Chapter 52 When Is It Safe to Resect Heterotopic Ossification?
WHAT IS HETEROTOPIC OSSIFICATIONAND WHAT CAUSES IT?
It is postulated that a circulatory factor, released from the brain, is the common factor in burn and trauma victims that leads to the growth of the HO. Much work is yet to be done to fully isolate this factor. The factors seem to be subtypes of bone morphogenetic protein (BMP), with BMP-1, −4, and −6 found in pathologic specimens.1 A correlation exists between the severity of the head injury and the risk for development of ectopic bone. The occurrence of autonomic dysregulation may predict the chance of development of HO in patients with severe head injury.2 The role of prostaglandin E2 has recently been suggested as a mediator in the differentiation of the progenitor cells.3
OPTIONS
Classic teaching has been to wait until the HO tissue is mature, until there is no further evidence of bone formation before attempting to remove it, thus minimizing the risk for HO re-formation. This traditional approach is based on the following theoretical concept: If the bone has matured and is no longer in an active stage of formation, there will be less chance of it re-forming after the resection. Although reasonable in theory, no Level I or II studies have evaluated this concept. More recently, individual surgeons are moving to earlier resection to reduce the time of disability for the patient.4
The traditional methods for assessing the maturity of the HO are as follows:
Classic orthopedic texts (Level V) recommend the following approach to HO resection: Wait at least 12 to 18 months after the HO has formed to guarantee that the tissue is mature and will not reoccur. Look at the quality of the bone on radiographs to look for the features of mature bone, density, trabecular patterns of bone, and cortical maturation. Always obtain a bone scan of the area. The bone scan must be cold—that is, showing no evidence of bone turnover or overt activity, thus assuring the surgeon that the tissue is mature and not likely to return once resected. In addition, the serum ALK should be followed until it normalizes before removing the bone.5–7
Currently, many authors believe that waiting until the radiographic appearance is reasonably mature and then proceeding with the resection is the best approach. They are hoping to reduce the morbidity of the prolonged delay to surgery and the problems of joint immobility that may not be correctable after resection. Tsionos, Leclercq, and Rochet,8 from the Institut de la Main, Paris, France, advised early resection in burn patients at the elbow with a suggested reduction of the period of morbidity for the patients (Level IV). Their mean time between the burn and operation was 12 months, with the median being 9.5 months. This chapter analyzes the literature according to levels of evidence to attempt to answer the question posed: When is it safe to resect HO?
EVIDENCE
Radiographic Appearance of Maturity
The typical radiologic appearance of HO is circumferential ossification with a lucent center.9 X-ray indicators of maturity—lesions with distinct margins and well-defined trabeculations—have not proved to be reliable predictors of nonrecurrence of HO after surgery10 (Level III).
Really only one study has been widely quoted that looks at the level of bone maturity and attempts to correlate this to the risk for bone reformation after resection. In a small, retrospective review of 19 patients with spinal cord injuries, Garland and Orwin10 found that 15 of 22 hips with a mature preoperative pattern of heterotopic bone had a recurrence after resection. No evidence was reported that a mature pattern of bone was less associated with a recurrence than one that was less mature. This is a Level III study.
Role of Alkaline Phosphatase in Assessing the Maturity of the Heterotopic Ossification
In situations in which there is the formation of large amounts of HO, ALK levels may become abnormal approximately 2 weeks after injury. In the typical case of HO, the ALK levels reached approximately 3.5 times the normal value 10 weeks after the inciting trauma, before returning to normal at approximately 18 weeks.11 Although it may seem a logical conclusion that there is a direct correlation between the level of ALK and the activity of the HO, this is not always the case. The levels of ALK may be entirely normal with active HO.10,11 Alternatively, the levels may remain increased for years after formation, yet the tissue appears completely mature on radiographs.12
The level of evidence is fair (Level II) for an association between increased ALK and the development of HO. In a prospective cohort analysis study by Tibone and coauthors,12 in which the authors gathered data on a series of patients with spinal cord injuries with developing HO, a relation between increasing levels of ALK and the development of HO was established. This study did not look at surgical resection or recurrence of the lesions after resection. The authors also found persistently increased levels of ALK in several patients for years after the development of HO, indicating that, if the level of ALK was an important parameter for determining the maturity of the HO, it might be thought that the HO might take many years to mature. In some cases, it may never be mature.
Comparing the levels of ALK and the rates of recurrence, Garland and Orwin,10 in their small retrospective series (Level III), found that serum ALK levels were normal in 9 of 13 hips that had a recurrence of bone formation after resection of the HO. Thus, little support exists for the routine use of serum ALK normalization as an indicator of the safety to proceed with resection of the HO.
BONE SCANS
Three-phase bone scans may be the most sensitive imaging modality for early detection of HO.10,11,13–19 Specifically, flow studies and blood-pool images will detect the beginnings of HO approximately 2.5 weeks after injury, with findings on delayed scintigrams becoming positive approximately 1 week later. Activity on the delayed bone scans usually peaks a few months after injury, after which the intensity of activity on these scans progressively lessens, with a return toward normal at 6 to 12 months. The scans will usually return to normal within 12 months, hence the classic suggestions to wait the 1-year period before resecting the bone. Paradoxically, in some cases, activity on the scan remains slightly increased even though the underlying HO has become mature.12
Several authors report on the use of serial bone scans to successfully monitor the metabolic activity of HO and determine the appropriate time for surgical resection, if needed, and to predict postoperative recurrence.14,15, 20, 21
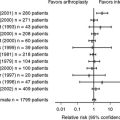
The studies evidence is summarized as follows:
Level of Neurologic Recovery
In a retrospective chart review of 25 adult patients with brain injury, Garland and coworkers23 analyzed the extent of the brain injury and the degree of recovery of the involved limb after resection of the HO (Level III). The authors categorized the patients into Class I to V according to the cognitive and physical residua of the brain injury, with Class I being minimal disability in both areas. In addition, the authors looked at the bone scans, levels of ALK, radiographic evidence of bone maturity before surgery, and use of postoperative preventive measures such as diphosphonate.
Garland13 has recommended different schedules for surgical intervention, depending on the cause of the condition underlying the HO: 6 months after direct traumatic musculoskeletal injury, 1 year after spinal cord injury, and 1.5 years after traumatic brain injury. This publication makes recommendations that the author describes as an estimate of timing without substantive evidence.
AREAS OF UNCERTAINTY
It is unclear whether what is required is a refinement of techniques to determine when the HO has matured, or whether there are other, more important factors that affect the likelihood of recurrence after surgical resection apart from the maturity of the bone mass. Little evidence is available to support the contention that radiographic assessment of HO maturity predicts the chance of reoccurrence after resection surgery10 (Level III).
For several investigators,14,20, 21 serial preoperative bone scans that quantify the ratio of heterotopic to normal bone activity have successfully predicted postoperative nonrecurrence; a decreasing or stable scintigraphic activity ratio is considered the hallmark of mature HO. As HO becomes mature, there also is a significant decrease, often reaching a normal level, in both flow study and blood-pool activity. Other authors, again based on poor level evidence, have found that even in the presence of a quiescent bone scan, a postresection reoccurrence of HO can occur (Level III).10,24
Neurologic recovery of the affected limb seems to be an important factor in reducing the chance of recurrence after resection of the HO (Level III).23 Although not specifically covered in this article, the use of appropriate postoperative measures to reduce the chances of recurrence, be this radiation treatment, use of anti-inflammatory drugs such as indomethacin or cyclo-oxygenase-2 inhibitors, or a combination of the two, may well be more important than the above preoperative indices in achieving a successful outcome from resection surgery.
Based on a critical review of the available literature with an assessment of the quality of the studies, the assessment of when it is safe to resect HO remains difficult. Table 52-1 provides a summary of recommendations for the treatment of heterotopic ossification.
| RECOMMENDATION | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
HO, heterotopic Ossification.
1 Liu K, Tripp S, Layfield LJ. Heterotopic ossification: Review of histologic findings and tissue distribution in a 10-year experience. Pathol Res Pract. 2007;203:633-640.
2 Hendricks HT, Geurts AC, van Ginneken BC, et al. Brain injury severity and autonomic dysregulation accurately predict heterotopic ossification in patients with traumatic brain injury. Clin Rehabil. 2007;21:545-553.
3 Ho SSW, Stern PJ, Bruno LP, et al. Pharmacological inhibition of prostaglandin E-2 in bone and its effect on pathological new bone formation in a rat brain model. Trans Orthop Res Soc. 1988;13:536.
4 Freebourn TM, Barber DB, Able AC. The treatment of immature heterotopic ossification in spinal cord injury with combination surgery, radiation therapy and NSAID. Spinal Cord. 1999;37:50-53.
5 Canale ST. Campbell’s Operative Orthopedics, 10th ed. St. Louis: Mosby, 2003.
6 Bucholz RW, Heckman JD. Rockwood and Green’s Fractures in Adults, 6th ed. Philadelphia: Lippincott Williams & Wilkins, 2005.
7 Weinstein SL, Buckwalter JA. Turek’s Orthopaedics: Principles and Their Application, 6th ed. Philadelphia: Lippincott William & Wilkins, 2005.
8 Tsionos I, Leclercq C, Rochet JM. Heterotopic ossification of the elbow in patients with burns: Results after early resection. J Bone Joint Surg Br. 2004;86-B:396-403.
9 Helms CA. “Skeletal don’t touch” lesions. In: Brant WE, Helms CA, editors. Fundamentals of Diagnostic Radiology. Baltimore, MD: Williams & Wilkins; 1994:963-975.
10 Garland DE, Orwin JF. Resection of heterotopic ossification in patients with spinal cord injuries. Clin Orthop. 1989;242:169-176.
11 Orzel JA, Rudd TG. Heterotopic bone formation: Clinical, laboratory and imaging correlation. J Nucl Med. 1985;26:125-132.
12 Tibone J, Sakimura I, Nickel VL, Hsu JD. Heterotopic ossification around the hip in spinal cord-injured patients: A long-term follow-up study. J Bone Joint Surg Am. 1978;60:769-775.
13 Garland DE. A clinical perspective on common forms of acquired heterotopic ossification. Clin Orthop. 1991;263:13-29.
14 Rossier AB, Bussat P, Infante F, et al. Current facts on para-osteoarthropathy (POA). Paraplegia. 1973;11:36-78.
15 Freed JH, Hahn H, Menter R, Dillon T. The use of three-phase bone scan in the early diagnosis of heterotopic ossification (HO) and in the evaluation of Didronel therapy. Paraplegia. 1982;20:208-216.
16 Tyler JL, Derbekyan V, Lisbona R. Early diagnosis of myositis ossificans with Tc-99m diphosphonate imaging. Clin Nucl Med. 1984;9:256-258.
17 Drane WE. Myositis ossificans and the three phase bone scan. AJR Am J Roentgenol. 1984;142:179-180.
18 Szabo Z, Ritzl F, Chittima S, et al. Bone scintigraphy of myositis ossificans in apallic syndrome. Eur J Nucl Med. 1982;7:426-428.
19 Suzuki Y, Hisada K, Takeda M. Demonstration of myositis ossificans by 99mTc pyrophosphate bone scanning. Radiology. 1974;111:663-664.
20 Muheim G, Donath A, Rossier AB. Serial scintigrams in the course of ectopic bone formation in paraplegic patients. AJR Am J Roentgenol. 1973;118:865-869.
21 Tanaka T, Rossier AB, Hussey RW, et al. Quantitative assessment of para-osteo-arthropathy and its maturation on serial radionuclide bone images. Radiology. 1977;123:217-221.
22 Stover SL, Niemann KM, Tulloss JR. Experience with surgical resection of heterotopic bone in spinal cord injury patients. Clin Orthop. 1991;263:71-77.
23 Garland DE, Hanscom DA, Keenan MA, et al. Resection of heterotopic ossification in the adult with head trauma. J Bone Joint Surg Am. 1985;67:1261-1269.
24 Garland DE. Surgical approaches for resection of heterotopic ossification in traumatic brain-injured adults. Clin Orthop Relat Res.; 263; 1991; 59-70.