Chapter 16 What Is the Evidence for a Cause-and-Effect Linkage Between Occupational Hand Use and Symptoms of Carpal Tunnel Syndrome?
Because the cause of carpal tunnel syndrome (CTS) is in most cases still unknown, a number of explanatory theories have been proposed, one of which has been occupational hand use. The possible association between occupational hand use and CTS has been mainly based on the common belief that the pathophysiologic mechanism in CTS is increased pressure in the carpal tunnel. It has been suggested that certain hand or wrist activities or postures needed to perform occupational tasks may cause increased carpal tunnel pressure, which may lead to CTS. The hand and wrist activities and postures often linked to CTS have been mainly repetitive movements, force (or combinations of these two factors), and excessive flexion and extension.1 The relationship between CTS and work has been argued for a long time2; an early review concludes that “exposure to physical work load factors, such as repetitive and forceful gripping, was probably a major risk factor for CTS in several types of worker populations.”3 The issue, however, has been debated intensely.4,5
It is helpful to review the reported prevalence and incidence rates of CTS in the general population to interpret the results reported in the literature regarding the relationship between work and CTS. Using diagnostic criteria including nerve conduction measurements, researchers have reported the prevalence rates of CTS among women in general population studies to range from 3% to 6% and among men from 0.6% to 2.1%.6–8 Based on symptoms and nerve conduction measurements, annual incidence rates of up to 0.5% among women and 0.1% among men have been reported.9 If it is assumed that a certain occupation does not increase the risk for CTS, the prevalence of CTS in a random sample of workers from that occupation would likely be lower than that in an age- and sex-matched random general population sample because the latter would include former workers who are sick, disabled, or retired.
STUDY DESIGNS AND BIASES
Randomized Studies
Randomized studies investigating whether occupational hand use is associated with clinical CTS would probably be difficult to perform given the nature of the research question and the large samples needed; to my knowledge, no such studies have been performed.
Confounders
It is well established that a number of factors such as age, sex, and body mass index are related to CTS.6,8, 10, 11 If the exposed workers are older or have a greater proportion of overweight persons than the nonexposed workers, finding a greater prevalence of CTS may be related to these factors rather than to occupation. These factors need to be accounted for when comparing the prevalence of CTS in different occupational groups. Few studies have addressed nonoccupational hand use, but the importance of this factor is uncertain. Other medical conditions, such as inflammatory joint disease and diabetes, may also confound the association between CTS and occupation, but because of the relatively low prevalence of these conditions in occupational groups, their impact may not be large.
LITERATURE REVIEW
The evidence regarding the association between CTS and occupational hand use should be based on appropriate epidemiologic studies in which participants were selected from populations of exposed and nonexposed persons (different occupations or occupational activities), and the presence of CTS determined with reasonable accuracy. A review of the studies generated by the literature search showed several common problems that may affect the conclusions and subsequently the evidence derived from them. Inclusion and exclusion criteria were used to select appropriate studies for evaluation of the evidence.
Carpal Tunnel Syndrome Case Definition
Many studies used self-reported symptoms, physical findings (usually Tinel’s sign and Phalen’s test), or both without nerve conduction measurement. Symptoms were usually self-reported either through questionnaire or interview often done by research assistants rather than by physicians experienced in the diagnosis of CTS. In addition, studies differed in their definition of symptoms required for the diagnosis with regard to location, severity, and frequency. The issue of CTS case definition was considered to be essential for the purpose of this report. A case definition based entirely on symptoms would probably lead to substantial misclassification. The prevalence of symptoms (numbness or tingling) in the hands is relatively high, and only a proportion of these symptomatic persons actually have CTS.8,12 Although there may be some evidence supporting the common clinical practice that patients judged by the treating physician to have characteristic CTS symptoms may not need electrophysiologic confirmation, nerve conduction tests will increase the probability of a correct diagnosis in all types of settings. The severity of CTS in epidemiologic studies is expected to be lower than that in clinical settings, and because nerve conduction measurement results are more likely to be normal in mild than in severe CTS, this makes the diagnostic procedure in epidemiologic studies more difficult. Questionnaires inquiring about symptoms would have low specificity, and although interviews can confirm the presence and location of the reported symptoms, an interview performed for the purpose of establishing a CTS diagnosis based on symptoms alone may need to be conducted by an examiner who can judge whether the symptoms are related to CTS or other disorder, or are nonspecific. Results based on reported symptoms alone are thus not appropriate as evidence of the association between work and CTS. However, the combination of symptoms and abnormal nerve conduction will substantially improve the specificity and would be reasonably reliable as a diagnostic procedure. In a general population study, the prevalence of symptoms was 14%, whereas with symptoms and abnormal nerve conduction, the prevalence rate was down to 5%.8 A similar pattern has been reported in occupational populations.13 This suggests that the degree of misclassification is substantially lower if a combination of symptoms and nerve conduction measurement is used in case definition for occupational studies than symptoms alone. The use of this case definition may still imply two problematic situations. First, a proportion of CTS cases with normal (i.e., false-negative) nerve conduction testing results would be excluded; this situation, which may occur in up to 20% of subjects,8,14 is expected to affect both the exposed and nonexposed groups equally and, therefore, may affect the precision but not the size of the estimated association. Second, a proportion of persons with nonspecific numbness/tingling but with false-positive nerve conduction testing results would be included as CTS cases. In the presence of reporting bias (symptomatic persons reporting higher exposure), this situation may overestimate the association, but probably to a small degree. Although relatively high rates of abnormal nerve conduction testing results (15–20%) have been reported in general population samples7,8 and among asymptomatic workers,13,15 the combination of symptoms and nerve conduction measurements still constitutes the most accurate diagnostic method available in CTS. Any case definition will lead to misclassification of a proportion of cases, but in epidemiologic studies, the use of nerve conduction measurements combined with self-reported symptoms substantially reduces the degree of misclassification.16 Similarly, studies that used a case definition based only on positive Tinel’s sign and Phalen’s test cannot be considered to provide adequate evidence because of the limitations of these tests in the diagnosis.17
Exclusion Criteria
RESULTS
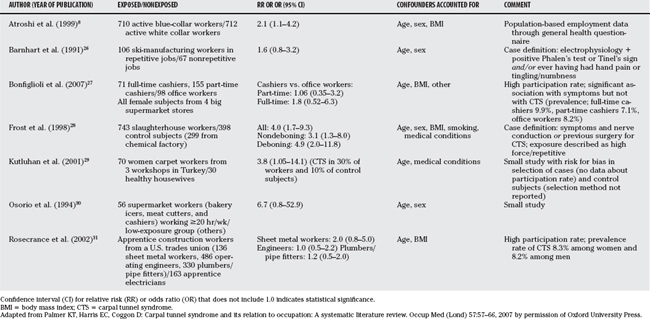
The review showed that most of the relevant studies had been included in two previous reviews, the most recent of which examined the literature published through 2004.18,19 Several of the studies that have assessed the relationship between CTS and occupational activities (Table 16-1) or occupational title (Table 16-2), using an adequate case definition (symptoms and nerve conduction measurement),8,20–31 have shown an association between CTS and either certain occupational activities (hand force, excessive wrist flexion/extension, or repetitive wrist motion) or certain occupations, with relative risks or odds ratios of up to 9.0 shown. However, some associations were inconsistent. In a number of “negative” studies that failed to show a statistically significant association, the lower limit of the 95% confidence interval for the odds ratio was just less than 1.0, suggesting a small sample size.
TABLE 16-1 Studies of Carpal Tunnel Syndrome and Occupational Activities Using a Carpal Tunnel Syndrome Case Definition of Symptoms and Abnormal Nerve Conduction Measurement Results (Unless Specified)
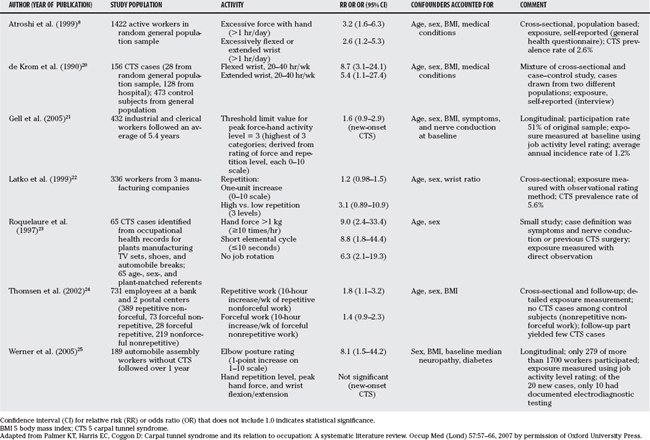
TABLE 16-2 Studies of Carpal Tunnel Syndrome and Job Title Using a Carpal Tunnel Syndrome Case Definition of Symptoms and Abnormal Nerve Conduction Measurement Results (Unless Specified)
Studies with Less Specific Case Definitions
In a longitudinal cohort study from Denmark, Andersen and coworkers32 investigated the relationship between computer work and CTS in a sample of 9480 technical assistants and machine technicians with a 1-year follow-up period; response rate was 73% at baseline and 82% at follow-up. Symptoms and exposure (mouse and keyboard use) were self-reported using a questionnaire and interview, but the case definition was based on symptoms only. The authors report an association between mouse use for more than 20 hours/week and risk for symptoms, but no statistically significant association with keyboard use, and conclude that “computer use does not pose a severe occupational hazard for developing symptoms of CTS.”32 The association between computer work and CTS has also been investigated in studies with adequate case definition. Gerr and colleagues33 followed 582 persons newly hired into jobs requiring at least 15 hours per week of computer use for up to 3 years, finding a low incidence of electrophysiologically confirmed CTS (3 cases). Stevens and researchers34 examined 256 employees described as frequent computer users at a medical facility, finding only 9 persons with electrophysiologically confirmed CTS and concluding that the prevalence was similar to that reported in general population studies. The overall evidence from a number of studies suggests that computer work is not associated with greater risk for CTS.
In a relatively large case–control study from France, Leclerc and coworkers35 compared 1210 workers in repetitive work (assembly line, clothing and shoe industry, and food industry) from 53 different companies with a control group of 337 workers. Exposure was measured partly by self-report and partly assessed by occupational physicians, but the case definition demanded only positive Tinel’s sign or Phalen’s test (symptoms were not part of the criteria). The authors conclude that “CTS was associated with several factors including repetitive work, especially packaging.”35 Using the same case definition, the authors performed a longitudinal study of 598 workers (assembly, clothing, food, packaging, cashiers) who were re-examined after 3 years, and reported an association between CTS and forceful movements.36 In a large cross-sectional study from France, Melchior and colleagues37 examined a random sample of 2656 workers for a variety of upper limb musculoskeletal disorders including CTS, which was diagnosed based on symptoms and signs only. The authors report a greater risk for “CTS” in manual compared with nonmanual workers, which after adjusting for age, obesity, and medical conditions was statistically significant among women (prevalence ratio, 2.1; 95% confidence interval, 1.2–3.7) but not among men (prevalence ratio, 1.4; 95% confidence interval, 0.7–2.8).
In a longitudinal study, Nathan and investigators38 examined a cohort of 471 workers from 4 industries in Oregon, at baseline and after 11 and 17 years; the case definition changed from only abnormal nerve conduction at baseline to what was described as “research-defined CTS” requiring symptoms (at least twice per month) and abnormal nerve conduction or previous CTS surgery at the final follow-up.38–40 The baseline work exposure was used despite possible work change over time, and large attrition of the sample occurred with 54% and 35% participation rates at the two follow-up examinations, respectively. The authors consistently report no association between CTS and occupational repetition or force. The significant risk for bias limits the contribution of these studies to the overall evidence. In a case–control study Nordstrom and coauthors41 identify 206 “newly diagnosed” CTS cases from clinic database in the Marshfield area in Wisconsin (physician-made diagnosis not requiring nerve conduction testing) and compare them with 211 randomly sampled residents with no CTS diagnosis; information on risk factors was obtained through telephone interviews and from medical records.41 After adjustment for age, sex, body mass index, and other medical conditions, the occupational risk factors that showed statistically significant associations with “CTS” were frequent (.6 vs. 0 hours) use of power tools/machinery and bending/twisting of hands/wrists, with odds ratios (95% confidence interval) of 3.3 (1.1–9.8) and 2.1 (1.0–4.5), respectively.
In a case–control study from Canada, Rossignol and colleagues42 used Montreal’s surgery database of 1 year to identify 969 first-surgery CTS cases and conducted telephone interviews of a sample of 238 cases to obtain occupational history (94% reported having electrodiagnostic tests but no data on results). The authors conclude that among manual workers, “55% of surgical CTS in women and 76% in men was attributable to work,” and that increased risk for surgical CTS was found in seven occupational groups. The study adjusted for age and sex but not for other confounders, and the use of surgery database and telephone interview of a sample to obtain occupational history may have introduced selection and reporting bias. In a frequently cited cross-sectional study, Silverstein and investigators43 examined 652 workers in 39 jobs from 7 industries in the United States, using good exposure measurement (including observation and video analysis) to classify jobs into 4 groups (high/low force/repetition), but the case definition was based only on symptoms and physical signs. After adjustment for several potential confounders, the odds ratio of “CTS” in the high-force, high-repetition group compared with the low-force, low-repetition group was 15.5 (95% confidence interval, 1.7–142).
Experimental Studies
Several experimental studies have explored the hypothesis that working with certain wrist positions or force exertion may have potentially harmful effects on the median nerve in the carpal tunnel. A number of studies have measured carpal tunnel pressures in different wrist or hand positions or activities.44–47 However, findings that wrist flexion and extension or certain finger positions or force levels lead to increased carpal canal pressure cannot be regarded as direct evidence that work with such positions will cause CTS. Similarly, studies have examined median nerve conduction or morphology in the carpal tunnel in certain occupational groups. The results of such experimental studies provide plausibility to the hypothesis, but not evidence, that specific work activities may lead to CTS.
CONCLUSIONS
To prove a causal relationship between occupational hand use and CTS, study investigators ideally would include an adequately large number of persons who have no symptoms of CTS at baseline, examine them clinically and neurophysiologically and follow them for an appropriate period, define and measure exposure with a reliable and valid method, and re-examine the persons at follow-up clinically and neurophysiologically to determine the incidence of CTS in the exposed and nonexposed groups. Most studies in the review were case–control or cross-sectional and had various limitations that affected the strength of the conclusions derived from them regarding the association between occupational hand use and CTS. The few longitudinal studies found typically were too small to yield adequate number of cases for strong conclusions regarding cause-and-effect relation. Dose–response associations have not been adequately demons-trated. Despite the limitations in the current literature, fairly consistent epidemiologic evidence has been reported of an association between certain work activities or certain occupations and CTS. However, the evidence does not permit firm conclusions about the exact nature of the cause, whether it is force, posture, repetitiveness, or a combination of these factors. A fair amount of evidence exists to support that occupations in which some or all of these factors are predominant (compared with other types of occupations) seem to be associated with a greater risk for CTS. Table 16-3 provides a summary of recommendations.
| ASSOCIATION BETWEEN OCCUPATIONAL ACTIVITY AND SYMPTOMS OF CARPAL TUNNEL SYNDROME | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
| Force (exertion of high force with the hand) | B |
| Repetitiveness (highly repetitive wrist motion) | B |
| Posture (prolonged extreme wrist flexion or extension) | B |
Based on evidence from studies that involve one or more of these occupational activities, as well as studies that involve specific occupations in which one of these activities would be dominant.
1 Keyserling WM, Stetson DS, Silverstein BA, et al. A checklist for evaluating ergonomic risk factors associated with upper extremity cumulative trauma disorders. Ergonomics. 1993;36:807-831.
2 Armstrong TJ, Chaffin DB. Carpal tunnel syndrome and selected personal attributes. J Occup Med. 1979;21:481-486.
3 Hagberg M, Morgenstern H, Kelsh M. Impact of occupations and job tasks on the prevalence of carpal tunnel syndrome. Scand J Work Environ Health. 1992;18:337-345.
4 Szabo RM, King KJ. Repetitive stress injury: Diagnosis or self-fulfilling prophecy? J Bone Joint Surg Am. 2000;82:1314-1322.
5 Amadio PC. Repetitive stress injury. J Bone Joint Surg Am. 2001;83:136-137.
6 de Krom MC, Knipschild PG, Kester AD, et al. Carpal tunnel syndrome: Prevalence in the general population. J Clin Epidemiol. 1992;45:373-376.
7 Ferry S, Pritchard T, Keenan J, et al. Estimating the prevalence of delayed median nerve conduction in the general population. Br J Rheumatol. 1998;37:630-635.
8 Atroshi I, Gummesson C, Johnsson R, et al. Prevalence of carpal tunnel syndrome in a general population. JAMA. 1999;282:153-158.
9 Mondelli M, Giannini F, Giacchi M. Carpal tunnel syndrome incidence in a general population. Neurology. 2002;58:289-294.
10 Werner RA, Albers JW, Franzblau A, et al. The relationship between body mass index and the diagnosis of carpal tunnel syndrome. Muscle Nerve. 1994;17:632-636.
11 Werner RA, Franzblau A, Albers JW, et al. Influence of body mass index and work activity on the prevalence of median mononeuropathy at the wrist. Occup Environ Med. 1997;54:268-271.
12 Anton D, Rosecrance J, Merlino L, et al. Prevalence of musculoskeletal symptoms and carpal tunnel syndrome among dental hygienists. Am J Ind Med. 2002;42:248-257.
13 Isolani L, Bonfiglioli R, Raffi GB, et al. Different case definitions to describe the prevalence of occupational carpal tunnel syndrome in meat industry workers. Int Arch Occup Environ Health. 2002;75:229-234.
14 Finsen V, Russwurm H. Neurophysiology not required before surgery for typical carpal tunnel syndrome. J Hand Surg [Br]. 2001;26:61-64.
15 Homan MM, Franzblau A, Werner RA, et al. Agreement between symptom surveys, physical examination procedures and electrodiagnostic findings for the carpal tunnel syndrome. Scand J Work Environ Health. 1999;25:115-124.
16 Rempel D, Evanoff B, Amadio PC, et al. Consensus criteria for the classification of carpal tunnel syndrome in epidemiologic studies. Am J Public Health. 1998;88:1447-1451.
17 Gerr F, Letz R. The sensitivity and specificity of tests for carpal tunnel syndrome vary with the comparison subjects. J Hand Surg [Br]. 1998;23:151-155.
18 National Institute for Occupational Health Safety. Musculoskeletal disorders and workplace factors: A critical review of epidemiologic evidence for work-related musculoskeletal disorders of the neck, upper extremity and low back. Cincinnati, OH: US Department of Health and Human Sciences/NIOSH, 1997.
19 Palmer KT, Harris EC, Coggon D. Carpal tunnel syndrome and its relation to occupation: A systematic literature review. Occup Med (Lond). 2007;57:57-66.
20 de Krom MC, Kester AD, Knipschild PG, et al. Risk factors for carpal tunnel syndrome. Am J Epidemiol. 1990;132:1102-1110.
21 Gell N, Werner RA, Franzblau A, et al. A longitudinal study of industrial and clerical workers: Incidence of carpal tunnel syndrome and assessment of risk factors. J Occup Rehabil. 2005;15:47-55.
22 Latko WA, Armstrong TJ, Franzblau A, et al. Cross-sectional study of the relationship between repetitive work and the prevalence of upper limb musculoskeletal disorders. Am J Ind Med. 1999;36:248-259.
23 Roquelaure Y, Mechali S, Dano C, et al. Occupational and personal risk factors for carpal tunnel syndrome in industrial workers. Scand J Work Environ Health. 1997;23:364-369.
24 Thomsen JF, Hansson GA, Mikkelsen S, et al. Carpal tunnel syndrome in repetitive work: A follow-up study. Am J Ind Med. 2002;42:344-353.
25 Werner RA, Franzblau A, Gell N, et al. Incidence of carpal tunnel syndrome among automobile assembly workers and assessment of risk factors. J Occup Environ Med. 2005;47:1044-1050.
26 Barnhart S, Demers PA, Miller M, et al. Carpal tunnel syndrome among ski manufacturing workers. Scand J Work Environ Health. 1991;17:46-52.
27 Bonfiglioli R, Mattioli S, Fiorentini C, et al. Relationship between repetitive work and the prevalence of carpal tunnel syndrome in part-time and full-time female supermarket cashiers: A quasi-experimental study. Int Arch Occup Environ Health. 2007;80:248-253.
28 Frost P, Andersen JH, Nielsen VK. Occurrence of carpal tunnel syndrome among slaughterhouse workers. Scand J Work Environ Health. 1998;24:285-292.
29 Kutluhan S, Akhan G, Demirci S, et al. Carpal tunnel syndrome in carpet workers. Int Arch Occup Environ Health. 2001;74:454-457.
30 Osorio AM, Ames RG, Jones J, et al. Carpal tunnel syndrome among grocery store workers. Am J Ind Med. 1994;25:229-245.
31 Rosecrance JC, Cook TM, Anton DC, et al. Carpal tunnel syndrome among apprentice construction workers. Am J Ind Med. 2002;42:107-116.
32 Andersen JH, Thomsen JF, Overgaard E, et al. Computer use and carpal tunnel syndrome: A 1-year follow-up study. JAMA. 2003;289:2963-2969.
33 Gerr F, Marcus M, Ensor C, et al. A prospective study of computer users: I. Study design and incidence of musculoskeletal symptoms and disorders. Am J Ind Med. 2002;41:221-235.
34 Stevens JC, Witt JC, Smith BE, et al. The frequency of carpal tunnel syndrome in computer users at a medical facility. Neurology. 2001;56:1568-1570.
35 Leclerc A, Franchi P, Cristofari MF, et al. Carpal tunnel syndrome and work organisation in repetitive work: A cross sectional study in France. Study Group on Repetitive Work. Occup Environ Med. 1998;55:180-187.
36 Leclerc A, Landre MF, Chastang JF, et al. Upper-limb disorders in repetitive work. Scand J Work Environ Health. 2001;27:268-278.
37 Melchior M, Roquelaure Y, Evanoff B, et al. Why are manual workers at high risk of upper limb disorders? The role of physical work factors in a random sample of workers in France (the Pays de la Loire study). Occup Environ Med. 2006;63:754-761.
38 Nathan PA, Meadows KD, Doyle LS. Occupation as a risk factor for impaired sensory conduction of the median nerve at the carpal tunnel. J Hand Surg [Br]. 1988;13:167-170.
39 Nathan PA, Meadows KD, Istvan JA. Predictors of carpal tunnel syndrome: An 11-year study of industrial workers. J Hand Surg [Am]. 2002;27:644-651.
40 Nathan PA, Istvan JA, Meadows KD. A longitudinal study of predictors of research-defined carpal tunnel syndrome in industrial workers: Findings at 17 years. J Hand Surg [Br]. 2005;30:593-598.
41 Nordstrom DL, Vierkant RA, DeStefano F, et al. Risk factors for carpal tunnel syndrome in a general population. Occup Environ Med. 1997;54:734-740.
42 Rossignol M, Stock S, Patry L, et al. Carpal tunnel syndrome: What is attributable to work? The Montreal Study. Occup Environ Med. 1997;54:519-523.
43 Silverstein BA, Fine LJ, Armstrong TJ. Occupational factors and carpal tunnel syndrome. Am J Ind Med. 1987;11:343-358.
44 Szabo RM, Chidgey LK. Stress carpal tunnel pressures in patients with carpal tunnel syndrome and normal patients. J Hand Surg [Am]. 1989;14:624-627.
45 Werner R, Armstrong TJ, Bir C, et al. Intracarpal canal pressures: The role of finger, hand, wrist and forearm position. Clin Biomech (Bristol, Avon). 1997;12:44-51.
46 Keir PJ, Bach JM, Rempel DM. Effects of finger posture on carpal tunnel pressure during wrist motion. J Hand Surg [Am]. 1998;23:1004-1009.
47 Keir PJ, Bach JM, Rempel DM. Fingertip loading and carpal tunnel pressure: Differences between a pinching and a pressing task. J Orthop Res. 1998;16:112-115.







