Chapter 67 What Is the Best Treatment for Plantar Fasciitis?
Plantar fasciitis is a painful heel syndrome of unclear cause. Chronic or acute injury to the origin of the plantar fascia at the medial tubercle of the calcaneus is thought to produce a cycle of microtrauma and degenerative changes. Plantar fasciitis affects both active and sedentary adults with studies reporting that up to 10% of runners and a similar proportion of the general population are affected.1–4 A significant occurrence also is reported in military personnel and professional athletes.5,6 Increased body mass index, extended time standing, and limited ankle dorsiflexion are risk factors predisposing to plantar fasciitis.7 The high prevalence, substantial pain, and decreased tolerance for activity result in large numbers of patients seeking treatment. The cumulative number of office visits in the United States is estimated to be nearly 1 million visits each year.1
TREATMENT
Plantar fasciitis tends to improve in most cases regardless of the treatment selected.8–11 As a result, conservative management is effective for nearly 90% of patients.12,13 The conservative treatments used in management of plantar fasciitis vary widely and are dependent on physician specialty.1 Common treatments include nonsteroidal anti-inflammatory drugs (NSAIDs), stretching, insoles, taping, physical therapy, and night splints. If these simple and noninvasive modalities prove ineffective, additional treatment options include iontophoresis, injections, extracorporeal shock wave therapy (ESWT), and surgical treatment. This chapter reviews the various treatment methods for plantar fasciitis, and the effectiveness and safety of these treatments as supported by the best available evidence.
Stretching
Stretching protocols for the treatment of plantar fasciitis include stretching the Achilles tendon with or without stretching of the plantar fascia. Limited evidence is available from controlled trials to establish the effectiveness of stretching.14 Prospective studies comparing a plantar fascia–specific stretching protocol before the first morning steps and Achilles tendon stretching for treating chronic plantar fasciitis found a greater improvement in pain symptoms with the plantar fascia–specific stretching after 8 weeks (Level of Evidence II).15 Long-term follow-up at 2 years was incomplete but suggested no difference between Achilles tendon stretching and the plantar fascia–specific groups, although both groups showed improvement (Level of Evidence III).16
Taping
Taping techniques are intended to alter the position and alignment of the calcaneus, and to support the longitudinal arch. The effectiveness of calcaneal taping was compared with stretching, no treatment, and sham taping in one small study. Taping produced greater improvement in reported pain on a visual analog scale (VAS) than sham taping, controls with no treatment, or stretching (Level II).14 A larger study with 92 participants that examined taping with ultrasound compared with sham ultrasound reported a small improvement with taping in first step pain, one of four measured parameters (Level I).17 Sensitivity or allergy to tape may cause skin irritation.18
Nonsteroidal Anti-inflammatory Drugs
NSAIDs are used extensively in the management of acute and chronic musculoskeletal pain. The mechanisms for the anti-inflammatory and analgesic effects of these drugs are well documented in an extensive body of basic science and clinical research. Despite this, limited evidence exists to support the efficacy of NSAIDs in shortening the course or decreasing the symptoms of plantar fasciitis. One small trial found a nonstatistically significant decrease in pain and disability with NSAID treatment of plantar fasciitis (Level II).19 Other studies have quantified NSAID use as a measure of improvement with other therapies.20 The use of NSAIDs is associated with known adverse effects, which have been reported extensively in the medical literature.
Orthoses
The use of orthoses is intended to change loading characteristics of the plantar aponeurosis. Studies using cadaveric limbs suggest that support of the medial longitudinal arch can decrease strain of the plantar aponeurosis.21 Several randomized, controlled trials have examined the use of insoles in management of plantar fasciitis. A recent study comparing custom insoles, sham insoles, and prefabricated insoles found minor improvement in symptoms 3 months after treatment with prefabricated or custom insoles compared with sham (Level I).22 Prefabricated insoles have been found to be as effective as custom insoles at a reduced total cost.22–24 Insoles may be equally effective and offer improved patient compliance compared with night splints.24,25 A randomized, placebo-controlled, double-blind study conducted with 101 patients compared magnetic insoles with sham magnetic insoles and found no statistically significant improvement in pain symptoms after 8 weeks of treatment (Level II).26
Night Splints
Tension night splints stretch the plantar fascia over several hours while the patient sleeps by maintaining a constant ankle dorsiflexion. A trial comparing night splints with conservative treatment with conservative treatment alone found no significant difference in symptoms (Level I).27 Roos and coworkers28 compared insoles with night splints and found no significant difference in pain reduction and improved compliance with insoles (Level II). 28 Three studies reported that patients find night splint treatment uncomfortable and difficult to maintain, resulting in decreased compliance.24,28, 29 A systematic review found that the evidence for the effectiveness of night splints is inconclusive (Level II).3
Casting
Limited evidence has been reported for the effectiveness of casting in treatment of plantar fasciitis. One case series of 32 patients reported improvement in pain symptoms after 6 months after treatment with casting (Level IV).30 A fiberglass walking cast was used in the study.
Iontophoresis
Iontophoresis uses an electrical potential generated by bipolar electrodes to transfer charged ions and ionizable materials including some medications through the skin to provide anti-inflammatory or analgesic treatment.31 Conflicting results have been published for the effectiveness of dexamethasone iontophoresis. In a double-blind study with 39 subjects comparing iontophoresis using dexamethasone with a placebo, significant improvement on the Maryland foot score was reported at the end of the 2-week treatment period (3.80; 95% confidence interval [CI], 0.76–6.84) but not after 1 month (0.30; 95% CI, −2.16 to 6.76) (Level I).31 A second randomized, controlled trial with 31 subjects compared iontophoresis with taping and 0.4% dexamethasone, 5% acetic acid, or 0.9% NaCl placebo. The graphical data presented in the study indicate no statistically significant improvement with dexamethasone treatment in six measured outcomes at 4 weeks and less relief of pain symptoms compared with the control group at 2 weeks of treatment. In the group treated with acetic acid, there was a significant improvement in morning stiffness at 4 weeks with no reported statistically significant difference in three measures of pain at 4 weeks and no significant improvement compared with placebo in all six parameters at 2 weeks (Level I).18
Steroid Injection
Previously published reviews have found limited evidence to support the use of steroid injections in the treatment of plantar fasciitis.3,8 Steroid injection with and without nerve block was compared with placebo in a double-blind, randomized, control trial with 91 participants (Level I).32 The study found a statistically significant benefit at 1 month with steroid injection but not at 3 and 6 months. In addition, it was reported that tibial nerve block was not effective at relieving pain associated with steroid injection. A prospective study with 132 patients comparing steroid injection with ESWT or placebo found a statistically significant improvement in pain symptoms for the group receiving steroid injection over ESWT or placebo (Level II).33 The participants in this study reported VAS pain scores that were significantly lower than for the control and ESWT groups at 3 and 12 months. Potential adverse side effects of steroid injection include fat pad atrophy and plantar fascia rupture.
Botulinum Toxin Type A Injection
Botulinum toxin is used in the treatment of a variety of pain syndromes, and its use in treatment of plantar fasciitis has been reported. A single randomized, placebo-controlled, double-blind study conducted with 27 patients and 43 treated feet found statistically significant improvement in pain symptoms 3 and 8 weeks after treatment (Level I).34 Additional studies of the use of botulinum toxin in the treatment of plantar fasciitis are necessary to further define safety and efficacy.
Extracorporeal Shock Wave Therapy
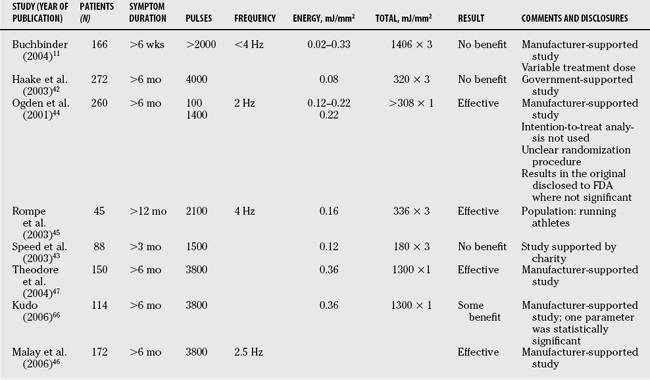
ESWT utilizes application of mechanical waves similar to those used in lithotripsy but of lower energy density, usually less then 0.36 mJ/mm2 per pulse. Therapy consists of 500 to 6000 pulses delivered at 2 to 4 Hz to treat plantar foot pain. The mechanism by which ESWT provides benefit is investigational. Current theories include stimulation of healing after increased release of growth factors and neovascularization in the environment of local tissue injury35,36 or alteration in the chemical function of small axons producing analgesic effects.37,38 The possibility of a noninvasive treatment for chronic plantar fasciitis has generated significant interest, and several studies investigating the effectiveness of this technique have been published. Many of these trials are not of sufficient quality to provide a reliable assessment of the effectiveness of ESWT.3,8, 39, 40 The studies investigating ESWT have been in many cases sponsored by the equipment manufacturers, and the randomized control trials have produced conflicting results. Good quality, randomized, placebo-controlled, double-blind clinical trials have found no significant benefit to ESWT,41–43 whereas other randomized, controlled trials44–47 have found ESWT to be beneficial. The reasons for the discrepancy in reported results are unclear. A lack of uniformity of therapy exists from study to study, with differing methods for assessment of therapy, and in some studies, significant problems with study design have been reported.3,40 Differences also exist in the definition of the terms high energy and low energy, as well as in the amount of energy used in various studies. No controlled trials adequately define and identify indications for high- or low-energy protocols for ESWT. In addition, differences in criteria for patient inclusion in the studies make it difficult to compare the trials directly. Table 67-1 summarizes double-blind, randomized studies comparing ESWT with placebo. The reported adverse reactions, including skin redness, bruising, pain, numbness, tingling, and local swelling,42,44, 46 likely do not pose serious health risks. However, clear evidence supporting the use of ESWT treatment in the treatment of plantar fasciitis has not been reported.
Surgery
No randomized, controlled trials compare patients undergoing surgical treatments with a control population. Surgical treatment is considered for the approximately 10% of patients who do not respond to conservative treatment. Surgical treatment options include percutaneous plantar fasciotomy, endoscopic plantar fasciotomy, or open fasciotomy.48,49 Cryosurgery is another proposed treatment that was reported in one case series to result in improvement of symptoms.50 Complications of surgical treatments include forefoot stress fracture, calcaneal fracture, medial or lateral column pain, nerve injury, infection, and instability.51,52 For surgical treatments, published case series report that between 75% and 95% of patients responded with improvement in measured symptoms after surgical treatment, with up to 27% having residual pain symptoms and 20% reporting activity restriction.8,49,53–56 Increasing body mass index is a risk factor for poorer response to surgical treatment.57 A study comparing plantar fascia release of 25%, 50%, or 66% of the insertion by open or endoscopic procedures reports that increasing lateral column pain symptoms occurred with increased percentage of plantar fascia release.51 Limited evidence is available to suggest when surgical treatment should be recommended or to guide the choice of surgical treatment.
Open Fasciotomy.
Medial fasciotomy can be performed with local or general anesthesia. The plantar fascia is approached through an incision beginning medially and extending to the plantar aspect of the foot to allow exposure and release of the deep and superficial fascia of the abductor hallucis brevis muscle. Further dissection is used to identify and transect the medial aspect of the central plantar fascial band.58 For patients with neurologic symptoms resulting from suspected compression of the first branch of the lateral plantar nerve, which innervates the abductor digiti quinti (Baxter’s nerve), fasciotomy is accompanied by decompression of the nerve through release of the deep fascia of the abductor hallucis.59 Other authors advocate proximal release of the tarsal tunnel when neurologic symptoms suggest that refractory heel pain is associated with both plantar fasciitis and tarsal tunnel syndrome.60 No controlled trials adequately compare isolated plantar fasciotomy with techniques that incorporate release of Baxter’s nerve or the tarsal tunnel. The open technique also allows for the removal of a prominent plantar heel spur when present. No controlled trials have determined whether removal of a spur improves outcomes when compared with soft-tissue release only.
Endoscopic Fasciotomy.
Endoscopic fasciotomy may be conducted with regional nerve blocks for anesthesia. One or two ports have been used with ideal port placement being 1 to 2 mm distal to the medial calcaneal tubercle at the level of the inferior aspect of the plantar fascia. After careful cannula placement, the plantar fascia is identified and the medial third is released with a hook knife. Patients can be fully weight bearing after the procedure with moderate activity. Prospective studies of endoscopic release of the plantar fascia have reported relief of symptoms in up to 97% of treated patients (Level II).61 Other studies have reported shortened recovery time compared with open procedures (Level IV).62 No large-scale trials have directly compared outcomes in patients undergoing open as opposed to endoscopic treatment for plantar fasciitis.
Other Treatments
The application of topical wheat-grass cream has been proposed in treatment of plantar fasciitis. A randomized, placebo-controlled double-blind study conducted with 80 patients found no statistically significant improvement resulting from treatment at 6 and 12 weeks. Primary outcome measures were a VAS for first-step pain in the morning and the Foot Health Status Questionnaire.63 No further studies on this treatment have been reported.
Irradiation of skin or soft tissue with low-power lasers has been proposed as an agent for pain management in plantar fasciitis.64 A single randomized, placebo-controlled, double-blind study conducted with 32 patients found no statistically significant improvement in 6 measured parameters during a series of treatments or 1 month after therapy. Adverse reactions were minimal (Level I).65
Limited evidence supports the recommendation of any one therapy in the treatment of plantar fasciitis.40 As a result, the use of less costly and less invasive treatment modalities such as stretching, taping, NSAIDs, orthoses, and night splints remain first-line therapies for plantar fasciitis. The failure of these conservative modalities may lead to the need for more costly or invasive treatments including casting, iontophoresis, injection, ESWT, or open or endoscopic plantar fasciotomy.
Studies for several of these treatments have produced conflicting results. Recommendations with grade of evidence for specific treatments and references are summarized in Table 67-2. Problems with study design have been recognized for several published trials and include description of randomization procedures, concealment of allocation, use of intention-to-treat analysis, absent or ineffective blinding, and duplicate publication of previously published results.2,3
| RECOMMENDATIONS | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION | REFERENCES |
|---|---|---|
Plantar fasciitis tends to improve spontaneously, and in most of the comparative studies of treatment for plantar fasciitis, it was found that both the treatment groups and the control groups improved with time.3,8, 11 Conservative treatment is effective for nearly 90% of patients.12,13 No evidence supports the use of rest and ice, and limited evidence supports NSAID use in the treatment of plantar fasciitis. These treatments are effective general measures used in conservative management of many musculoskeletal complaints and may be considered for adjunctive therapy for treatment of plantar fasciitis in absence of contraindications. Prefabricated insoles, plantar fascia–specific stretching, and taping techniques should be considered as part of conservative treatment for short-term improvement in symptoms, but evidence for their efficacy is also limited.
The optimal period of conservative treatment before considering more invasive treatments has not been determined. Most studies examined the effectiveness of conservative treatments at 3 months, 6 months, or 1 year. When symptoms persist despite conservative treatment, steroid injections may be considered for short-term relief of symptoms but are associated with plantar fascia rupture and fat pad atrophy. Botulinum toxin injection and acetic acid iontophoresis may be considered, but the effectiveness of each is supported by only a single, small randomized trial. Casting and cryosurgery are additional proposed therapies, but evidence is lacking to establish effectiveness of these treatments. Available evidence does not provide convincing support for the effectiveness of night splints, steroid iontophoresis, ESWT, magnetic insoles, laser therapy, or topical application of wheat grass. Patient who do not respond to nonoperative management may consider surgical treatment with endoscopic or open release of 50% or less of the plantar fascia. Reported complications of surgery include persistent pain, fracture, nerve injury, infection, and instability. No randomized controlled trials compare surgical treatment with a control population, but there have been several reports of series of patients achieving satisfactory results with either open or endoscopic plantar fasciotomy.
1 Riddle DL, Schappert SM. Volume of ambulatory care visits and patterns of care for patients diagnosed with plantar fasciitis: A national study of medical doctors. Foot Ankle Int. 2004;25:303-310.
2 Atkins D, Crawford F, Edwards J, et al. A systematic review of treatments for the painful heel. Rheumatology. 1999;38:968-973.
3 Crawford F, Atkins D, Edward J. Interventions for treating plantar heel pain (Cochrane Review). In: Cochrane Library, Issue 3. Oxford: Update Software; 2000.
4 DeMaio M, Paine R, Mangine RE, et al. Plantar fasciitis. Orthopedics. 1993;16:1153-1163.
5 Moseley JBJr, Chimenti BT. Foot and ankle injuries in the professional athlete. The Foot and Ankle in Sport. St. Louis: Mosby, 1995;321-328.
6 Sadat-Ali M. Plantar fasciitis/calcaneal spur among security forces personnel. Mil Med. 1998;163:56-57.
7 Riddle DL, Pulisic M, Pidcoe P, et al. Risk factors for plantar fasciitis: A matched case control study. J Bone Joint Surg Am. 2003;85-A:872-887.
8 Cole C, Seto C, Gazewood J. Plantar fasciitis: Evidence-based review of diagnosis and therapy. Am Fam Physician. 2005;72:2237-2242.
9 Berkowitz JF, Kier R, Rudicel S. Plantar fasciitis: MR imaging. Radiology. 1991;179:665-667.
10 Kane D, Greaney T, Shanahan M, et al. The role of ultrasonography in the diagnosis and management of idiopathic plantar fasciitis. Rheumatology (Oxford). 2001;40:1002-1008.
11 Buchbinder R. Clinical practice. Plantar fasciitis. N Engl J Med. 2004;350:2159-2166.
12 Gill L, Kiebzak G. Outcome of non-surgical treatment for plantar fasciitis. Foot Ankle. 1997;18:821-822.
13 Wolgin M, Cook C, Graham C, Mauldin D. Conservative treatment of plantar heel pain: Long term follow-up. Foot Ankle Int. 1994;15:97-102.
14 Hyland MR, Webber-Gaffney A, Cohen L, et al. Randomized controlled trial of calcaneal taping, sham taping, and plantar fascia stretching for the short-term management of plantar heel pain. J Orthop Sports Phys Ther. 2006;36:364-371.
15 DiGiovanni BF, Nawoczenski DA, Lintal ME, et al. Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:1270-1277.
16 Digiovanni BF, Nawoczenski DA, Malay DP, et al. Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis. A prospective clinical trial with two-year follow-up. J Bone Joint Surg Am. 2006;88:1775-1781.
17 Radford JA, Landorf KB, Buchbinder R, et al. Effectiveness of low-Dye taping for the short-term treatment of plantar heel pain: A randomised trial. BMC Musculoskelet Disord. 2006;7:64.
18 Osborne HR, Allison GT. Treatment of plantar fasciitis by LowDye taping and iontophoresis: Short term results of a double blinded, randomised, placebo controlled clinical trial of dexamethasone and acetic acid. Br J Sports Med. 2006;40:545-549.
19 Donley BG, Moore T, Sferra J, et al. The efficacy of oral nonsteroidal anti-inflammatory medication (NSAID) in the treatment of plantar fasciitis: A randomized, prospective, placebo-controlled study. Foot Ankle Int. 2007;28:20-23.
20 Turlik MA, Donatelli TJ, Veremis MG. A comparison of shoe inserts in relieving mechanical heel pain. Foot. 1999;9:84-87.
21 Kogler GF, Solomonidis SE, Paul JP. Biomechanics of longitudinal arch support mechanisms in foot orthoses and their effect on plantar aponeurosis strain. Clin Biomech (Bristol, Avon). 1996;11:243-252.
22 Landorf KB, Keenan A-M, Herbert RD. Effectiveness of foot orthoses to treat plantar fasciitis: A randomized trial. Arch Intern Med. 2006;166:1305-1310.
23 Pfeffer G, Bacchetti P, Deland J, et al. Comparison of custom and prefabricated orthoses in the initial treatment of proximal plantar fasciitis. Foot Ankle Int. 1999;20:214-221.
24 Martin JE, Hosch JC, Goforth WP, et al. Mechanical treatment of plantar fasciitis. A prospective study. J Am Podiatr Med Assoc. 2001;91:55-62.
25 Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006;27:606-611.
26 Winemiller MH, Billow RG, Laskowski ER, et al. Effect of magnetic vs sham-magnetic insoles on plantar heel pain: A randomized controlled trial [erratum appears in JAMA. 2004 Jan 7;291(1):46]. JAMA. 2003;290:1474-1478.
27 Probe RA, Baca M, Adams R, et al. Night splint treatment for plantar fasciitis. A prospective randomized study. Clin Orthop Relat Res. 1999:190-195.
28 Roos E, Engstrom M, Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006;27:606-611.
29 Powell M, Post WR, Keener J, et al. Effective treatment of chronic plantar fasciitis with dorsiflexion night splints: A crossover prospective randomized outcome study. Foot Ankle Int. 1998;19:10-18.
30 Tisdel CL, Harper MC. Chronic plantar heel pain: Treatment with a short leg walking cast. Foot Ankle Int. 1996;17:41-42.
31 Gudeman SD, Eisele SA, Heidt RSJr, et al. Treatment of plantar fasciitis by iontophoresis of 0.4% dexamethasone. A randomized, double-blind, placebo-controlled study. Am J Sports Med. 1997;25:312-316.
32 Crawford F, Atkins D, Young P, et al. Steroid injection for heel pain: Evidence of short-term effectiveness. A randomized controlled trial. Rheumatology. 1999;38:974-977.
33 Porter MD, Shadbolt B. Intralesional corticosteroid injection versus extracorporeal shock wave therapy for plantar fasciopathy. Clin J Sport Med. 2005;15:119-124.
34 Babcock MS, Foster L, Pasquina P, et al. Treatment of pain attributed to plantar fasciitis with botulinum toxin A: A short-term, randomized, placebo-controlled, double-blind study. Am J Phys Med Rehabil. 2005;84:649-654.
35 Perez M, Weiner R, Gilley JC. Extracorporeal shockwave therapy for plantar fasciitis. Clin Podiatr Med Surg. 2003;20:323-334.
36 Haake M, Wessel C, Wilke A. [Effects of extracorporeal shockwaves (ESW) on human bone marrow cell cultures]. Biomed Tech (Berl). 1999;44:278-282.
37 Plaisier PW, van der Hul RL, Terpstra OT, et al. Current role of extracorporeal shockwave therapy in surgery. Br J Surg. 1994;81:174-181.
38 Wilner JM, Strash WW. Extracorporeal shockwave therapy for plantar fasciitis and other musculoskeletal conditions utilizing the Ossatron—an update. Clin Podiatr Med Surg. 2004;21:441-447.
39 Trebinjac S, Muji-Skiki E, Ninkovi M, et al: Extracorporeal shock wave therapy in orthopaedic diseases. Bosn J Basic Med Sci 5:27–32, 200.
40 Thomson CE, Crawford F, Murray GD. The effectiveness of extra corporeal shock wave therapy for plantar heel pain: A systematic review and meta-analysis. BMC Musculoskelet Disord. 2005;6:19.
41 Buchbinder R, Ptasznik R, Gordon J, et al. Ultrasound-guided extracorporeal shock wave therapy for plantar fasciitis: A randomized controlled trial. JAMA. 2002;288:1364-1372.
42 Haake M, Buch M, Schoellner C, et al. Extracorporeal shock wave therapy for plantar fasciitis: Randomised controlled multicentre trial. BMJ. 2003;327:75.
43 Speed CA, Nichols D, Wies J, et al. Extracorporeal shock wave therapy for plantar fasciitis. A double blind randomised controlled trial. J Orthop Res. 2003;21:937-940.
44 Ogden JA, Alvarez R, Levitt R, et al. Shock wave therapy for chronic proximal plantar fasciitis. Clin Orthop Relat Res. 2001:47-59.
45 Rompe JD, Decking J, Schoellner C, et al. Shock wave application for chronic plantar fasciitis in running athletes. A prospective, randomized, placebo-controlled trial. Am J Sports Med. 2003;31:268-275.
46 Malay DS, Pressman MM, Assili A, et al. Extracorporeal shockwave therapy versus placebo for the treatment of chronic proximal plantar fasciitis: Results of a randomized, placebo-controlled, double-blinded, multicenter intervention trial. J Foot Ankle Surg. 2006;45:196-210.
47 Theodore GH, Buch M, Amendola A, et al. Extracorporeal shock wave therapy for the treatment of plantar fasciitis. Foot Ankle Int. 2004;25:290-297.
48 Schepsis AA, Leach RE, Gorzyca J. Plantar fasciitis. Etiology, treatment, surgical results, and review of the literature. Clin Orthop. 1991;266:185-196.
49 Davies MS, Weiss GA, Saxby TS. Plantar fasciitis: How successful is surgical intervention? Foot Ankle Int. 1999;20:803-807.
50 Allen BH, Fallat LM, Schwartz SM. Cryosurgery: An innovative technique for the treatment of plantar fasciitis. J Foot Ankle Surg. 2007;46:75-79.
51 Brugh AM, Fallat LM, Savoy-Moore RT. Lateral column symptomatology following plantar fascial release: A prospective study. J Foot Ankle Surg. 2002;41:365-371.
52 Woelffer KE, Figura MA, Sandberg NS, et al. Five-year follow-up results of instep plantar fasciotomy for chronic heel pain. J Foot Ankle Surg. 2000;39:218-223.
53 Brown JN, Roberts S, Taylor M, et al. Plantar fascia release through a transverse plantar incision. Foot Ankle Int. 1999;20:364-367.
54 Boyle RA, Slater GL. Endoscopic plantar fascia release: A case series. Foot Ankle Int. 2003;24:176-179.
55 Fishco WD, Goecker RM, Schwartz RI. The instep plantar fasciotomy for chronic plantar fasciitis. A retrospective review. J Am Podiatr Med Assoc. 2000;90:66-69.
56 Vohra PK, Giorgini RJ, Sobel E, et al. Long-term follow-up of heel spur surgery. A 10-year retrospective study. J Am Podiatr Med Assoc. 1999;89:81-88.
57 Saxena A. Uniportal endoscopic plantar fasciotomy: A prospective study on athletic patients. Foot Ankle Int. 2004;25:882-889.
58 Fishco WD, Goecker RM, Schwartz RI. The instep plantar fasciotomy for chronic plantar fasciitis. A retrospective review. J Am Podiatric Med Assoc. 1998;90:66-69.
59 Baxter DE, Pfeffer GB. Treatment of chronic heel pain by the surgical release of the first branch o the lateral plantar nerve. Clin Orthop. 1992;279:229-236.
60 Labib SA, Gould JS, Rodriguez-del-Rio FA, Lyman S. Heel pain triad (HPT): The combination of plantar fasciitis, posterior tibial tendon dysfunction and tarsal tunnel syndrome. Foot Ankle Int. 2002;23:212-220.
61 Barrett SL, Day SV, Pignetti TT, et al. Endoscopic planter fasciotomy: A multi-surgeon prospective analysis of 652 cases. J Foot Ankle Surg. 1995;34:400-407.
62 Tomczak RL, Haverstock BD. A retrospective comparison of endoscopic plantar fasciotomy to open plantar fasciotomy with heel spur resection for chronic plantar fasciitis/heel spur surgery. J Foot Surg. 1995;34:305-311.
63 Young MA, Cook JL, Webster KE. The effect of topical wheatgrass cream on chronic plantar fasciitis: A randomized, double-blind, placebo-controlled trial. Complement Ther Med. 2006;14:3-9.
64 Basford JR, Malanga GA, Krause DA, et al. A randomized controlled evaluation of low-intensity laser therapy: Plantar fasciitis. Arch Phys Med Rehabil. 1998;79:249-254.
65 Batt ME, Tanji JL, Skattum N. Plantar fasciitis: A prospective randomized clinical trial of the tension night splint. Clin J Sport Med. 1996;6:158-162.
66 Kudo P, Dainty K, Clarfield M, et al. Randomized, placebo-controlled, double-blind clinical trial evaluating the treatment of plantar fasciitis with an extracoporeal shockwave therapy (ESWT) device: a North American confirmatory study. J Orthop Res. 2006;24(2):115-123.