seppanen M, Virolainen-Julkunen A, Kakko I, et al. Myiasis during adventure sports race. Emerg Infect Dis. 2004;10:137.
41 Spaite DW, Criss EA, Valenzuela TD, et al. A new model for providing prehospital medical care in large stadiums. Ann Emerg Med. 1988;17:825.
42 Speedy DB, Noakes TD, Rogers IR, et al. Hyponatremia in ultra-distance triathletes. Med Sci Sports Exerc. 1999;31:809.
43 Speedy DB, Rogers I, Safih S, Foley B. Hyponatremia and seizures in an ultra-distance triathlete. J Emerg Med. 2000;18:41.
44 Stone SC, McNutt E. Update: Outbreak of acute febrile illness among athletes participating in Eco-Challenge-Sabah 2000—Borneo, Malaysia, 2000. Ann Emerg Med. 2001;38:83.
45 Surgenor S, Uphold RE. Acute hyponatremia in ultra-endurance athletes. Am J Emerg Med. 1994;12:441.
46 Talbot TS, Townes DA, Wedmore IS. To air is human: Altitude illness during an expedition length adventure race. Wilderness Environ Med. 2004;15:90.
47 Reggae Marathon Limited. The origins of the marathon. http://www.reggaemarathon.com/index.php?option=com_content&view=article&id=81.
48 Townes DA. Event medicine: Medical support for adventure racing. Wilderness Med. 2003;20:7.
49 Townes DA. Wilderness medicine: Strategies for provision of medical support for adventure racing. Sports Med. 2005;35:557.
50 Townes DA, Barsotti C, Cromeans M. Injury and illness during a multi-day recreational bicycling tour. Wilderness Environ Med. 2005;16:125.
51 Townes DA, Talbot TS, Wedmore IS, Billingsly R. Event medicine: Injury and illness during an expedition-length adventure race. J Emerg Med. 2004;27:161.
52 Whipkey RR, Paris PM, Stewart RD. Emergency care for mass gatherings. Postgrad Med. 1984;76:44.
53 Vonhof J. Fixing your feet: Prevention and treatments for athletes, ed 3. Berkeley, Calif.: Wilderness Press; 2004.
54 Zeitz KM, Schneider DA, Jarrett D, et al. Mass gathering events: Retrospective analysis of patient presentations over seven years. Prehosp Diast Med. 2002;17:147.