Wide Excision With or Without Skin Graft
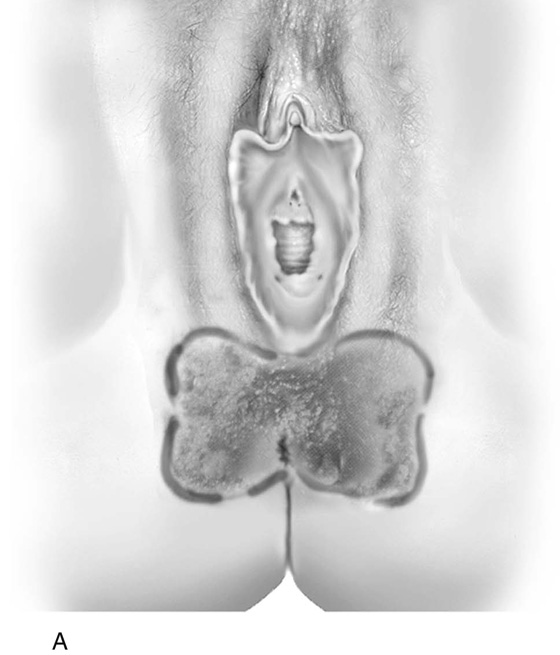
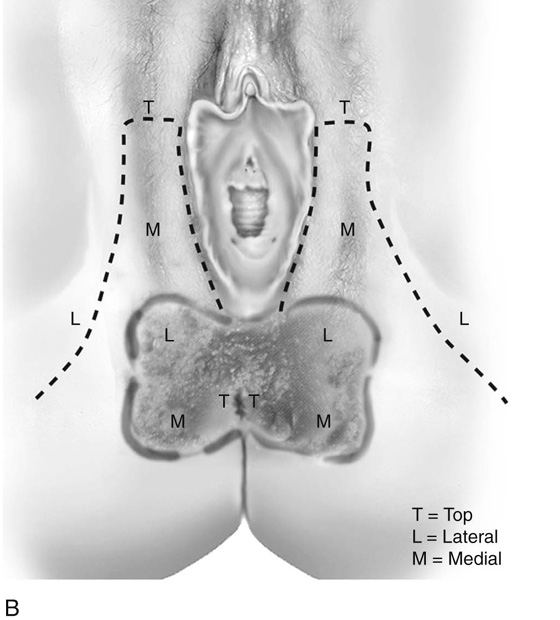
The treatment for vulvar intraepithelial neoplasia (VIN) varies depending on the extent of the disease process. Wide, local excision accomplishes therapeutic goals most simply and with the least disruption for the patient when the VIN is localized. On the basis of microscopic analysis of more than 1000 histologic sections of vulvar carcinoma in situ (CIS), the following data were obtained: (1) skin appendages (e.g., sebaceous glands, hair follicles, sweat glands) were involved (by extension) with neoplasia in 38% of all cases studied and in 60% of women older than 50 years of age; (2) skin appendages in hair-bearing areas extended to a mean depth of 1.53 ± 0.77 mm; (3) in the labia minora, extension of neoplastic cells into sebaceous glands plunged to a mean depth of 1.0 mm; and (4) the deepest skin appendage involvement (hair-bearing areas) was to a depth of 3 mm. Therefore, specifications for treatment required excision to a depth of 2.3 mm for labia majora and perineal and perianal skin; a depth of no more than 1 mm for the labia minora and periclitoral skin; and a peripheral margin of 3.0 mm (see Fig. 62–26).
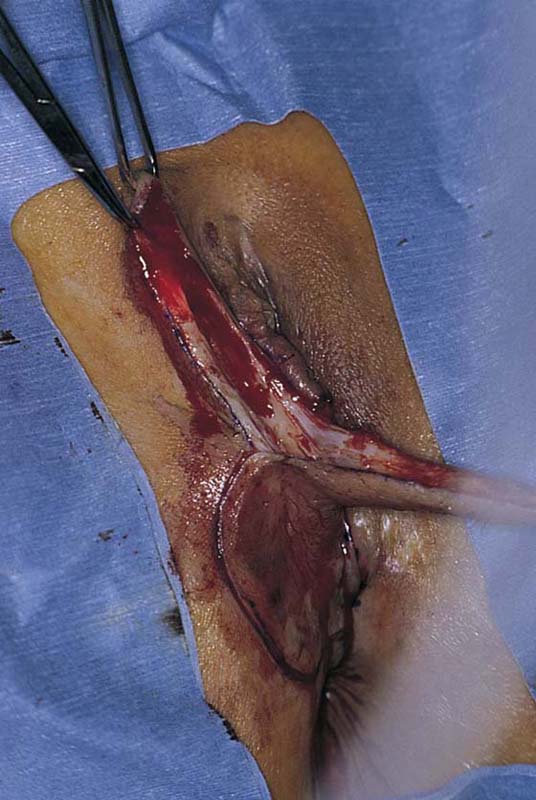
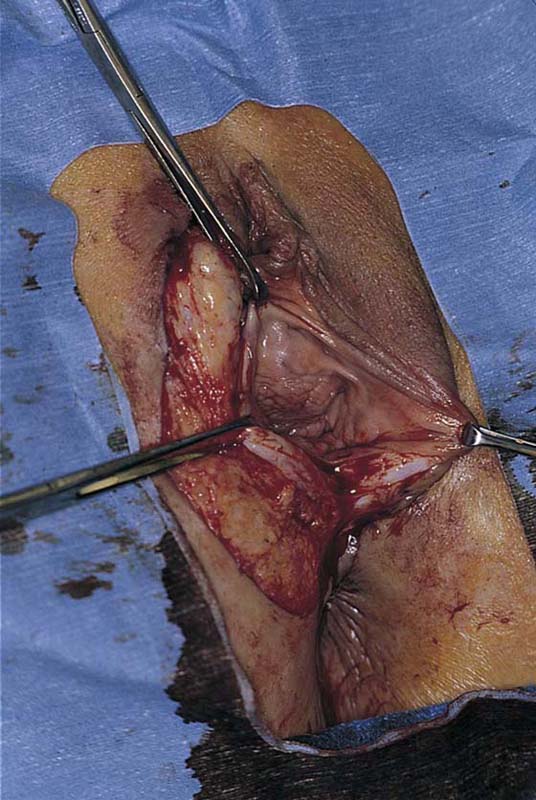
Sharp excision may be performed with conventional instrument (knife, scissors) or by means of a superpulsed carbon dioxide (CO2) laser. A basic tenet for surgical treatment of the vulva is limitation of deep tissue devitalization by energy devices (e.g., electrosurgical coagulation). After the excision is done, sufficient time and effort should be expended to obtain vigorous hemostasis. Bleeding vessels should be clamped and suture-ligated with 4-0 Vicryl (Figs. 68–1 through 68–4). When the latter is completed, the operative site is irrigated with normal warm saline. Primary closure without tension on the suture is the preferred method of closure. If the skin is tightly stretched to obtain closure, the edges may undergo necrosis and separate. Alternatively, wounds that are closed under tension are vulnerable to suture tear-out when inevitable postoperative tissue edema develops.
If primary closure is impossible or is tenuous, plans should be made to graft the operative site (Figs. 68–5A through 68–12B) either with a pedicle graft or a free graft (Fig. 68–13). The principle of the pedicle graft involves preservation of a plentiful blood supply to the graft. Therefore, the surgeon must know the source and direction of the blood vessels to avoid cross-cutting them. Second, the length of the graft should be approximately one-half the width of the base (i.e., if the height of the graft is 3 cm, then the pedicle width should be 6 cm) (Figs. 68–14 through 68–20). For small areas (i.e., 2 cm wide and 4 cm long), a full-thickness graft may be excised from the lower abdomen (see Fig. 68–11). This is carefully cleared of all fat and sutured into the wound. Finally, a split-thickness graft from the thigh or buttock may be obtained preoperatively and then grafted onto the wound. In actuality, this is the preferred method of treatment for large defect coverage. For all grafts, an evenly distributed pressure dressing is applied (Fig. 68–21).
When a large, deep resection or previous iatrogenic scar formation has compromised the blood supply and created massive tissue loss in the vulva or vagina, a myocutaneous graft should be considered. This type of graft provides tissue substance, as well as a blood supply to the graft. The graft utilizes the medially located gracilis muscle (see Chapter 70), which may be delivered via a tunnel from the thigh into the perineum or vagina (Figs. 68–22 through 68–24).
FIGURE 68–1 A lesion involving the entire right labium majus.
FIGURE 68–2 The labium has been excised with an adequate margin. The interlabial sulcus skin and the skin at the lateral margin of the labium majus have been approximated without excessive tension on the suture line.
FIGURE 68–3 Silver sulfadiazine (Silvadene) is plentifully applied to the wound postoperatively.
FIGURE 68–4 Instant Ocean tub baths are recommended on a daily basis during the recovery phase after vulvar surgery.
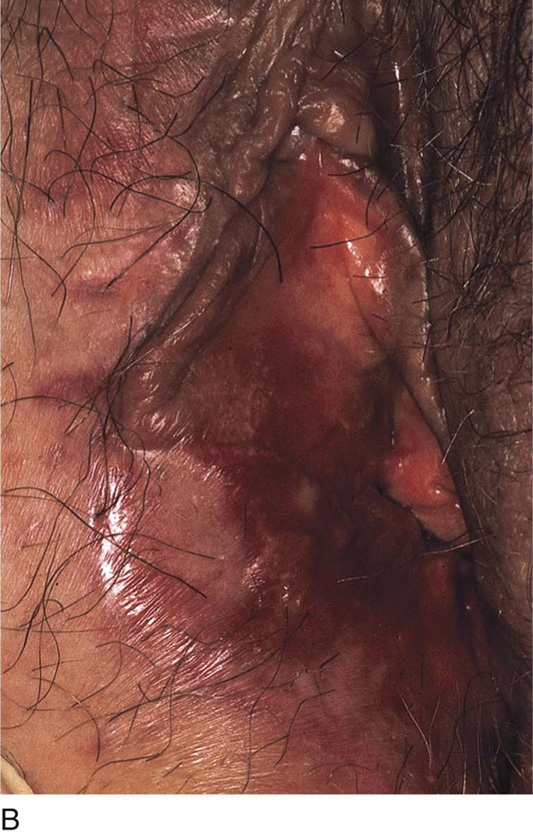
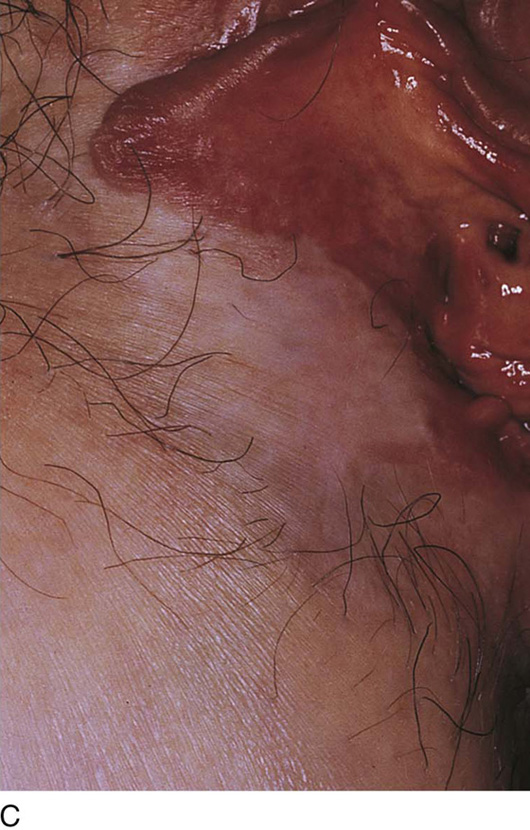
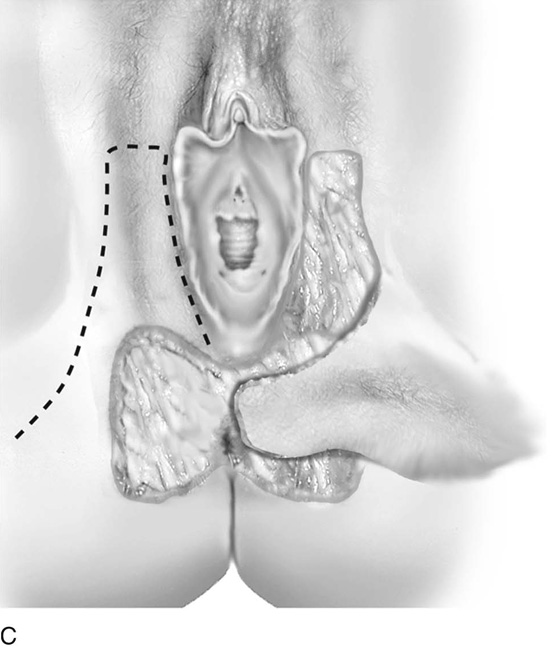
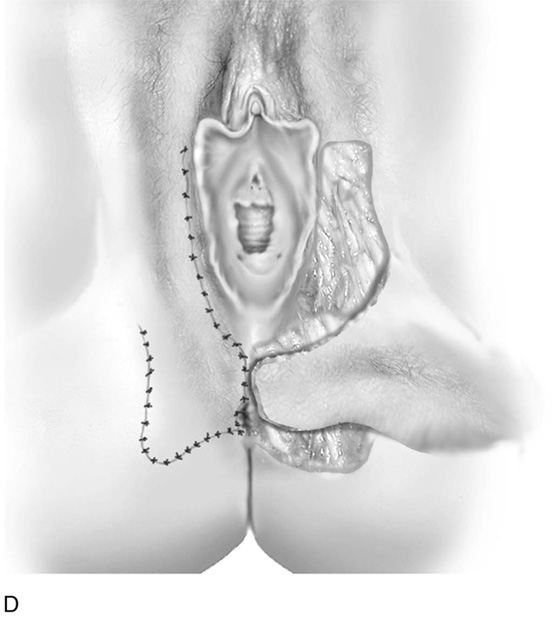
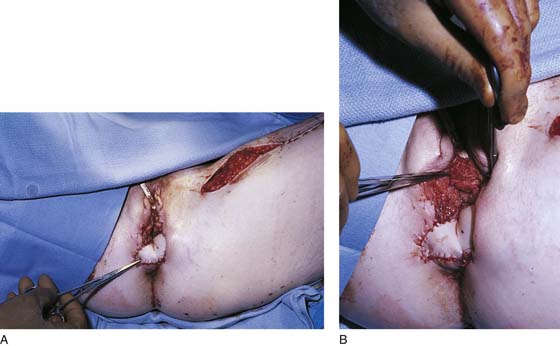
FIGURE 68–5 A. This patient has an extensive carcinoma in situ (CIS) of the right vestibule, labium minus, and labium majus. Note the recent biopsy wound in the lower labium majus. B. Another view of the red, dark brown, and raised areas of CIS. C. On the operating table, the extent of the area to be resected is sketched with a sterile marking pen.
FIGURE 68–6 The skin containing the carcinoma in situ (CIS) is sharply excised en bloc. A full-thickness resection (i.e., extending into the subcutaneous fat) is done.
FIGURE 68–7 Hemostasis is obtained with the use of mosquito clamps and 3-0 or 4-0 polydioxanone (PDS) or Vicryl suture-ligatures. The proper depth of excision is maintained by the operator by stretching the skin inferiorly and pushing up on the skin with the index finger at the line of resection.
FIGURE 68–8 The entire right side of the vulva has been removed. Only a portion of the right labium minus (including the clitoris and its hood) remains.
FIGURE 68–9 Allis clamps grasp the margins of the remaining portion of the right vestibule and the intact upper and left vestibular tissues.
FIGURE 68–10 The upper portion of the wound has been closed with 3-0 Vicryl without excessive tension on the suture line.
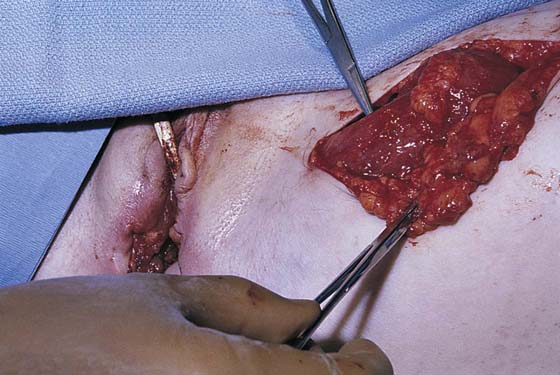
FIGURE 68–11 A graft is taken from the lower abdominal wall and is based on measurements of the vulvar wound defect. The skin is carefully defatted, moistened, and held in a sterile sponge until its use is required.
FIGURE 68–12 A. The graft seen in Figure 68–11 has been sutured into place to cover the defect left after extensive carcinoma in situ (CIS) resection of the right side of the vulva. B. View of part A shows the grafted site on the vulva 1 year postoperatively. Note that only one third of the right labium minus remains. C. Magnified view of the graft site at 1 year postoperatively.
FIGURE 68–13 Extensive bilateral excision of the vulvar tissues was required to eliminate another patient’s carcinoma in situ (CIS). A split-thickness graft was applied to the right side, whereas a pedicle graft was necessary on the left.
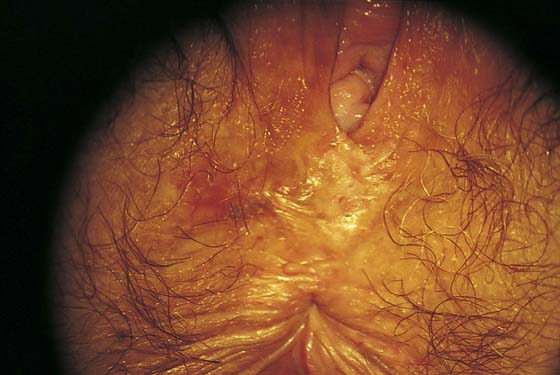
FIGURE 68–14 This patient had biopsy-proven carcinoma in situ (CIS) of the perineum and perianal skin.
FIGURE 68–15 The extent of the planned resection is outlined with a sterile marking pen.
FIGURE 68–16 The skin of the perineal and perianal area has been excised into the subcutaneous tissues.
FIGURE 68–17 A. The perianal and perineal defect is clearly seen. The full-thickness resection was shown in Figure 68–16. B. A broad-based pedicle graft is outlined. The graft will be cut and freed from the underlying fat and rotated posteriorly (inferiorly) and medially. C. The left flap has been rotated into place. D. The right flap has been rotated and sutured into place with 3-0 Vicryl. The donor site has been closed on the right. No sutures have been placed into the left-sided graft.
FIGURE 68–18 Allis clamps have been placed on the pedicle grafts to facilitate their rotation to cover the wound.
FIGURE 68–19 The grafts have been rotated, sutured into place, and secured.
FIGURE 68–20 Both pedicle grafts have been sutured into the margins of and cover the wound totally. The distal edges of the graft are sutured to the anal mucosa.
FIGURE 68–21 When the surgery has been completed, the wounds are thoroughly irrigated with sterile normal saline. Xeroform gauze is applied to the graft, and this is followed by the application of a pressure dressing. A Foley catheter has been placed in the bladder.
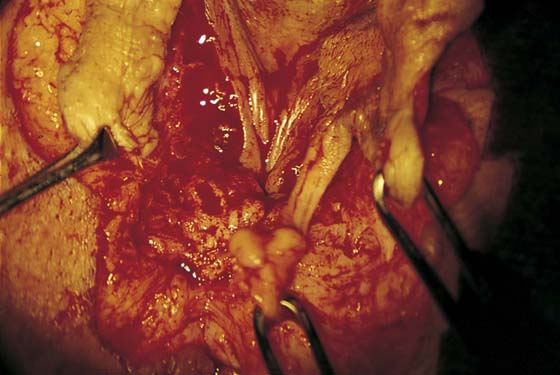
FIGURE 68–22 When an extensive mass of tissue is resected in the vulva or vagina, a myocutaneous graft is indicated. Here, the gracilis muscle and its posterior blood supply are secured.
FIGURE 68–23 A. The muscle, together with the overlying skin and subcutaneous tissue, constitutes the pedicle graft. This graft is rotated and delivered via a tunnel through the thigh to the labial area. The graft is then sutured into place after testing for the adequacy of blood flow (using Doppler sonography). B. Detailed view of part A. The wound is being closed.
FIGURE 68–24 A drain has been placed into a portion of the vagina. The left wall of the vagina and the perineum have been replaced and repaired with a gracilis myocutaneous flap.