Chapter 75 What Is the Best Treatment for Displaced Intra-Articular Calcaneal Fractures?
All patients who present with a displaced intraarticular calcaneal fracture should be treated initially with rest, ice, compression, and elevation. After initial assessment of the injured patient, decision making becomes much more difficult. Certain factors in patients with displaced intra-articular calcaneal fractures are critically important in deciding whether to operate.1
An early (1976) Level II study2 demonstrated that more patients in the group who had a surgical reduction of their subtalar joint had resumed heavy work. Other studies, reviews, and meta-analyses have shown consistent direction that surgical treatment provides slight advantages in certain circumstances for individual patients with defined patient and fracture factors.3–9
TREATMENT OPTIONS
Nonoperative Treatment
A common theme among prospective trials of operative versus nonoperative treatment for displaced intra-articular calcaneal fractures is that the hindfoot becomes stiff when immobilized. Because of this, nonoperative care was thought best without immobilization.2,6, 7 One small, randomized, controlled trial was quick to dismiss nonoperative care because operative care was much better in their Level II trial.9 However, nonoperative care has withstood the test of time in certain patient populations, especially those patients who are elderly, presenting with multiple medical problems, distal vascular insufficiency, or incorrigible smoking habits. This means ice, elevation, tensoring, and early range of motion establishing full weight bearing by 6 weeks. These patients, especially sedentary patients,1,6 have reasonable long-term results with nonoperative care.
Operative Reduction
The debate has raged over whether operative care is better than nonoperative care in many randomized clinical trials.2,6, 7, 9 However, one thing becomes clear with careful review of well-performed Level II studies with good follow-up and computerized tomography. Those cases where an operative reduction has been done perfectly end in a better result.6,10 Nonoperative care, when compared with operative care, has consistently less successful results. Interestingly, the worst outcomes appear to be in those patients who have had operative reduction and internal fixation with a less than optimal anatomic reduction proved by computerized tomography.6,10 This is also reinforced by a study11 in which all prospective randomized trials were reviewed to judge operative reduction. This study suggests that there was only weak evidence to support open reduction and internal fixation versus nonoperative care. There was weak evidence to show an improved plain radiographic anatomic alignment in this group of radiographic studies.7,9, 12
A common theme with these studies and the earlier-mentioned randomized, controlled trials is that patient selection is important. Simple, displaced fractures that can be easily reduced (Sanders type II)12 are best reduced surgically. Sanders type III and IV fractures (comminuted) are more difficult to reduce accurately and to maintain reduction.13
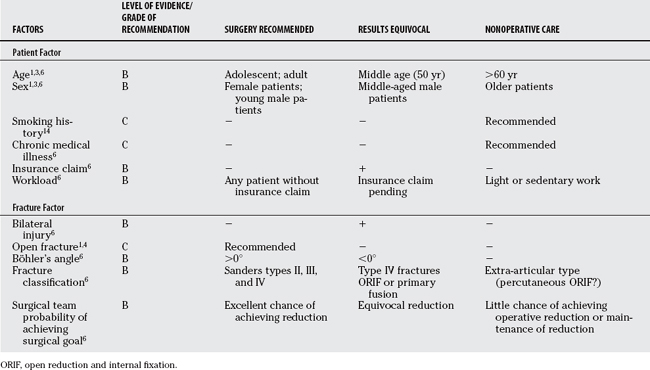
Another article has stated the significance of avoiding complications.14 Complications will often result in a less than optimal long-term result with problems such as pain, stiffness, or infection lessening the long-term outcome.1,6, 14 It is clear that complications occur regardless of management strategy (even by experienced surgeons). Complications are a cause of significant morbidity, especially failure to obtain and maintain a reduction, infection, and late and long-term stiffness.14 Surgeon decision making was thought to be crucial for patient outcome. The right patient must receive surgery to minimize possible complications (long-term problems from nonoperative care). The right patient should also be treated without surgery (to minimize operative complications in that patient deemed more suitably treated without surgery).1,14 The patient and fracture factors thought to be important include age, sex, smoking history, compensation claim information, workload on foot, fracture classification, bilaterality, and description of whether the calcaneus is an open or closed fracture.
EVIDENCE
Nonoperative Treatment
No Level I evidence provides guidance for treatment of displaced intra-articular calcaneal fractures. There are combinations of demographic groups or types of patients who are best treated by nonoperative care.1,6 Older patients (.60 years), medically unwell patients or unrepentant smokers, sedentary workers, or those with simple fractures patterns such as extra-articular type can be treated without surgery.1,6 The nonoperative protocol for these patients includes early range of motion, ice, elevation, and good follow-up. These decisions are based on the proviso that a computerized tomographic calcaneal scan demonstrates that the foot does not have any deformity. One of the features that was important from Howard and coauthors’14 article was that foot deformity treated without surgery will respond poorly, but given the fact that no gross foot deformity (marked varus or valgus) exists, this patient should have little in the way of complications and may be a candidate for nonoperative care.
Percutaneous Fixation
For those displaced fractures where full surgical approaches are not advisable (skin or soft-tissue concerns, elderly patients with vascular problems, or patients with diabetes), percutaneous fixation may be used. Essex-Lopresti15 introduced the use of the reduction technique with a posterior joystick elevating the depressed posterior facet. Tornetta16 reintroduced the percutaneous techniques for posterior facet percutaneous reduction more recently with a Level IV study. No Level I or II studies suggest that percutaneous reduction provides better long-term results for displaced intra-articular calcaneal fractures.
Operative Reduction
Once soft tissues have settled (7–10 days), operative treatment is suggested by a number of Level II studies.2–6,8–10 Young patients are found to respond better than older adult patients.6 Female patients may respond better than male patients with displaced intra-articular calcaneal fractures.6 Open fractures, because of the amount of energy and violence imparted with the foot injury, will have marked foot deformities and have better outcomes with operative care. If a patient presents with a Böhler’s angle of greater than 15 degrees, then operative care may be suggested because these patients will do better with operative strategies.6 Those with a Böhler’s angle of less than 0 degrees show equivocal results with operative care, although at least one study by Thordarson and Krieger9 suggests much better results with operative care. Simple fracture patterns, such as Sanders fracture types II and III, respond better with operative care.4,6 Fractures that are severely comminuted provide treatment dilemmas. Fractures with Sanders type IV characteristics can be treated with primary operative repair or primary fusion treatment. One study demonstrated that the amount of initial injury involved with the displaced intra-articular calcaneal fracture was a primary prognostic determinant of long-term patient outcome.17 Patients with Böhler’s angle presentation of less than 0 degrees were 10 times more likely to require late subtalar fusion than a Böhler’s angle presentation of greater than 15 degrees, whereas a Sanders type IV presentation was 5.5 times more likely to be fused than a simple Sanders type II fracture. Workers with insurance claims were three times more likely to need fusion than those without an insurance claim, whereas nonoperative care resulted in fusion six times more likely than in those patients treated with initial open reduction and internal fixation.17
AREAS OF UNCERTAINTY
Age
Ceccarelli and colleagues18 provided long-term follow-up care on calcaneal fractures in children. Children were defined as younger than 17 years. Those patients who presented with fractures when they were younger than 14 years responded well regardless of nonoperative or operative care. Those patients who were 15 to 17 years old responded better with operative care. This Level II study also showed that extra-articular fractures could be treated without surgery.
Workers’ Compensation (Insurance Claims)
Buckley and colleagues6 determined that results were equivocal with their Level II study when these patients suffered displaced intra-articular calcaneal fractures. Any patient without workers’ compensation insurance claim did better with operative care, whereas those patients with an insurance claim did not score as well on the standard scoring scales (scored 20 points less on a 100-point scoring scale).6
Bilateral
Patients with bilateral calcaneal injuries seem to have less successful outcomes than patients with one fracture.6 Gait and occupation are compromised. Treatment strategies are unclear.
Subtalar Fusion
Patients with severe fractures (Sanders type IV) on initial presentation may be treated operatively with primary reconstruction or fusion. No evidence has been reported that one is better than the other in the literature. However, late subtalar fusion is predicted by a number of presenting patient features.17 Importantly, those patients who were fused late (.6 months after injury) demonstrated outcome scores similar to those treated with surgery early.17 Level II evidence suggests that if someone is treated without surgery initially because of ongoing medical circumstance, but they require a late subtalar fusion for pain, then their outcome will be similar to patients who had early operative care.
GUIDELINES
The spectrum of care for displaced intra-articular calcaneal fractures is dependent on patient factors and fracture factors. Level II evidence suggests that young patients, any patient without a worker compensation insurance claim, and simple fracture types with good soft tissue will have optimal results with operative care.1,6, 10 Importantly, a surgeon must be wary of patient complications during surgery.14 Should complications occur, the outcome for the patient significantly lessens because of further surgical needs. The surgical team must be adept at provision of an accurate reduction. Level II evidence6,10 suggests that if the operative reduction is not well achieved and the surgical team is able only to achieve a partial reduction, then long-term outcome for the patient is compromised. Lastly, for patients who are medically unwell, older, have extra-articular fractures, or perform light or sedentary work, Level II evidence suggests nonoperative care may be the best choice.
Patient must be carefully assessed to ensure they are good operative candidates. Smoking cessation attempts and good soft-tissue care are mandated. Investigation with plain radiograph and computed tomographic scanning can quantify and qualify the type of fracture present. When nonsurgical management is chosen, functional care is preferable to casting with early motion, non–weight bearing, and stretching. At 6 weeks, progressive weight bearing can be started with the use of custom orthoses and good footwear.1
Surgery is the standard of care for most displaced intra-articular fractures of the calcaneus. Skeletally mature patients,18 young adult patients,6 and any patient without an insurance claim6 should have operative reduction internal fixation with an experienced surgical team. Simple fracture types are more easily reduced and the fracture reductions maintained. Difficult reductions occur in the Sanders type III and IV fractures, and the surgeon must always be aware that “the achievement of a reduction and the maintenance of a reduction” determines whether a patient will have a good result.6,10 If the result is compromised with a less than adequate surgical procedure, then the patient will probably have results that are equal to or no better than nonoperative care.6 Complications must be avoided because patients with complications will have less successful results and long-term outcome.1,14 Subtalar arthritis, if it does occur, may be treated with late subtalar fusion17 with good results.
In conclusion, this clinical scenario has proved to be a clinical conundrum. Unfortunately, the surgical team may focus on the fracture and may overlook significant patient characteristics that could help in guiding optimal patient care. Operative management is the treatment of choice as long as complications can be minimized. Nonoperative care can lead to successful results in select patients in a high percentage of cases. Table 75-1 provides a summary of recommendations for the treatment of displaced intraarticular calcaneal fractures.
1 Buckley R, Tough S. Displaced intra-articular calcaneal fractures. J Am Acad Orthop Surg. 2004;12:172-178.
2 Aaron D, Howat T. Intra-articular fractures of the calcaneum. Injury. 1976;7:205-211.
3 Bajammal S, Tornetta IP, Sanders D, et al. Displaced intra-articular calcaneal fractures. J Orthop Trauma. 2005;19:360-364.
4 Bridgman S, Dunn K, McBride D, et al. Interventions for treating calcaneal fractures. Cochrane Database Syst Rev. 2000:CD001161.
5 Bridgeman S, Dunn K, McBride D, et al. Interventions for treating calcaneal fractures. Foot. 2002;12:47-61.
6 Buckley R, Tough S, McCormack R, et al. Operative compared with non-operative treatment of displaced intra-articular calcaneal fractures: A prospective randomized controlled multi-centre trial. J Bone Joint Surg Am. 2002;84:1733-1744.
7 Parmar H, Triffitt P, Gregg P. Intra-articular fractures of the calcaneum treated operatively or conservatively, a prospective study. J Bone Joint Surg Br. 1993;75:932-937.
8 Randle J, Kreder H, Stephen D, et al. Should calcaneal fractures be treated surgically? Meta-analysis. Clin Orthop Relat Res. 2000:217-227.
9 Thordarson D, Krieger L. Operative vs. non-operative treatment of intra-articular fractures of the calcaneus: A prospective randomized trial. Foot Ankle Int. 1996;17:2-9.
10 Richards P, Bridgman S. Review of the radiology in randomized controlled trials in open reduction and internal fixation (ORIF) of displaced intra-articular calcaneal fractures. Injury. 2001;32:633-636.
11 O’Farrell D, O’Byrne J, McCabe J, et al. Fractures of the os calcis: improved results with internal fixation. Injury. 1993;24:263-265.
12 Sanders R. Intra-articular fractures of the calcaneus: Present state of the art. J Orthop Trauma. 1992;6:252-265.
13 Longino D, Buckley R. Bone graft in the operative treatment of displaced intra-articular calcaneal fractures: Is it helpful? J Orthop Trauma. 2001;15:280-286.
14 Howard J, Buckley R, McCormack R, et al. Complications following management of displaced intra-articular calcaneal fractures: A prospective randomized trial comparing open reduction internal fixation with non-operative management. J Orthop Trauma. 2003;17:241-249.
15 Essex-Lopresti P. The mechanism, reduction technique and results in fractures of the os calcis. Br J Surg. 1952;39:395-419.
16 Tornetta P. The Essex-Lopresti reduction for calcaneal fractures revisited. J Orthop Trauma. 1998;12:469-473.
17 Csizy M, Buckley R, Tough S, et al. Displaced intra-articular calcaneal fractures: Variables predicting late subtalar fusion. J Orthop Trauma. 2003;17:106-112.
18 Ceccarelli F, Faldini C, Piras F, et al. Surgical vs. non-surgical treatment of calcaneal fractures in children: A long term results comparative study. Foot Ankle Int. 2000;21:825-832.