Chapter 86 What Is the Role for Hip Resurfacing Arthroplasty?
Hip resurfacing is a technique that has re-emerged since the late 1990s. Hip resurfacing using different methods of fixation and different bearing surfaces have previously been unsuccessful. The experience with the Wagner resurfacing in the early 1980s was reported by Bell and coauthors1 in their study of implant failures with the Wagner resurfacing. They note that loosening was associated with the development of a membrane at the bone-cement interface. This histologic examination of the membrane demonstrated foreign body response to wear products from the arthroplasty. This suggested that the bearing materials used in this second generation of resurfacing devices was a major factor in the high early failure rate.2
The high volumetric of polyethylene of the earlier designs led several investigators to simultaneously and independently investigate in the early 1990s the use of metal-on-metal (MOM) bearing surfaces.3,4 The bearings designed during the 1990s have proved more durable and are the subject of this review.
Hip resurfacing arthroplasty is an increasingly popular hip arthroplasty option for young, active patients who will likely loosen a conventional total hip replacement (THR) prosthesis. THR has proved to be highly effective in elderly and less active patients, who can expect an implant failure rate less than 10% at 10 years after surgery.5 These excellent results, however, are not observed in younger, more active recipients of THR, who routinely put significant strain on their hip prosthesis during work and recreational pursuits. In these patients, implant failure rates of 25% to 30% have been reported at 15 years.6 This is likely caused by an active lifestyle that contributes to excessive wear, osteolysis, and loosening of the implant.7,8
EVIDENCE
Systematic Reviews
At this time, there are two Level IV systematic reviews available on the outcomes of hip resurfacing arthroplasty. The systematic review by Vale and colleagues9 compared the reported outcomes of hip resurfacing with other treatments including THR. This review included 20 articles (1990–2001) that met the inclusion criteria, which included study patients who were active and younger than 65 years, and who would likely outlive a THR. Hip resurfacing revision rates were found to range from 0% to 14% over a 3-year follow-up period compared with THR revision rates of 10% or less over a 10-year period. Furthermore, 91% of patients with hip resurfacing were reported to be pain free at 4-year follow-up evaluation, compared with 84% at 11 years for patients with THRs. Unfortunately, that review was limited to eight case series reports of hip resurfacing outcomes. Hence, no comparative studies were available that directly compared hip resurfacing with THR.
Wyness and researchers10 provide a follow-up systematic review on the effectiveness of hip resurfacing based on studies published before 2002 (Level IV). This review includes data from four hip resurfacing studies, four THR studies, and one watchful waiting study. In addition, the authors include three unpublished hip resurfacing studies supplied from manufacturers for analysis. Unfortunately, similar to Vale and colleagues’9 review, no comparative studies were available to this systematic review. The studies included in this review rate poorly for study description and for controlling bias. Of the hip resurfacing reports, revision rates were between 0% and 14.3% over a follow-up range of 8.3 to 48 months.
Prospective, Randomized Studies
One prospective, randomized, controlled trial (RCT)11 has assessed outcomes after modern hip resurfacing with THR. Howie and coauthors12 also report a hip resurfacing RCT that featured 24 patients 55 years or younger. That study compared the outcomes of 11 patients who randomly received McMinn resurfacing devices with 13 patients with THR. The surgeries were performed between 1993 and 1995, and unlike current hip resurfacing techniques, cement fixation of the acetabular component was used. An extremely high revision rate of 73% was observed in the resurfacing group, which contributed to the abandonment of cement fixation for the acetabular component.
Vendittoli and coworkers’11 RCT compares the clinical outcomes of patients with hip resurfacing (107 hips) with THR (103 hips) over a study period from 2003 to 2006. The average age of the hip resurfacing group (49.1 years; range, 23–64 years) was similar to that of the THR group (50.6 years; range, 24–65 years), although the hip resurfacing group had a lower body mass index (27.2 vs. 29.6) than the THR group. Osteoarthritis was the primary diagnosis for all patients, and outcome measures included the, Western Ontario and McMaster Universities (WOMAC) index, Postel-Merle-d’Aubigne (PMA) functional assessment, and the UCLA activity score. This RCT found that hip resurfacing, compared with THR, took longer operating time (101 vs. 85 min) and resulted in shorter length of hospital stay (5.0 days vs. 6.1 days). At 1-year follow-up examination, WOMAC and PMA scores were similar for both groups, although patients with hip resurfacing had greater average UCLA activity scores. Vendittoli and coworkers11 also note that more resurfacing patients returned to work and resumed heavy or moderate activities at 1-year follow-up compared with the THR group. No dislocations or femoral neck fractures were observed in the resurfacing group, although two cases of femoral aseptic loosening led to revision surgery (one at 6 months and the other at 9 months after surgery). In the THR group, one revision was performed for recurrent dislocation. Those authors conclude that hip resurfacing and THR result in similar satisfaction rates in young patients, but hip resurfacing may give better functional performance in terms of activity level and capacity to return to work. Although this RCT is the best experimental study conducted to date on hip resurfacing, it is limited by its short-term follow-up period.
HIP RESURFACING OUTCOMES
Implant Survival Rates
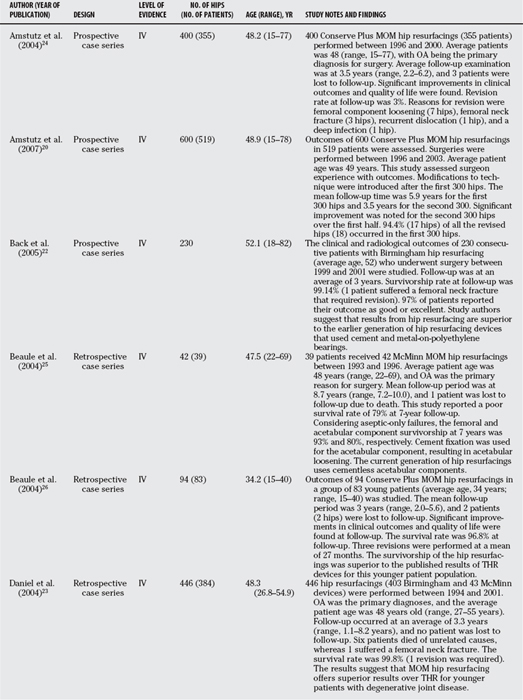
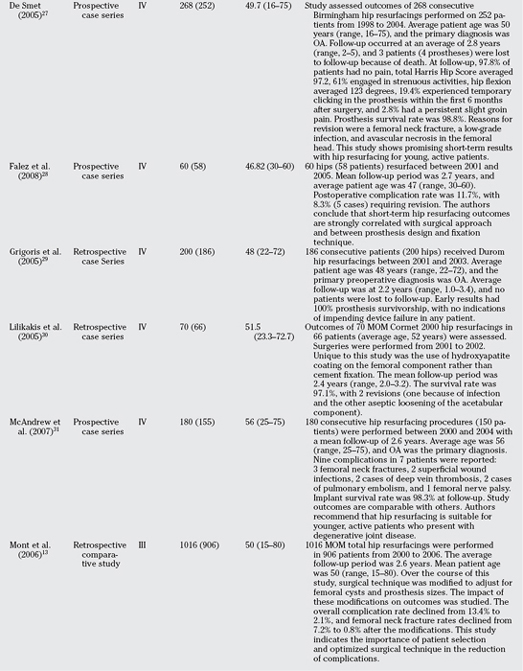
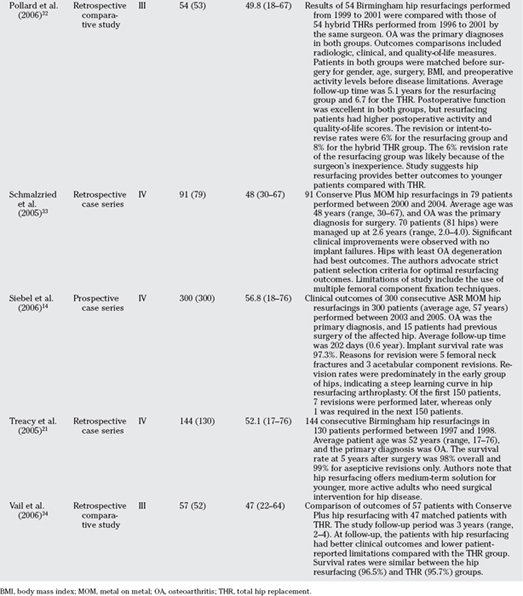
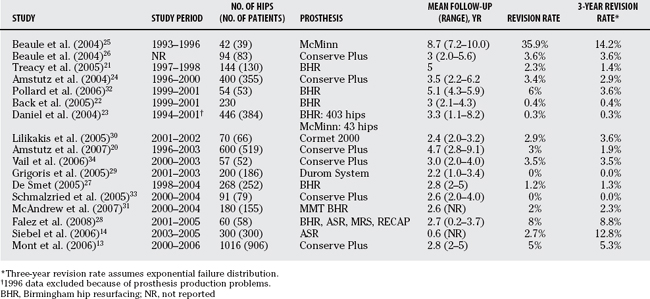
Currently, there are no long-term outcomes on revision rates for the current generation of hip resurfacings. Reported short-term outcomes of up to 5 years after surgery have indicated various rates of revision (see Table 86-1). We summarized the revision rates for these studies as the overall revision rates per 100 hip-years of follow-up. We used a Poisson distribution to determine the rates after first testing for overdispersion of study rates using a negative binomial distribution. We used hip-time of follow-up as an offset in estimating the failure rate. At the 5% level of significance, there was no evidence of overdispersion among the rates. The overall rate per 100 hip-years of follow-up was 0.99 (95% confidence interval, 0.83–1.17).
Table 86-2 provides a summary of the revision rates and study duration reported in comparative and case series hip resurfacing studies. In addition, it includes the 3-year revision rates for each study based on an exponential failure distribution. Numerous factors contribute to the variance in revision rates reported in the literature. These include surgeon experience13,14 and appropriate patient selection.
Adverse Events
The major complication after MOM hip resurfacing is femoral neck fracture. This contributes to the earlier revision rate noted with hip resurfacing when compared with total hip arthroplasty. The overall incidence rate of femoral neck fracture as reported by Shimmin and Back15 is 1.46%. The incidence rate for women is 1.91% and for men is 0.98%. The mean time to fracture was 15.4 weeks. Significant varus placement of the femoral component and intraoperative notching of the femoral neck were predisposing factors in 85% of cases.
Implant Wear and Metal Ion Effects
The advent of MOM arthroplasty has led to an increased concern about the consequence of metal ion debris with respect to both toxicity and carcogenicity. Keegan and coauthors’16 review article outlines the potential toxicities of metal ions. Visuri and investigators’17 work shows no increase in the cancer rate on long-term follow-up of patients with MOM total joint arthroplasty. However, because the event rate is low, the literature must be considered inconclusive on this issue. No evidence exists for an increased risk for cancer with the ion levels that are currently seen in clinical practice. Further surveillance is required.
A major drawback with metal-on-polyethylene hip arthroplasty devices is their wear profile and subsequent release of polyethylene particles into the joint. This wear debris is believed to be a significant cause of osteolysis and long-term implant failure.18,19
MOM bearings for THR and hip resurfacing are becoming increasingly popular because of their improved wear characteristics. The literature shows considerable variation in revision rates for MOM resurfacing. Much of this is due to variation in study durations, and when we interpolated 3-year rates using an exponential failure distribution, the rates ranged from 0% to 14.2%. Early articles reported greater revision rates than typically seen with THRs because of the early occurrence of femoral neck fractures leading to conversion to total hip arthroplasty. Reports by experienced surgeons20–23 (Level IV) showed excellent midterm results with lower projected revision rates than that for THR as reported by the Swedish Joint Replacement Registry. Reported results from the Australian registry show an acceptable midterm survivorship of several of the resurfacing systems, surpassing the reports of a high failure rate for the Wagner resurfacing system by midterm assessment. The greater earlier failure rate is largely a consequence of femoral neck fracture. Based on Shimmin and Back’s15 analysis, many of the fractures were as a consequence of technical error. Appropriate physician training, attention to intraoperative detail, and careful patient selection to avoid patients with poor bone quality should lead to a reduction in the postoperative rate of femoral neck fracture. The authors recommend continued study of the outcome of resurfacing and surveillance for possible adverse consequences of increased metal ion levels. Resurfacing arthroplasty shows great promise in young adults with osteoarthritis who have a high functional demand and when performed by an experienced surgeon. Table 86-3 provides a summary of recommendations.
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATIONS |
|---|---|
| Resurfacing arthroplasty may have a role in young adults. | I |
1 Bell RS, Schatzker J, Fornasier VL, et al. A study of implant failure in the Wagner resurfacing arthroplasty. J Bone Joint Surg Am. 1985;67:1165-1175.
2 Howie DW, Campbell D, McGee M, et al. Wagner resurfacing hip arthroplasty. The results of one hundred consecutive arthroplasties after eight to ten years. J Bone Joint Surg Am. 1990;72:708-714.
3 Schmalzried TP, Fowble VA, Ure KJ, et al. Metal on metal surface replacement of the hip. Technique, fixation, and early results. Clin Orthop Relat Res.; 329 suppl; 1996; S106-S114.
4 McMinn D, Daniel J. History and modern concepts in surface replacement. Proc Inst Mech Eng [H]. 2006;220:239-251.
5 Malchau H, Herberts P, Eisler T, et al. The Swedish Total Hip Replacement Register. J Bone Joint Surg Am. 2002;84-A(suppl 2):2-20.
6 Northmore-Ball MD. Young adults with arthritic hips. BMJ. 1997;315:265-266.
7 Crowther JD, Lachiewicz PF. Survival and polyethylene wear of porous-coated acetabular components in patients less than fifty years old: Results at nine to fourteen years. J Bone Joint Surg Am. 2002;84-A:729-735.
8 Duffy GP, Berry DJ, Rowland C, et al. Primary uncemented total hip arthroplasty in patients <40 years old: 10- to 14-year results using first-generation proximally porous-coated implants. J Arthroplasty. 2001;16:140-144.
9 Vale L, Wyness L, McCormack K, et al. A systematic review of the effectiveness and cost-effectiveness of metal-on-metal hip resurfacing arthroplasty for treatment of hip disease. Health Technol Assess. 2002;6:1-109.
10 Wyness L, Vale L, McCormack K, et al. The effectiveness of metal on metal hip resurfacing: A systematic review of the available evidence published before 2002. BMC Health Serv Res. 2004;4:39.
11 Vendittoli PA, Lavigne M, Roy AG, et al. A prospective randomized clinical trial comparing metal-on-metal total hip arthroplasty and metal-on-metal total hip resurfacing in patients less than 65 years old. Hip International. 2006;16:S73-S81.
12 Howie DW, McGee MA, Costi K, et al. Metal-on-metal resurfacing versus total hip replacement: The value of a randomized clinical trial. Orthop Clin North Am. 2005;36:195-201. ix
13 Mont MA, Ragland PS, Etienne G, et al. Hip resurfacing arthroplasty. J Am Acad Orthop Surg. 2006;14:454-463.
14 Siebel T, Maubach S, Morlock MM. Lessons learned from early clinical experience and results of 300 ASR hip resurfacing implantations. Proc Inst Mech Eng [H]. 2006;220:345-353.
15 Shimmin AJ, Back D. Femoral neck fractures following Birmingham hip resurfacing: A national review of 50 cases. J Bone Joint Surg Br. 2005;87:463-464.
16 Keegan GM, Learmonth ID, Case CP. Orthopaedic metals and their potential toxicity in the arthroplasty patient: A review of current knowledge and future strategies. J Bone Joint Surg Br. 2007;89:567-573.
17 Visuri T, Pukkala E, Paavolainen P, et al. Cancer risk after metal on metal and polyethylene on metal total hip arthroplasty. Clin Orthop Relat Res.; 329 suppl; 1996; S280-S289.
18 Schmalzried TP, Jasty M, Harris WH. Periprosthetic bone loss in total hip arthroplasty. Polyethylene wear debris and the concept of the effective joint space. J Bone Joint Surg Am. 1992;74:849-863.
19 Schmalzried TP, Kwong LM, Jasty M, et al. The mechanism of loosening of cemented acetabular components in total hip arthroplasty. Analysis of specimens retrieved at autopsy. Clin Orthop Relat Res. 1992:60-78.
20 Amstutz HC, Le Duff MJ, Campbell PA, et al. The effects of technique changes on aseptic loosening of the femoral component in hip resurfacing. Results of 600 Conserve Plus with a 3 to 9 year follow-up. J Arthroplasty. 2007;22:481-489.
21 Treacy RB, McBryde CW, Pynsent PB. Birmingham hip resurfacing arthroplasty. A minimum follow-up of five years. J Bone Joint Surg Br. 2005;87:167-170.
22 Back DL, Dalziel R, Young D, et al. Early results of primary Birmingham hip resurfacings. An independent prospective study of the first 230 hips. J Bone Joint Surg Br. 2005;87:324-329.
23 Daniel J, Pynsent PB, McMinn DJ. Metal-on-metal resurfacing of the hip in patients under the age of 55 years with osteoarthritis. J Bone Joint Surg Br. 2004;86:177-184.
24 Amstutz HC, Beaule PE, Dorey FJ, et al. Metal-on-metal hybrid surface arthroplasty: Two to six-year follow-up study. J Bone Joint Surg Am. 2004;86-A:28-39.
25 Beaule PE, Le DM, Campbell P, et al. Metal-on-metal surface arthroplasty with a cemented femoral component: A 7-10 year follow-up study. J Arthroplasty. 2004;19:17-22.
26 Beaule PE, Dorey FJ, Leduff M, et al. Risk factors affecting outcome of metal-on-metal surface arthroplasty of the hip. Clin Orthop Relat Res. 2004:87-93.
27 De Smet KA. Belgium experience with metal-on-metal surface arthroplasty. Orthop Clin North Am. 2005;36:203-213. ix,
28 Falez F, Favetti F, Casella F, et al. Hip resurfacing: Why does it fail? Early results and critical analysis of our first 60 cases. Int Orthop. 2007;32:209-216.
29 Grigoris P, Roberts P, Panousis K, et al. The evolution of hip resurfacing arthroplasty. Orthop Clin North Am. 2005;36:125-134. vii,
30 Lilikakis AK, Vowler SL, Villar RN. Hydroxyapatite-coated femoral implant in metal-on-metal resurfacing hip arthroplasty: Minimum of two years follow-up. Orthop Clin North Am. 2005;36:215-222. ix,
31 McAndrew AR, Khaleel A, Bloomfield MD, Aweid A. A District General Hospital’s Experience of hip resurfacing. Hip International. 2007;17:1-3.
32 Pollard TC, Baker RP, Eastaugh-Waring SJ, et al. Treatment of the young active patient with osteoarthritis of the hip. A five- to seven-year comparison of hybrid total hip arthroplasty and metal-on-metal resurfacing. J Bone Joint Surg Br. 2006;88:592-600.
33 Schmalzried TP, Silva M, de la Rosa MA, et al. Optimizing patient selection and outcomes with total hip resurfacing. Clin Orthop Relat Res. 2005;441:200-204.
34 Vail TP, Mina CA, Yergler JD, et al. Metal-on-metal hip resurfacing compares favorably with THA at 2 years followup. Clin Orthop Relat Res. 2006;453:123-131.