Chapter 84 Which Bearing Surface Should Be Used: Highly Cross-Linked Polyethylene versus Metal or Metal versus Ceramic on Ceramic?
Total hip replacement changes the lives of more than one million patients worldwide each year. In wellselected patients, the success of the implant has historically meant that for nearly 90% of patients, their primary hip replacement is their only hip replacement.1 This level of success has been reached with multiple implants including cemented monoblock femoral stems with conventional cemented, all-polyethylene, acetabular components of several different designs. If this is the case, why are we looking for alternative bearings?
First, the levels of success in historical data were achieved only in select groups of patients. Many historical studies had an inbuilt selection bias. Surgeons were aware that there were certain diagnoses that fared poorly with the implants and techniques available to them, and in particular, younger patients did not respond as well in terms of survivorship of the implant. As such, patients who were perceived to be at high risk for unsuccessful results were not offered a total hip replacement. National registries are probably the best tool for observing the effect that age and diagnosis have on the revision rate. The Swedish registry has been collecting data relating age and diagnosis to the success of hip arthroplasty since 1979. Over this period, they have observed an overall diminishing revision burden, which they speculate may be caused by better surgical training, an improvement in the performance of modern implants compared with their historical counterparts, and surgeons modifying their practice to use combinations of implants that have performed well in the registry.2 Despite these favorable conditions for hip arthroplasty, there has been a relative increase in the revision rate of total hip replacements performed for inflammatory arthropathies, childhood hip disorders, and post-traumatic arthritis2—all diagnoses found predominantly in young people having total hip arthroplasties.
WHAT ARE THE TRIBOLOGICAL DEMANDS ON TOTAL HIP ARTHROPLASTY ARTICULATIONS?
Historically, wear particles from conventional polyethylene gamma irradiated in air, coupled with small-diameter metal or ceramic heads, has led to osteolysis and failure of the components after 5 to 15 years of use.3,4 In a study of Charnley hips retrieved at time of revision for aseptic loosening,5 the mean time to revision was 12 years, and the mean volumetric wear at failure was 785 mm.4 The same polyethylene had been tested in another study using a hip simulator, and this degree of volumetric wear was obtained after 12 years of wear when it was assumed that 1.5 million steps were taken in a year.6,7 Assuming 1.5 million steps per year as average use of the joint replacement, conventional articulations should have a total lifetime of between 10 and 20 million cycles before failure.
Young people have higher levels of activity than older patients by up to an additional million steps per year.8 They should also expect to live 20 to 40 years longer than the conventional recipients of total hip replacements. Younger patients are also planning to return to more vigorous activities with their hip replacements, and as such, we would expect that they would be at a greater risk for polyethylene failure and osteolysis, as well as an increased risk for dislocation than their historical counterparts. To improve both range of motion and stability, larger and larger diameter femoral heads have been developed.9 A progression has occurred from the 22.25-mm to the 26-, 28-, 32-, and now 36- and 38-mm metal heads for use in metal/poly articulations. These larger heads have increased wear associated with the increased surface area of the articulation.4,10 In hip simulator data, this is seen with conventional polyethylene and significantly reduced with highly cross-linked polyethylene. Even with the biggest heads, the wear of the highly cross-linked polyethylene is still significantly less than the historical wear rates of smaller heads against conventional polyethylene. Metal-on-metal articulations have even greater available bearing diameters and are now up to 44 mm with conventional stems and shells, and anatomic head sizes with surface replacement components.
Thus, the lifetime tribological demand that young people place on their hip replacements may have increased to between 100 and 200 million cycles. If a single implanted articulation is to cope with the expected increase in demand of the younger or more active patient, there would need to be at least a 10-fold improvement in the wear characteristics of the alternative bearing couple compared with conventional polyethylene for the bearing couple to survive without need for revision. This is the driving force behind the development of alternative bearing surfaces.11
Evidence
Hip simulator studies have been used extensively since the late 1990s to support the research and development of new bearing systems for hip prostheses.12–15 Total hip replacements often fail because of polyethylene wear debris-induced osteolysis.16 Most studies comparing cross-linked polyethylene and conventional polyethylene have concentrated only on volumetric wear. Osteolysis is, however, dependent on the size, shape, and chemical activity of the wear debris generated.17 To compare alternative bearing surfaces, one must determine the relative biological activity of the debris generated and then relate it to the volumetric wear of the articulation. This then gives a means of directly comparing the tribological and biological performances of different alternative bearings.5,17–25
CROSS-LINKED POLYETHYLENE
Ultra-high-molecular-weight polyethylene comprises long chains of polyethylene molecules, some in parallel and others in random orientation. When the polyethylene molecules are exposed to gamma irradiation, free radicals are released. With the release of free radicals from adjacent polyethylene molecules, two chains may link at the site from which the free radicals were released. The amount of cross linking is determined by the type of irradiation the polyethylene is exposed to, the dosage of radiation applied, the atmosphere in which the polyethylene is exposed to the radiation, and the postradiation treatment of the polyethylene.26 Cross linking improves the resistance of the polyethylene to adhesive and abrasive wear. This should result in decreased linear and volumetric wear in cross-linked polyethylene articulations compared with conventional polyethylene.
In hip simulator studies, there is an eightfold reduction in volumetric wear of cross-linked polyethylene compared with conventional polyethylene.19,24 Improvements in wear rate by an additional 40% are seen when ceramic heads are used against the cross-linked polyethylene.19,24 In clinical studies, a reduction in linear and volumetric wear has been seen using cross-linked polyethylene ranging from 28% to 95%.26–30 These observations would suggest that if volumetric wear alone determined osteolysis potential, cross-linked polyethylene should be a much better articulation than conventional polyethylene.
Unfortunately, cross-linked polyethylene produces wear debris that theoretically may have a specific biological activity double that of conventional polyethylene.19,24 Thus, even though there is an eightfold reduction in volumetric wear, there is only a fourfold improvement in the functional biological activity of the bearing couple. Thus, in vitro, cross-linked polyethylene articulations do not reach the 10-fold improvement in wear characteristics that are estimated to be required by younger patients having total hip replacement. In vitro experiments thus predict a reduction in osteolysis when highly cross-linked polyethylene is used; however, the reduction may not be proportionate to the observed reduction in the volumetric wear.
In a randomized, prospective study with minimum 4-year radiographic follow-up, the incidence of osteolysis was significantly less in the cross-linked arm of the study.27 This observation was more pronounced on the femoral side where the difference between the cross-linked and noncross-linked group was highly significant (P = 0.001). However, when the volume of the osteolytic area was examined, one finds that although the total volume of osteolysis was less in the cross-linked group, the difference was not significant (P = 0.4). In another 5-year retrospective study comparing cross-linked and conventional polyethylenes, there were no osteolytic lesions observed around the femoral components in the cross-linked group28 (Level of Evidence IV).
Thus far we have concentrated on the improved material property of wear resistance that cross-linked polyethylene has compared with conventional polyethylene. There are, however, downsides to crosslinking polyethylene, namely, the physical properties of yield strength, overall tensile strength, and resistance to elongation or crack propagation are all reduced.31 These physical properties are important to the overall survival of the implant because they each represent a mode through which the implant may fail. One needs to remember that wear-related osteolysis and aseptic loosening are not the only reasons that an implant may fail. Impingement of the neck of the femoral component on the polyethylene insert may result in catastrophic failure caused by fracture of the polyethylene. Fatigue failure of the locking mechanism may lead to loosening of the insert within the modular shell again, causing catastrophic failure.31 These failure mechanisms are rarely seen with conventional polyethylene; however, the diminished mechanical properties of cross-linked polyethylene raise concerns that failures because of these mechanisms may become more frequent.32 A balance therefore needs to be reached between the improved wear properties and the reduced physical properties of cross-linked polyethylene. To date, this balance has not been determined.
METAL ON METAL
Of all the alternative bearings, metal on metal has data with the longest follow-up period, with clinical data available on the McKee–Farrar prosthesis for nearly 30 years of follow-up.33 Currently, there are two main iterations of the metal-on-metal articulation in North America: a modular metal insert that fits into a traditional press-fit shell, or a surface replacement metal head that articulates against nonmodular acetabular components.
Metal-on-metal articulations have the most complex tribology of the alternative bearings. The wear properties are dependent on the exact composition of the alloy used, the size of the articulation, the time after implantation, and the clearance between the components. In simulator studies, high-carbon alloys have been compared with low-carbon alloys with the findings that low-carbon alloys had a six times greater volumetric wear rate than high-carbon alloys.33 From this observation, the investigators recommend that low-carbon alloys should not be used in metal-on-metal articulations. This has been supported by other authors.34 Metal-on-metal articulations feature a significant running in phenomenon. In the first million cycles, the articulation has a significantly increased wear rate compared with the steady-state wear rate observed after this.35 Paradoxically, articulations of larger diameters have less volumetric wear than smaller articulations. This applies both to the wearing in and the steady-state wear rates.36 Lubrication analysis revealed that as the head size increased, the fluid film also increased, hence reducing wear.37
Radial clearance has also been examined as a contributor to volumetric wear rate. As the radial clearance increases between 20 and 150 μm and beyond, the volumetric wear in both the running-in and the steady-state phase increases. Lubrication analysis revealed that as radial clearance increased, fluid film decreased, which explains the worsening wear rates for increased radial clearance.37
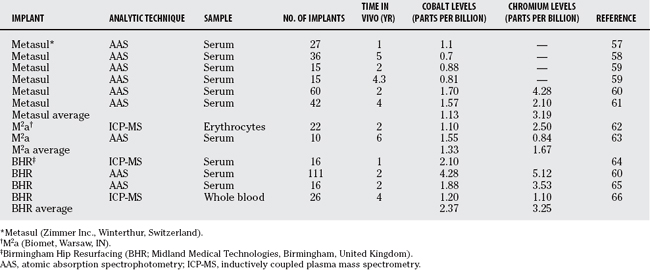
The single greatest concern with the use of metal-on-metal bearings continues to be the increased levels of metal ions measurable in patients’ blood and urine after implantation. Many studies have evaluated the circulating heavy metal ions (Table 84-1).38 There are, however, multiple complex issues associated with the analysis of metal ions, including collection techniques, analysis, statistical methodologies, and reporting of results. To date, the literature on this topic has been characterized by significant variability in all of these factors. Attempts have been made to standardize these methods.39 What then are the observed biological effects of the wear debris?
Wear debris from metal-on-metal articulations is in the nanometer size range, and these particles have been found to be cytotoxic to cells at volumes of 5 μm3/cell and greater.40 Necrosis has been observed histologically around retrieved implants of both historical and modern design.41 This cytotoxic effect of the wear debris to the local tissue remains of concern to users of metal-on-metal articulations. Concerns are also raised about the effect of elevated heavy metal ions in remote tissues to the hip replacement. Both chromium and cobalt levels are increased above baseline with metal-on-metal articulations.35,42 Concerns have also been expressed about potential metal ion carcinogenicity. More than 700,000 metal-on-metal total hip arthroplasties have been performed globally with no causal links to cancer.43,44 Metal wear debris also may cause inflammatory or allergic local tissue reactions in some individuals. This may lead to pain at the site of implantation from synovitis or implant loosening.45
These potential adverse biological effects of metal-on-metal articulations are the rationale behind ongoing research into novel hard-bearing articulations. For example, currently under investigation are a delta ceramic head on metal insert bearing, and the use of metal components coated with a thick layer of chromium cyanide (CrCN). Both ceramic-on-metal and the CrCN-coated metal-on-metal articulations have volumetric wear rates 10 to 100 times less than metal-on-metal articulations of the same diameter head size.46–48 The improvement observed with the ceramic-on-metal articulation is thought to be because of the differential hardness of the metal and the ceramic, and the smoother surface and improved lubrication that ceramics offer. The wear debris from the CrCN-coated bearings was also found to be more biocompatible and less cytotoxic than the metallic debris.49
CERAMIC ON CERAMIC
Ceramic-on-ceramic articulations in simulated wear testing outperform other articulations. Volumetric wear rates for ceramic-on-ceramic articulations using traditional hip simulators have been as low as 0.1 mm3/million cycles.37 To put this in perspective, this is about 350 times lower than the volumetric wear rates of metal on conventional polyethylene and 50 times less than the volumetric wear rate of metal on cross-linked polyethylene. Unfortunately, these wear rates have not been observed in clinical retrieval studies of worn ceramic on ceramic articulations. As the hip moves in vivo, the femoral head does not stay in the exact center of the joint at all times through the gait cycle, and at times may come in contact with the rim of the cup. Standard hip simulators have not been able to replicate the stripe wear that is seen on retrieved femoral heads.50 Thus, a microseparation hip simulator has been developed that replicates the stripe wear seen on retrieved femoral heads. Volumetric wear rates of 1.4 mm3/million cycles have been observed using this simulator.51 These observations are consistent with retrieval studies of ceramicon-ceramic articulations.37 Comparing these results with other bearings, the ceramic-on-ceramic articulation produces 25 times less debris than conventional polyethylene and 4 times less debris than highly cross-linked polyethylene.37 In vivo, ceramic-onceramic bearings produce similar volumetric wear to metal-on-metal bearings when the metal-on-metal bearing has finished running in and is within its steady-state wear.
When examining the functional biological activity of the debris from the microseparation hip simulator in the same way that the debris of polyethylene articulations was analyzed, there was a bimodal distribution of particle size in the ceramic debris: nanometer-sized debris from the normal articulation surfaces and micron-sized debris from grain boundary failure and pull out from the regions of stripe wear.52 When this debris was cultured with human macrophages, measured tumor necrosis factor-α production produced a specific biological activity of 0.18. When combined with volumetric wear, substantially lower functional biological activity is derived for ceramic-on-ceramic articulations than either conventional polyethylene (80 times lower) or cross-linked polyethylene (20 times lower).37 This lower functional biological activity is reflected in retrieval studies where there has been a low incidence of osteolysis.53
Ceramics are brittle materials. A real risk exists for fracturing one of the components if the component dislocates or if the neck of the femoral component impinges on the rim of the acetabular insert.54 There have also been reports of spontaneous fracture of ceramic femoral heads (zirconia heads).54 Modern ceramics have a fracture risk rate of 0.004%54 (Level of Evidence III). One of the theoretical concerns that this raises is that when there is a ceramic fracture, the bearing used for the revision should also be ceramic because the hardness of the residual fragments after revision will cause accelerated wear because of third body wear in either a metal-on-metal or a metal-on-polyethylene articulation. When the ceramic fractures, damage may also occur to the femoral trunnion, which then may necessitate removal of a well-fixed femoral stem because the morse taper may be too damaged for another modular head to be implanted on it.54
Another complication that occurs uniquely with ceramic-on-ceramic bearings is squeaking. For reasons yet to be determined, a small percentage of patients (0.5–7%)55,56 (Level of Evidence IV) experience a positional- or activity-related squeaking noise arising from their articulation. This can be unsettling for the patient and rarely may necessitate a revision. Squeaking does not appear to be a problem with metal-on-metal articulations because when squeaking does occur, it is usually only a temporary phenomenon during the metal-on-metal bearing run-in period. More information, however, is needed to understand more fully the squeaking phenomenon in both ceramic-on-ceramic and metal-on-metal bearing couples.
The 2000s has seen a significant improvement in the materials and options that are available for use as articulating surfaces in total hip arthroplasty. Currently, most of the commercially available bearings have only short- to mid-term follow-up, but results to date are encouraging. Long-term follow-up is, however, required to confirm in vivo results will replicate in vitro data. There continues to be much ongoing work in the improvement of current bearing materials, as well as the evaluation of potential newer bearing couples. Table 84-2 summarizes the levels of evidence for bearing surfaces.
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION | REFERENCES |
|---|---|---|
UHMWPE, ultra-high-molecular-weight polyethylene.
1 Callaghan JJ, Templeton JE, Liu SS, et al. Results of Charnley total hip arthroplasty at a minimum of thirty years. A concise follow-up of a previous report. J Bone Joint Surg Am. 2004;86:690-695.
2 Malchau H, Garellick G, Eisler T, et al: Presidential Guest Address. The Swedish Hip Registry. Clin Orthop 441:19–29.
3 Ingham E, Fisher J. Biological reactions to wear debris in total joint replacement. Proc Inst Mech Eng. 2000;214:21-37.
4 Livermore J, Ilstrup D, Murray B. Effect of head size on the wear of the polyethylene acetabular component. J Bone Joint Surg Am. 1990;72:518-528.
5 Tipper JL, Ingham E, Hailey JL, et al. Quantitative analysis of polyethylene wear debris, wear rate and head damage in retrieved Charnley hip prostheses. J Mater Sci Mater Med. 2000;11:117-124.
6 Barbour PS, Stone MH, Fisher J. A hip joint simulator study using simplified loading and motion cycles generating physiological wear paths and rates. Proc Inst Mech Eng. 1999;213:455-467.
7 Barbour PS, Stone MH, Fisher J. A hip joint simulator study using new and physiologically scratched femoral heads with ultra-high molecular weight polyethylene acetabular cups. Proc Inst Mech Eng. 2000;214:569-576.
8 Schmalzried TP, Szuszczewicz ES, Northfield MR, et al. Quantitative assessment of walking activity after total hip and total knee replacement. J Bone Joint Surg Am. 1998;80:54-58.
9 Crowninshield RD, Maloney WJ, Wentz DH, et al. Biomechanics of large diameter heads. Clin Orthop Relat Res.; 429; 2004; 102-107.
10 Fisher J. Wear of joint replacements. In: Shanbhag A, Rubash HE, Jacobs JJ, editors. Joint Replacement and Bone Resorption—Pathology, Biomaterials and Clinical Practice. New York: Taylor and Francis; 2006:145-169.
11 Heisel C, Silva M, Schmalzried TP. Bearing surface options for total hip replacements in young patients. Instr Course Lect. 2004;53:49-65.
12 Chan FW, Bobyn JD, Medley JB. Engineering issues and wear performance of metal on metal hip implants. Clin Orthop Relat Res.; 333; 1996; 96-107.
13 D’Lima DD, Hermida JC, Chen PC, Colwell CWJr. Polyethylene cross-linking by two different methods reduces acetabular liner wear in a hip joint wear simulator. J Orthop Res. 2003;21:761-766.
14 Jin ZM, Dowson D, Fisher J. Analysis of fluid film lubrication in artificial hip joint replacements with surfaces of high elastic modulus. Proc Inst Mech Eng [H]. 1997;211:247-256.
15 Wang A, Essner A, Schmidig G. The effects of lubricant composition on in vitro wear testing of polymeric acetabular components. J Biomed Mater Res B Appl Biomater. 2004;68:45-52.
16 Willert HG, Semliitsch M. Reactions of the articular capsule to wear products of artificial joint prostheses. J Biomed Mater Res. 1977;11:157-164.
17 Ingram JH, Stone M, Fisher J, Ingham E. The influence of molecular weight, crosslinking and counterface roughness on TNF-alpha production by macrophages in response to ultra high molecular weight polyethylene particles. Biomaterials. 2004;25:3511-3522.
18 Tipper JL, Firkins PJ, Besong AA, et al. Characterisation of wear debris from UHMWPE on zirconia ceramic, metal-on-metal and alumina ceramic-on-ceramic hip prostheses generated in a physiological anatomical hip joint simulator. Wear. 2001;250:120-128.
19 Galvin AL, Tipper JL, Ingham E, Fisher J. Nanometre size wear debris generated from crosslinked and non-crosslinked ultra high molecular weight polyethylene in artificial joints. Wear. 2005;259:977-983.
20 Hatton A, Nevelos JE, Nevelos AA, et al. Alumina-alumina artificial hip joints. Part I: A histological analysis and characterisation of wear debris by laser capture microdissection of tissues retrieved at revision. Biomaterials. 2002;23:3429-3440.
21 Tipper JL, Hatton A, Nevelos JE, et al. Alumina-alumina artificial hip joints: Part II: Characterisation of the wear debris from in vitro hip joints simulations. Biomaterials. 2002;23:3441-3448.
22 Firkins PJ, Tipper JL, Saadatzadeh MR, et al. Quantitative analysis of wear and wear debris from metal-on-metal hip prostheses tested in a physiological hip joint simulator. Biomed Mater Eng. 2001;11:143-157.
23 Green TR, Fisher J, Stone M, et al. Polyethylene particles of a “critical size” are necessary for the induction of cytokines by macrophages in vitro. Biomaterials. 1998;19:2297-2302.
24 Endo M, Tipper JL, Barton DC, et al. Comparison of wear, wear debris and functional biological activity of moderately crosslinked and non-crosslinked polyethylene in hip prostheses. Proc Inst Mech Eng [H]. 2002;216:111-122.
25 Fisher J, Bell J, Barbour PS, et al. A novel method for the prediction of functional biological activity of polyethylene wear debris. Proc Inst Mech Eng [H]. 2001;215:127-132.
26 Geerdink CH, Grimm B, Ramakrishnan R, et al. Crosslinked polyethylene compared to conventional polyethylene in total hip replacement: Pre-clinical evaluation, in-vitro testing and prospective clinical followup study. Acta Orthopaedica. 2006;77:719-725.
27 Engh CAJr, Stepniewski AS, Ginn SD, et al. A randomized prospective evaluation of outcomes after total hip arthroplasty using cross-linked marathon and non–cross-linked enduron polyethylene liners. J Arthoplasty. 2006;21(suppl 2):17-25.
28 D’Antonio JA, Manley MT, Capello WN, et al: Five-year experience with crossfire highly cross-linked polyethylene. Clin Orthop Relat Res (441):143–150.
29 Manning DW, Chiang PP, Martell JM, et al. In vivo comparative wear study of traditional and highly cross-linked polyethylene in total hip arthroplasty. J Arthroplasty. 2005;20:880-886.
30 Digas G, Kärrholm J, Thanner J, et al. Highly cross-linked polyethylene in total hip arthroplasty. Clin Orthop Relat Res. 2004;429:6-16.
31 Bradford L, Baker D, Ries MD, Pruitt LA: Fatigue crack propagation resistance of highly crosslinked polyethylene. Clin Orthop Relat Res (429):68–72.
32 Birman MV, Noble PC, Conditt MA, et al: Cracking and impingement in ultra–high-molecular-weight polyethylene acetabular liners. J Arthroplasty 20(suppl 3):87–92.
33 Brown SR, Davies WA, DeHeer DH, Swanson AB. Long-term survival of McKee-Farrar total hip prostheses. Clin Orthop Relat Res.; 402; 2002; 157.
34 Chan FW, Bobyn JD, Medley JB, et al. The Otto Aufranc Award: Wear and lubrication of metal-on metal hip implants. Clin Orthop Relat Res.; 369; 1999; 10.
35 Lhotka C, Szekeres T, Steffan I, et al. Four-year study of cobalt and chromium blood levels in patients managed with two different metal-on-metal total hip replacements. J Orthop Res. 2003;21:189-195.
36 Hu XQ, Isaac GH, Fisher J. Changes in contact area during the bedding-in of different sizes of metal on metal hip prostheses. Biomed Mater Eng. 2004;14:145-149.
37 Fisher J, Jin Z, Tipper J, et al. Tribology of alternative bearings. Clin Orthop. 2006;453:25-34.
38 MacDonald SJ. Can a safe level for metal ions in patients with metal-on-metal total hip arthroplasties be determined? J Arthroplasty. 2004;19(suppl 3):71-77.
39 MacDonald SJ, Brodner W, Jacobs JJ. A consensus paper on metal ions in metal-on-metal hip arthroplasties. J Arthroplasty. 2004;19:12-16.
40 Germain MA, Hatton A, Williams S, et al. Comparison of the cytotoxicity of clinically relevant cobalt-chromium and alumina ceramic wear particles in vitro. Biomaterials. 2003;24:469-479.
41 Doorn PE, Mirra JM, Campbell PA, Amstutz HC: Tissue reaction to metal on metal total hip prostheses. Clin Orthop Relat Res 329S:S187–S205.
42 Daniel J, Ziaee H, Pradhan C, et al. Blood and urine metal ion levels in young and active patients after Birmingham hip resurfacing arthroplasty. J Bone Joint Surg Br. 2007;89-B:169-173.
43 Visuri TI, Pulkkinen P, Paavolainen P. Malignant tumors at the site of total hip prosthesis. Analytic review of 46 cases. J Arthroplasty. 2006;21:311-323.
44 Visuri TI, Pukkala E, Pulkkinen P, Paavolainen P. Cancer incidence and causes of death among total hip replacement patients: A review based on Nordic cohorts with a specialemphasis on metal-on-metal bearings. Proc Inst Mech Eng [H]. 2006;220:399-407.
45 Jacobs JJ, Hallab J. Loosening and osteolysis associated with metal-on-metal bearings: A local effect of metal hypersensitivity? J Bone Joint Surg Am. 2006;88:1171-1172.
46 Firkins PJ, Tipper JL, Ingham E, et al. A novel low wearing differential hardness, ceramic-on-metal hip joint prostheses. J Biomech. 2001;34:1291-1298.
47 Fisher J, Hu XQ, Stewart TD, et al. Wear of surface engineered metal-on-metal hip prostheses. J Mater Sci Mater Med. 2004;15:225-235.
48 Fisher J, Hu XQ, Tipper JL, et al. An in vitro study of the reduction in wear of metal on metal hip prostheses using surface-engineered femoral heads. Proc Inst Mech Eng [H]. 2002;216:219-230.
49 Williams S, Tipper JL, Ingham E, et al. In vitro analysis of the wear, wear debris and biological activity of surface-engineered coatings for use in metal-on-metal total hip replacements. Proc Inst Mech Eng [H]. 2003;217:155-163.
50 Walter WL, Insley GM, Walter WK, Tuke MA. Edge loading in third generation alumina ceramic-on-ceramic bearings. J Arthroplasty. 2004;19:402-413.
51 Stewart T, Tipper JL, Streicher R, et al. Long-term wear or HIPed alumina on alumina bearings for THR under microseparation conditions. J Mater Sci Mater Med. 2001;12:1053-1056.
52 Tipper JL, Hatton A, Nevelos JE, et al. Alumina-alumina artificial hip joints: Part II: Characterisation of the wear debris from in vitro hip joints simulations. Biomaterials. 2002;23:3441-3448.
53 Hamadouche M, Boutin P, Daussange J, et al. Alumina-on-alumina total hip arthroplasty: A minimum 18.5-year follow-up study. J Bone Joint Surg Am. 2002;84:69-77.
54 Bierbaum BJ, Nairus J, Kuesis D, et al. Ceramic-on-ceramic bearings in total hip arthroplasty. Clin Orthop Relat Res. 2002;405:158-163.
55 Walter WL, O’Toole GC, Walter WK, et al. Squeaking in ceramic on ceramic hips. J Arthroplasty. 2007;22:496-503.
56 Jarrett C, Ranawat AS, Bruzzone M, et al: “The squeaking hip” An under reported phenomenon of ceramic on ceramic total hip arthroplasty. Presented at the Hip Society Summer Meeting; Iowa City, IA, 2006.
57 Brodner W, Bitzan P, Meisinger V, et al. Elevated serum cobalt with metal on metal articulating surfaces. J Bone Joint Surg Br. 1997;79:316.
58 Brodner W, Bitzan P, Meisinger V, et al. Serum cobalt levels after metal-on-metal total hip arthroplasty. J Bone Joint Surg Am. 2003;85:2168.
59 Savarino L, Granchi D, Ciapetti G, et al. Ion release in stable hip arthroplasties using metal-on-metal articulating surfaces: A comparison between short- and medium-term results. J Biomed Mater Res. 2003;66A:450.
60 Witzleb WC, Ziegler J, Krummenauer F, et al. Exposure to chromium, cobalt and molybdenum from metal-on-metal total hip replacement and hip resurfacing arthroplasty. Acta Orthop. 2006;77:697-705.
61 Savarino L, Greco M, Cenni E, et al. Differences in ion release after ceramic-on-ceramic and metal-on-metal total hip replacement. Medium-term follow-up. J Bone Joint Surg Br. 2006;88:472-476.
62 MacDonald SJ, McCalden RW, Chess DG, et al. Metal-on-metal versus polyethylene in hip arthroplasty: A randomized clinical trial. Clin Orthop Relat Res.; 406; 2003; 282.
63 Rasquinha VJ, Ranawat CS, Weiskopf J, et al. Serum metal levels and bearing surfaces in total hip arthroplasty. J Arthroplasty. 2006;21(6 suppl 2):47-52.
64 Clarke MT, Lee PTH, Arora A, Villar RN. Levels of metal ions after small and large diameter metal-on-metal hip arthroplasty. J Bone Joint Surg Br. 2003;85:913.
65 Back DL, Young DA, Shimmin AJ. How do serum cobalt and chromium levels change after metal-on-metal hip resurfacing?. Clin Orthop Relat Res.; 438; 2005; 177-181.
66 Daniel J, Ziaee H, Pradham C, et al. Blood and urine metal ion levels in young and active patients after Birmingham hip resurfacing arthroplasty. Four-year results of a prospective longitudinal study. J Bone Joint Surg Br. 2006;89:169-173.