Chapter 18 What Is the Optimal Treatment of Displaced Midshaft Clavicle Fractures?
Clavicle fractures most commonly occur in young active individuals as a result of a direct blow to the shoulder that produces axial compression of the bone. They account for approximately 2.6% of all fractures and are seen in most fracture clinics in large numbers. The most common type of injury is a fracture that occurs in the middle third (or midshaft) of the clavicle; this accounts for approximately 80% of all clavicle fractures and is the focus of this chapter. Proximal and distal third fractures are distinctly different entities with widely disparate mechanisms of injury, treatment methods, and prognoses; they are not discussed in this chapter. Even when significantly displaced, midshaft clavicle fractures traditionally have been treated without surgery. This treatment strategy was based on early reports suggesting that clavicular nonunion was extremely rare after nonoperative treatment, with an incidence rate of 0.1% to 1.0%.1–3 Similarly, clavicular malunion was described as being of radiographic interest only with no clinical significance.1–3
However, recent studies that are restricted to completely displaced midshaft fractures in adults (the focus of this chapter), that use patient-oriented outcome measures, and that have improved follow-up dispute this generally accepted orthopedic dogma.4–8 Nonunion rates between 11% and 21% have been reported, which are exponentially greater than described previously. Also, a significant proportion of patients with healed fractures but ongoing symptomatology have been described: It would appear that clavicular malunion is a distinct clinical entity with characteristic clinical and radiographic features.9,10 A variety of potential explanations has been proposed to explain this change, including survival of critically injured trauma patients with more severe fracture patterns, increased patient expectations, more complete follow-up (including patient-oriented outcome measures), and eliminating children (with their inherently good prognosis) from studies.4–11
Sufficient evidence now exists to conclude that the results of closed treatment are much inferior to what has been reported previously. Because there are numerous recent studies that support the safety and efficacy of primary operative fixation for completely displaced midshaft clavicle fractures,12–14 a discussion of the advantages and disadvantages of operative versus nonoperative treatment is warranted to augment what heretofore would have been a short chapter.
OPTIONS
Nonoperative Treatment
For centuries, attempts have been made to obtain and maintain “closed reduction” of displaced clavicular fractures, and literally hundreds of casts, splints, slings, and wraps have been described. Unfortunately, currently, no convincing evidence exists that any significant improvement can be made to the original position of the fracture. The “figure-of-eight” bandage has been popular in North America for many years, but no convincing clinical evidence is available that a closed reduction of a displaced clavicle fracture can be maintained by this device. The other popular nonoperative method is simple sling immobilization, followed by early motion. Andersen and colleagues15 performed a randomized, clinical trial comparing a sling versus a figure-of-eight bandage for displaced clavicular shaft fractures. The study revealed no functional or radiographic difference between the two groups at final follow-up, and in general, patients favored the sling. Because no significant difference exists between the two groups, both forms of nonoperative treatment are amalgamated as “nonoperative treatment” for the purposes of this chapter.
Operative Treatment
Currently, two basic operative techniques exist for the fixation of displaced midshaft fractures of the clavicle. Arguably, the most popular method is open reduction and plate fixation. This technique has been well described, has a proven track record, and with modern implants, surgical techniques, and soft-tissue handling, has a high success rate and low complication rate.12–14 For example, Smith and colleagues16 report union in 30 of 30 cases treated in this manner in a prospective trial. The disadvantages of this technique include the prominence of the plate and potential wound complications from the soft-tissue dissection required. However, with newly available precontoured plates (as opposed to the straight plates used previously), this has become less of a problem. Some authors recommend the use of anterior-inferior placement of the plate as a means of decreasing local irritation (as well as avoiding neurovascular structures while drilling).17 For the purposes of this chapter, open reduction and plating are considered as a single group (whether superior or anterior-inferior).
The second method that is discussed is intramedullary pinning of the clavicle. Although it is intrinsically difficult to perform intramedullary fixation of a curved bone with a straight intramedullary device, it is possible. The advantages of this technique include minimal soft-tissue dissection at the fracture site, less soft-tissue prominence of the hardware, and in some applications of this technique, the ability to remove the hardware relatively early through a small incision.18–23 Chuang and coauthors23 report success in 30 of 31 midshaft clavicle fractures treated with closed reduction and an intramedullary screw technique. Disadvantages of this technique, common to any unlocked intramedullary device, include difficulty in controlling shortening and rotation, especially in comminuted fractures. This led to a high rate of loss of reduction in one prospective, randomized study.22
EVIDENCE
Nonoperative Treatment
Whereas prior reports had described generally favorable results after nonoperative care of displaced midshaft fractures of the clavicle, Hill, McGuire, and Crosby’s7 landmark study published in 1997 reported a high degree of residual patient dissatisfaction. For the first time in this setting, they used a patient-based outcome tool and found that 31% of patients were dissatisfied with their outcomes, and noted a nonunion rate of 15%. Conversely, Nordqvist and coworkers8 describe good results after long-term follow-up of 225 clavicle fractures, with 185 good, 39 fair, and only 1 poor result. However, in the subcategory of displaced, comminuted fractures (the topic of the article), 27% of patients rated their shoulder as “fair,” which in the rating scale used, roughly corresponds to the dissatisfied group (31%) in Hill’s study. Another Scandinavian study by Nowak and investigators6 (the 2002 Neer Award article) found that 46% of 208 patients treated without surgery still had shoulder sequelae at 9- to 10-year follow-up. They found that comminution and displacement correlated with poor outcome. These and other nonoperative studies were summarized in a recent meta-analysis (see Comparative Studies section later in this chapter).
Operative Treatment
Initial reports regarding operative fixation of displaced clavicular fractures were plagued by selection bias (only the worst, comminuted, open fractures received surgery), poor soft-tissue handling, lack of antibiotic coverage (with correspondingly high infection rates), and especially inadequate or suboptimal fixation methods (i.e., cerclage wires or short, weak plates).1–3 Thus, not surprisingly, operative failure rates were high and fixation was avoided. More recent articles with improved techniques have conclusively proved that properly performed, primary operative repair of displaced midshaft clavicle fractures is a safe, reliable technique with a low complication rate. Collinge and coworkers17 report union in 39 of 42 cases treated with anterior/inferior plating, whereas Poigenfurst and coauthors12 report similarly favorable results in 122 consecutive cases treated with superior plating. A summary of the results of operative fixation is given in the following section.
Comparative Studies
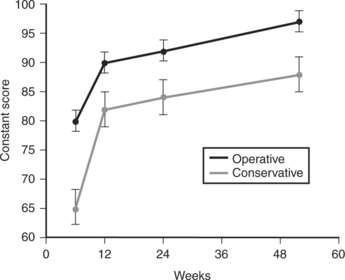
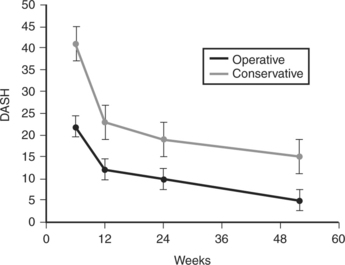
Despite the high numbers of clavicle fractures seen in clinical practice, a paucity of high-quality comparative studies is available for review. One of the few randomized clinical trials reported was recently completed by the Canadian Orthopaedic Trauma Society (COTS). They randomized 132 patients with completely displaced fractures of the midshaft clavicle to nonoperative (sling) versus operative (open-reduction and plate-fixation) treatment.24 Follow-up of 111 patients at a year after injury revealed significantly improved Constant and DASH scores in the operative group (Figs. 18-1 and 18-2). Also, there were fewer nonunions (2/62 vs. 7/49; P 5 0.042) and symptomatic malunions (0/62 vs. 9/49; P 5 0.001) in the operative group. There were complications specific to the operative group (hardware removal, five cases; infection, three cases), but these usually responded to a single repeat operative procedure. Similar findings were reported by Smith and colleagues,16 who, in a prospective randomized trial, found that open reduction and plate fixation resulted in union of 30 of 30 cases, whereas the nonoperative group had 12 nonunions in 35 cases (P 5 0.001). These authors conclude that plate fixation was safe, effective, and superior to nonoperative care for preventing nonunion. However, they did note a 30% rate of hardware removal; this study took place before precontoured plates were readily available.
Only one randomized prospective trial compares nonoperative care with intramedullary fixation of displaced clavicle fractures. These data were presented in 2005 and noted that although shoulder outcome scores were similar at 1 year (93 for operative vs. 98 for nonoperative), complications were significantly greater in the operative group.22 This included nonunion, refracture, infection, and pin prominence. However, almost half the patients in the operative group lost some of the original reduction, indicating fixation was suboptimal. A similar study, retrospective in nature, compared nonoperative (figure-of-eight bandage) versus operative (intramedullary pin fixation) treatment.21 Again, although there were no significant differences in shoulder scores (85 for nonoperative vs. 83 for operative) at final follow-up, there were more complications in the operative group including 8 infections, 3 refractures, 2 hardware failures, and 2 nonunions (14/40 patients, 35%). It would appear that although this technique is successful in expert hands, it is not as consistently reliable in general as compression plate fixation. This may relate to technique (it is a demanding procedure), patient selection (not ideal for comminuted fractures), or other unrecognized factors.
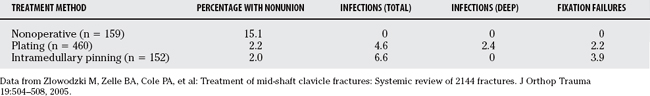
A recent meta-analysis was performed of available data from articles on midshaft clavicle fractures published between 1975 and 2005. Concentrating on data regarding displaced fractures, a nonunion rate of 15.1% was found after nonoperative care.14 The nonunion rate for plating was 2.2% and for intramedullary pinning was 2%. Thus, for displaced midshaft clavicular fractures, plating provided a relative risk reduction of 86% (95% CI, 71–93%) for nonunion compared with nonoperative care.
AREAS OF CONTROVERSY
Sling versus Figure-of-Eight Bandage
Although traditionally favored as a means of obtaining and maintaining a closed reduction of a displaced clavicle fracture, the figure-of-eight bandage was found to be equivalent to a simple sling in terms of position of fracture healing in a randomized, prospective trial that Andersen and colleagues15 conducted. In addition, patients preferred the sling (2/27 dissatisfied with sling vs. 9/34 dissatisfied with figure-of-eight bandage; P 5 0.09).
Prediction of Unsatisfactory Outcome with Nonoperative Care
It is clear that many patients with displaced midshaft fractures of the clavicle will have good results with simple nonoperative care; however, it is clear that a substantial portion will not.7–9 A goal of modern research in this field is to attempt to elicit prognostic factors that will identify individuals with an intrinsically poor outcome and then concentrate surgical resources on this group. Robinson and coauthors4 report a prospective, observational cohort study of a consecutive series of 868 patients with clavicle fractures, 581 of whom had a midshaft diaphyseal fracture. They found a significantly greater nonunion rate (21%) in displaced comminuted midshaft fractures. A letter to the editor on this article by Brinker and coworkers5 analyzing the data suggests a nonunion rate varying between 20% and 33% for displaced comminuted fractures in males. Hill and colleagues’7 study of 52 displaced midshaft clavicle fractures revealed 8 nonunions and 16 patients who described dissatisfaction with their outcome based on patient-oriented measures: They conclude that displacement of the fracture fragments by greater than 2 cm was associated with an unsatisfactory result. Nowak and investigators6 describe sequelae in 46% of patients treated without surgery 9 to 10 years after injury, and found that no bony contact (displacement), comminution, and increasing age were risk factors for a poor outcome.
Cosmesis
Although it has not traditionally been a focus of the orthopedic surgeon, it is well recognized that cosmesis is important to patients. An obvious and unsightly scar on the anterior aspect of the shoulder has been considered a deterrent to operative treatment of clavicular fractures. However, the significant shoulder asymmetry (with the typical depressed, medially translated, anteriorly rotated, “ptotic” position) that can result after a displaced fracture of the clavicle can be problematic for the modern body-image conscious patient. Several studies have addressed this question. The COTS study examined specifically the question of cosmesis, and patients were asked the question, “Are you satisfied with the appearance of your shoulder?” More patients in the operative group answered “yes” to this question than in the nonoperative group (52/62 vs. 26/49; P 5 0.001).24 Nowak and investigators’6 study of long-term follow-up of nonoperative care revealed 27% of patients who were unhappy with the appearance of their shoulder. Smith’s study16 reports that 44% of the patients in the nonoperative group “had complaints about the cosmetic appearance of their shoulder at final follow-up.” In this predominantly young population, nonoperative care can produce an unappealing “ptotic,” droopy shoulder that can be of greater cosmetic concern than a scar.
It is important to remember that the following recommendations pertain to a specific subgroup of clavicle fractures: completely displaced fractures of the midshaft in healthy, active individuals between 16 and 60 years of age. This comprised 66 of 242 (27%) clavicle fractures in Hill’s study.7
Sling versus Figure of Eight
Grade B evidence (single randomized trial) exists that a sling is as effective as a figure of eight in immobilizing fractures of the clavicle, and it is favored by patients.15
Position of Plate for Open Reduction with Internal Fixation
Grade C evidence (retrospective reviews and nonrandomized comparative study) exists that anterior-inferior plate placement is associated with a lower rate of symptomatic hardware compared with traditional straight plates used superiorly.14,17 However, no comparison with superior precontoured plates has been reported in the literature, and the technique of anteriorinferior plating is one that has a significant learning curve.
Factors Associated with Poor Outcome after Nonoperative Care of Displaced Midshaft Clavicle Fractures
Grade A evidence has been reported from population-based, prospective, observational studies, randomized prospective trials, and retrospective reviews that increasing fracture displacement (especially greater than 2 cm of shortening), comminution/increasing number of fracture fragments, and advancing age are associated with poor outcome (nonunion, symptomatic malunion) after nonoperative care of displaced midshaft fractures of the clavicle.4,7, 9, 10, 14, 16, 24
Plate Fixation versus Intramedullary Nailing
No specific recommendation can be made regarding plate fixation versus intramedullary nailing for displaced midshaft clavicle fractures. Currently, there is no direct comparative study published examining the outcome of plating versus intramedullary nailing of displaced clavicular fractures. However, although two separate randomized trials show clear advantages of open reduction with internal fixation with plating over nonoperative care,16,24 similar studies examining the effect of intramedullary nailing provide contradictory results.20–22 Currently, it is unclear whether the theoretic advantages of intramedullary nailing will outweigh the difficulties in maintaining length and rotation (critical elements of the reduction) of the fracture. One unpublished retrospective review with small numbers (17 patients per group) suggests some superiority of intramedullary pinning over plate fixation or nonoperative care in this setting.20
Plating versus Nonoperative Care of Displaced Midshaft Fractures of the Clavicle
Level B evidence (one published randomized, clinical trial; one presented randomized, clinical trial; one literature meta-analysis) exists that primary plate fixation results in a significant risk reduction for nonunion and symptomatic malunion compared with nonoperative treatment.14,16, 24 Also, as would be expected, patients return to their preoperative level of function more quickly. However, there is a significant reoperation rate, mainly for hardware removal.
SUMMARY
Completely displaced midshaft fractures in healthy, active individuals comprise approximately 25% of all clavicle fractures. A reasonable amount of evidence supports the use of a sling for those patients in whom nonoperative treatment is chosen. Sufficient evidence exists from high-quality prospective studies that certain risk factors (such as displacement or shortening of more than 2 cm or fracture comminution) portend a poor prognosis, and consideration should be given, in the appropriate patient, to operative treatment. Primary plate fixation of displaced clavicle fractures reduces the nonunion and symptomatic malunion rate significantly and results in more rapid return of upper extremity function than nonoperative treatment. Optimal plate position (superior vs. anterior/inferior), or whether intramedullary pinning is as effective as plate fixation, remains unclear. Table 18-1 provides a summary of recommendations for the treatment of displaced midshaft clavicle fractures.
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION | REFERENCES |
|---|---|---|
1 Rowe CR. An atlas of anatomy and treatment of midclavicular fractures. Clin Orthop Relat Res. 1968;58:29-42.
2 Crenshaw AH. Fractures of the shoulder girdle, arm and forearm. Campbell’s Operative Orthopaedics, 8th ed., St. Louis: Mosby-Yearbook; 1992:989-995.
3 Neer C. Nonunion of the clavicle. JAMA. 1960;172:1006-1011.
4 Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following non-operative treatment of a clavicle fracture. J Bone Joint Surg Am. 2004;86:1359-1365.
5 Brinker MR, Edwards TB, O’Connor DP. Letter to the editor. J Bone Joint Surg Am. 2005;87:677-678.
6 Nowak J, Holgersson M, Larsson S. Can we predict long-term sequelae after fractures of the clavicle based on initial findings? A prospective study with nine to ten years follow-up. J Shoulder Elbow Surg. 2004;13:479-486.
7 Hill JM, McGuire MH, Crosby LA. Closed treatment of displaced middle-third fractures of the clavicle gives poor results. J Bone Joint Surg Br. 1997;79:537-541.
8 Nordqvist A, Petersson CJ, Redlund-Johnell I. Mid-clavicle fractures in adults: End result study after conservative treatment. J Orthop Trauma. 1998;12:572-576.
9 McKee MD, Wild LM, Schemitsch EH. Midshaft malunions of the clavicle. J Bone Joint Surg Am. 2003;85:790-797.
10 Basamania CJ: Claviculoplasty. J Shoulder Elbow Surg 8:540, 1999. (Abstracts: Seventh International Conference on Surgery of the Shoulder, 1999.)
11 McKee MD, Stephen DJG, Kreder HJ, et al. Functional outcome following clavicle fractures in polytrauma patients. J Trauma. 2000;47:616.
12 Poigenfurst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: Results of 122 operations. Injury. 1992;23:237-241.
13 McKee MD, Seiler JG, Jupiter JB. The application of the limited contact dynamic compression plate in the upper extremity: An analysis of 114 consecutive cases. Injury. 1995;26:661-666.
14 Zlowodzki M, Zelle BA, Cole PA, et al. Treatment of mid-shaft clavicle fractures: Systemic review of 2144 fractures. J Orthop Trauma. 2005;19:504-508.
15 Andersen K, Jensen PO, Lauritzen J. The treatment of clavicular fractures: Figure of eight bandage versus a simple sling. Acta Orthop Scand. 1987;58:71-74.
16 Smith CA, Rudd J, Crosby LA: Results of operative versus non-operative treatment for 100% displaced mid-shaft clavicle. Proceedings from the 16th Annual Open Meeting of the American Shoulder and Elbow Surgeons, March 18, 2000, p 41.
17 Collinge C, Devinney S, Herscovici D, et al. Anterior-inferior plate fixation of middle-third fractures and nonunions of the clavicle. J Orthop Trauma. 2006;20:680-686.
18 Jubel A, Andermahr J, Schiffer G, et al. Elastic stable intramedullary nailing of mid-clavicular fractures with a titanium nail. Clin Orthop Relat Res. 2003;408:279-285.
19 Boehme D, Curtis RJ, DeHaan JT, et al. Nonunion of fractures of the mid-shaft of the clavicle. Treatment with a modified Haigie intramedullary pin and autogenous bone-grafting. J Bone Joint Surg Am. 1991;73:1219-1226.
20 Sampath DS: Treatment of displaced midclavicle fractures with Rockwood pin: A comparative study. Proceedings of the 2005 AAOS Annual Meeting, p 566.
21 Grassi FA, Tajana MS, D’Angelo F. Management of midclavicular fractures: Comparison between non-operative treatment and open intramedullary fixation in 80 patients. J Trauma. 2001;50:1096-1100.
22 Judd DB, Bottoni CR, Pallis MP, Smith E: Intramedullary fixation versus non-operative treatment for mid-shaft clavicle fractures. Proceedings of the 2005 AAOS Annual Meeting, p 594.
23 Chuang TY, Ho WP, Hsieh PH, et al. Closed reduction and internal fixation for acute midshaft clavicular fractures using cannulated screws. J Trauma. 2006;60:1315-1322.
24 Canadian Orthopaedic Trauma Society. Nonoperative treatment compared with plate fixation of displaced midshaft clavicle fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1-10.