Chapter 11 What Is the Best Treatment for Displaced Fractures of the Distal Radius?
The optimal treatment for displaced distal radius fractures is unclear. Despite a literature filled with hundreds of studies examining biomechanics, treatment outcomes, and techniques, level I evidence is limited and does not provide an unambiguous answer. Many “prospective randomized” studies before 2000 have significant methodologic errors. Yet, more recent studies utilizing stringent blinding and more reproducible evaluation methods may offer some insight into choosing a treatment method.
EVIDENCE (LEVEL I AND II EVIDENCE)
Handoll and Madhok1,2 performed a systematic review of the distal radius fracture literature before 2000. Significant methodologic deficiencies abounded: Most series had a small number of patients, allocation concealment was deficient in 42 of 44 studies, and a majority of outcomes were reported using a modified Gartland and Werley scheme, a nonvalidated surgeon-generated outcome measure. Despite these deficiencies, their systematic review suggests that external fixation and percutaneous pinning have better radiographic outcomes and may have improved functional outcomes compared with closed reduction and casting.
Studies after 2000 with improved methodology confirm results of previous studies. In a level I study, Kreder and colleagues3 compared spanning external fixation to closed reduction and casting in distal radius fractures without joint incongruity and found trends toward improved 36-Item Short Form Health Survey (SF-36) bodily pain scores and Musculoskeletal Functional Assessment (MFA) scores at 2 years; however, these trends did not reach statistical significance. Radiologic outcomes also showed a trend that approached significance that favored external fixation. Comparisons of percutaneous pinning to closed reduction using validated outcomes also found that radiographic parameters were significantly improved with pinning; however, there was no difference in the SF-36 score.4 Harley and colleagues’5 level I study also examined outcomes of augmented external fixation versus percutaneous pinning at 1 year. Although validated and functional outcomes were similar, external fixation demonstrated better articular congruity on radiographic follow-up.
External fixation has also been compared with internal fixation. When comparing dorsal pi plating with external fixation in a level II study, Grewal and investigators6 found no significant difference in Disabilities in Arm, Shoulder, and Hand (DASH) or SF-36 scores; however, the pi plate group had significantly weaker grip strengths and greater number of complications, especially tendonitis and the need for hardware removal. Kreder and colleagues7 in a multicenter level I study found that although MFA and SF-36 scores were similar at 2 years between both external fixation with indirect reduction and percutaneous pinning and open reduction, internal fixation was statistically equivalent, internal fixation yielded a better SF-36 bodily pain subscore, but external fixation yielded better grip strengths at the 6-month period.
Although many studies have confirmed previous conclusions, some newer studies have brought these conclusions under question. In a 1998 level II study, McQueen8 found that nonbridging external fixation yielded better radiographic results, grip strength, and flexion than bridging external fixation. However, Atroshi and colleagues9 found that in a level I study, although radiographic outcomes were improved in patients treated with nonbridging fixators, DASH scores were statistically equivalent.
Trials have also examined adjunctive bone graft substitutes. In a level II randomized, controlled trial by Sanchez-Sotelo and coauthors,10 Norian-treated wrists had better functional outcomes compared with wrists treated with closed reduction and casting. In the regression analysis, treatment without Norian increased the probability of a poor functional result by 12 and increased the probability of malunion by 11. Cassidy and colleagues11 compared Norian SRS-treated wrists with external fixation in a level I study and found better subjective outcomes at 6 weeks; however, no significant clinical differences were observed at 1 year.
With regard to external fixation, Werber and researchers’12 level II study demonstrated that use of a five-pin external fixator with one pin supporting the radial articular fragment yielded better radiographic and functional outcomes than a standard four-pin fixator. Egol and coworkers’13 level I study demonstrated no significant difference in the incidence of pin-site infection regardless of pin-site care using dry dressings, peroxide pin-site care, or chlorhexidine impregnated discs.
AREAS OF UNCERTAINTY (LEVEL II AND III EVIDENCE)
Plating Techniques
A number of new plating techniques have become popular since the late 1990s. Volar fixed-angle plating was introduced with the pi plate in the late 1980s,14 but now has undergone a renaissance. Orbay and Fernandez15,16 have popularized this concept, and fixed-angle volar plating is now again in widespread use. Low-profile dorsal plating and different forms of fragment-specific fixation methods have been used successfully as documented in level IV case series.17,18
Despite this explosion of different types of plates and plating techniques, limited evidence has compared these different techniques. In Ruch and Papadonikolakis’s19 level III case–control series, no difference existed in the DASH between volar nonlocking plating versus dorsal nonlocking plating. In Koshimune and colleagues’20 level II study, there was no clear advantage of volar locked versus volar nonlocked plating when evaluating radiographic parameters of palmar inclination, radial tilt, and radial length as final outcome.
Rehabilitation
Handoll and Madhok21 also performed a systematic review of literature examining optimal methods for rehabilitation after surgical fixation of distal radius fracture. Despite the 15 trials that were able to be included in the review, the authors conclude that no specific guidelines can be made regarding rehabilitation after distal radius fracture.
Progression to Arthrosis
Previous studies have documented a statistical association with intra-articular step-off with radiographic arthrosis.22 Kreder and investigators’3 level I study from 2006 demonstrated that patients with a residual step-off were 10 times more likely to experience development of radiographic arthrosis. Patients with a step-off greater than 2 mm were eight times more likely to develop radiographic arthrosis than patients with a step-off less than 2 mm. Despite these dramatic numbers, the clinical impact of this radiographic arthrosis is unclear. A level II prospective, randomized trial by Young and coworkers’23 with 7-year follow-up of 85 patients from the United Kingdom demonstrated radiographic arthrosis in 20 patients, but clinically significant arthrosis in only one patient. Goldfarb et al. demonstrated that radiographic arthrosis was present in 13 of 16 wrists at fifteen years after distal radius fracture, however clinical function was quite good despite the radiographic appearance.24a Long-term studies will be necessary to elucidate the incidence of clinically significant radiocarpal arthrosis after distal radius fracture, and it is likely that only a large cohort of patients will be able to distinguish whether one intervention is better than another in preventing clinical arthrosis.
CASE SERIES FOR FURTHER STUDY (LEVEL IV AND V EVIDENCE)
A number of authors have reported case series of different methods of plate fixation using various outcome measures ranging from Gartland and Werley functional scores to DASH and SF-36 scores.15–17,24–26 This recent rash of case reports on plating reflect a growing worldwide trend favoring plate fixation; subsequently, they should be examined critically.
Case series involving volar-fixed angle plating demonstrated success in the potentially osteopenic elderly population16 and also demonstrated DASH and Gartland and Werley scores comparable with previous series using other techniques.26 Harness and colleagues27 reported on a cohort of seven patients whose volar plating construct lost fixation. Careful review of this cohort found that the stand-ard volar implants used did not adequately support the ulnar volar margin of the lunate facet. Dorsal plating series report minimal problems with extensor tendon irritation at 18 months with rare plate removal.17,25 DASH and Gartland and Werley scores were also similar to other functional outcomes studies.
Application of Evidence
Grade C Recommendations, Poor Evidence
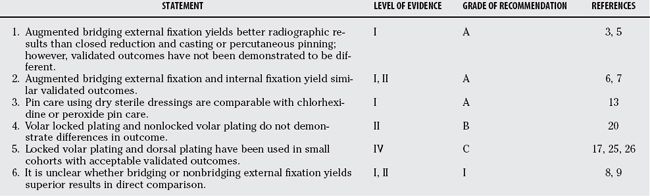
Loss of lunate facet fixation can compromise the overall result. As such, surgeons should be particularly wary of distal fractures of the intermediate column. Extensor tenosynovitis continues to be a complication with both volar and dorsal plating. No level I evidence shows that these complications occur at a lower rate than with other plating methods; however, in case series compared with historical controls, the incidence may be lower. It is reasonable to utilize newer plate technologies whereas paying close attention to noted potential complications. Table 11-1 provides a summary of recommendations for treatment of displaced fractures of the distal radius.
1 Handoll HH, Madhok R. Surgical interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev.; 3; 2003; CD003209.
2 Handoll HH, Madhok R. Surgical interventions for treating distal radial fractures in adults. Cochrane Database Syst Rev.; 3; 2001; CD003209.
3 Kreder HJ, Agel J, McKee MD, et al. A randomized, controlled trial of distal radius fractures with metaphyseal displacement but without joint incongruity: Closed reduction and casting versus closed reduction, spanning external fixation, and optional percutaneous K-wires. J Orthop Trauma. 2006;20:115-121.
4 Azzopardi T, Ehrendorfer S, Coulton T, et al. Unstable extra-articular fractures of the distal radius. J Bone Joint Surg Br. 2005;87:837-840.
5 Harley BJ, Scharfenberger A, Beaupre LA, et al. Augmented external fixation versus percutaneous pinning and casting for unstable fractures of the distal radius—A prospective randomized trial. J Hand Surg [Am]. 2004;29:815-824.
6 Grewal R, Perey B, Wilmink M, et al. A randomized prospective study on the treatment of intra-articular distal radius fractures: Open reduction and internal fixation with dorsal plating versus mini open reduction, percutaneous fixation, and external fixation. J Hand Surg [Am]. 2005;30:764-772.
7 Kreder HJ, Hanel DP, Agel J, et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius. J Bone Joint Surg Br. 2005;87:829-836.
8 McQueen MM. Redisplaced unstable fractures of the distal radius: A randomized, prospective study of bridging versus non-bridging external fixation. J Bone Joint Surg Br. 1998;80:665-669.
9 Atroshi I, Brogren E, Larsson G-U, et al. Wrist-bridging versus non-bridging external fixation for displaced distal radius fractures: A randomized assessor-blind clinical trial of 38 patients followed for 1 year. Acta Orthop. 2006;77:445-453.
10 Sanchez-Sotelo J, Munuera L, Madero R. Treatment of fractures of the distal radius with a remodellable bone cement: A prospective randomized study using Norian SRS. J Bone Joint Surg Br. 2000;82:856-863.
11 Cassidy C, Jupiter JB, Cohen M, et al. Norian SRS cement compared with conventional fixation in distal radial fractures. J Bone Joint Surg Am. 2003;85:2127-2136.
12 Werber KD, Raeder F, Brauer RB, et al. External fixation of distal radial fractures: Four compared with five pins: A randomized prospective study. J Bone Joint Surg Am. 2003;85:660-666.
13 Egol KA, Paksima N, Puopolo S, et al. Treatment of external fixation pins about the wrist: A prospective, randomized trial. J Bone Joint Surg Am. 2006;88:349-354.
14 Ring D, Jupiter JB, Brennwald J, et al. Prospective multicenter trial of a plate for dorsal fixation of distal radius fractures. J Hand Surg [Am]. 1997;22:777-784.
15 Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: A preliminary report. J Hand Surg [Am]. 2002;27:205-215.
16 Orbay JL, Fernandez DL. Volar fixed-angle plate fixation for unstable distal radius fractures in the elderly patient. J Hand Surg [Am]. 2004;29:96-102.
17 Simic PM, Robison J, Gardner MJ, et al. Treatment of distal radius fractures with a low-profile dorsal plating system: An outcomes assessment. J Hand Surg [Am]. 2006;31:382-386.
18 Benson LS, Minihane KP, Stern LD, et al. The outcome of intra-articular distal radius fractures treated with fragment-specific fixation. J Hand Surg [Am]. 2006;31:1333-1339.
19 Ruch DS, Papadonikolakis A. Volar versus dorsal plating in the management of intra-articular distal radius fractures. J Hand Surg [Am]. 2006;31:9-16.
20 Koshimune M, Kamano M, Takamatsu K, et al. A randomized comparison of locking and non-locking palmar plating for unstable Colles’ fractures in the elderly. J Hand Surg [Br]. 2005;30:499-503.
21 Handoll HH, Madhok R, Howe TE. Rehabilitation for distal radial fractures in adults. Cochrane Database Syst Rev. 2006;3:CD003324.
22 Knirk JL, Jupiter JB. Intra-articular fractures of the distal end of the radius in young adults. J Bone Joint Surg Am. 1986;68:647-659.
23 Young CF, Nanu AM, Checketts RG. Seven-year outcome following Colles’ type distal radial fracture. A comparison of two treatment methods. J Hand Surg [Br]. 2003;28:422-426.
24 Rozental TD, Beredjiklian PK, Bozentka DJ. Functional outcome and complications following two types of dorsal plating for unstable fractures of the distal part of the radius. J Bone Joint Surg Am. 2003;85:1956-1960.
24a Goldfarb CA, Rudzki JR, Catalano LW, Hughes M, Borrelli JJr. Fifteen-year outcome of displaced intra-articular fractures of the distal radius. J Hand Surg [Am]. 2006 Apr;31(4):633-639.
25 Kamath AF, Zurakowski D, Day CS. Low-profile dorsal plating for dorsally angulated distal radius fractures: An outcomes study. J Hand Surg [Am]. 2006;31:1061-1067.
26 Rozental TD, Blazar PE. Functional outcome and complications after volar plating for dorsally displaced, unstable fractures of the distal radius. J Hand Surg [Am]. 2006;31:359-365.
27 Harness NG, Jupiter JB, Orbay JL, et al. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004;86:1900-1908.