Chapter 12 What Is the Best Surgical Treatment for Early Degenerative Osteoarthritis of the Wrist?
SCAPHOTRAPEZIOTRAPEZOID JOINT ARTHRITIS
Evidence
In his monumental review of 800 triscaphe fusions, Dr. Watson1 does identify 98 patients whose arthrodesis was for primary STT arthritis. The case series review states that 62% of the patients were examined in the office and the others had data pulled from chart reviews. The mean follow-up was 3.4 years. Patients were immobilized for 3 weeks in a long arm cast, followed by 3 weeks in a short arm cast. Pain was graded by the patients as mild, moderate, or severe. The flexion extension arc was 85% and 80%, respectively, of the contralateral side. Grip strength was 77% of the other side. The results with regard to pain were not broken out independently for STT arthritis versus other indications for STT fusion. The rate of nonunion across all indications for STT arthrodesis was only 4%.
In a review of eight patients with STT arthritis, Srinivasan and Matthews2 found four were pain free, three had pain with certain activities, and one had constant pain. The flexion extension arc averaged 115 degrees compared with 124 degrees on the uninjured side. One of the eight had a nonunion. Follow-up averaged 4 years.
Only one case series describes results of distal scaphoid excision specifically for STT arthritis.3 Garcia-Elias and colleagues3 reported on 21 patients with a mean follow-up of 29 months. Patients were immobilized for 2 to 3 weeks in a short arm splint. The preoperative visual analog scale (VAS) pain score was 7.5, and the postoperative score was 0.6, with 13 having no pain. Grip improved from 57% of the contralateral side preoperatively to 83% of the contralateral side after surgery. Wrist flexion averaged 57 degrees and wrist extension averaged 61 degrees. The radiolunate angle increased from 9 degrees before surgery to 17 degrees after surgery.
SCAPHOLUNATE ADVANCED COLLAPSE AND SCAPHOID NON-UNION ADVANCED COLLAPSE
The two most common surgical options for chronic SLAC and SNAC wrist are either a proximal row carpectomy (PRC) or a four-corner (Capitate–Lunate–Hamate–Triquetrum) fusion. Proponents of PRC point to its technical simplicity, decreased time for immobilization, and lack of nonunion risk. Proponents of four-corner fusion highlight the maintenance of physiologic carpal height and a congruent radiolunate joint, which may theoretically allow a more durable articulation.
Evidence
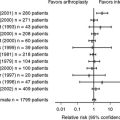
No randomized trials have compared PRC with a four-corner fusion (Level I). No prospective comparative studies exist (Level II). Four retrospective comparative studies (Level III) have been reported, only one of which has a methodology that would minimize patient selection bias and the results of which might therefore be valid.4–7
The highest quality study, by Cohen and Kozin4 in 2001, retrospectively examined 2 cohorts of 19 patients at different institutions, which performed exclusively either PRC or four-corner fusions. Importantly, there were no preoperative differences with regard to age, sex, stage of arthritis, or preoperative pain or function. All patients were stage II, except one four-corner patient who was stage III. The most significant limitation is that the follow-up averaged 19 months for the PRC group and 28 months for the four-corner group. Typically, these procedures are performed on patients with the hope of decades of postoperative functionality, thus any conclusion based on 2 years of follow-up is limited. Nevertheless, it avoids the selection bias in other comparative studies where patients had one or the other procedure based on surgeon preference.
Wyrick and coworkers’5 retrospective review of 17 patients with four-corner and 10 patients with PRC treatment with a 27-month mean follow-up showed better grip strength, range of motion, and pain relief with a PRC.5 There were three nonunions in the arthrodesis group, only one of which was symptomatic. However, five of the patients with four-corner fusion required revision surgery, whereas none of the patients with PRC required revision.
Tomaino and researchers’6 retrospective review examined 15 patients with PRC and 9 patients with arthrodesis at an average of 5.5 years. Mean postoperative pain and grip scores were comparable. PRC preserved a greater arc of motion, 77 versus 52 degrees for arthrodesis. Three patients with PRC treatment were unsatisfied, and one went on to a wrist fusion.
Krakauer and coauthors’ retrospective review7 compares results of mostly stage II PRC patients with mostly stage III four-corner patients and is therefore not believed to be helpful in providing a valid comparison of the two procedures.
OSTEOARTHRITIS OF THE DISTAL RADIOULNAR JOINT
Osteoarthritic changes at the distal radioulnar joint (DRUJ) are a challenging surgical dilemma. Our understanding of the anatomy and biomechanics of the joint and the related surgical options have increased substantially over the past two decades. In this analysis, we are focusing specifically on osteoarthritis of the DRUJ and not ulnocarpal impingement or other causes of ulnar-sided wrist pain and arthrosis. The most common surgical techniques have been complete distal resection (Darrach), hemiresection (with or without soft tissue interposition), Sauve–Kapandji (SK), or prosthetic replacement.
Evidence
Minami and colleagues8 retrospectively compare the results of 20 Darrach resections with 25 SK and 16 hemiresections for DRUJ osteoarthritis. The follow-up was impressively a minimum of 5 years and a mean of 8 of 11 years. The authors originally performed Darrach resections on all patients with symptomatic DRUJ osteoarthritis. Later, they performed SK procedures if the triangular fibrocartilage complex (TFCC) could not be reconstructed or there was positive ulnar variance of greater than 5 mm. If the TFCC was intact or reconstructible, a hemiresection with interposition (e.g., Bowers) was performed. Unfortunately, the Darrach resection group was older (68 versus 53 SK or 60 hemiresections), and 75% were arthritic changes caused by prior distal radius trauma, whereas only about 25% of the SK and hemiresection group conditions were due to secondary osteoarthritis and 75% were due to primary or idiopathic osteoarthritis. No ordinal preoperative pain scoring is available with which to compare postoperative pain results. These points make any comparison of postoperative pain, grip, or range of motion questionable. Of note, 40% of patients who had undergone Darrach resections had no postoperative pain, 20% had slight pain, 25% had moderate pain, and 15% had severe pain. Grip strength decreased in 65% of patients with a Darrach resection.
Watson and Gabuzda9 reviewed results from 32 patients with matched hemiresection without interposition for post-traumatic osteoarthritis of the DRUJ. Two patients in the series had Madelung’s deformity, and three had previously undergone a Darrach procedure. Twenty-one were examined personally and 11 by telephone. Follow-up averaged 51 months. Of the 21 patients examined, 6 experienced residual pain at the DRUJ. Of the 11 questioned by telephone, 5 had no pain, 3 had mild pain, 2 had moderate pain, and 1 had severe pain. Revisions for radioulnar impingement were performed on three patients.
Van Schoonhoven and coworkers10 evaluated 36 patients with matched hemiresection with interposition for post-traumatic osteoarthritis of the DRUJ with an average follow-up of 34 months. Preoperative pain scores measured 7.8, whereas postoperative scores were 3.9. Grip strength improved from 40% to 64% of the uninjured side. In 21 patients, radioulnar impingement was observed and required revision in 5 patients.
Lamey and Fernandez11 report on 18 patients with post-traumatic osteoarthritic changes of the DRUJ treated with a modified SK procedure. Follow-up averaged 4 years. Supination improved dramatically from 16 degrees before surgery to 76 degrees after surgery, and pronation improved from 42 to 81 degrees. Grip strength went from 36% of the unaffected side to 73% of the unaffected side. Fifteen patients reported no pain in the area of the DRUJ, and three reported mild pain with rotation. Eleven patients had repeat operations, primarily for removal of hardware. The ulnar stump was reported as stable in 16 patients.
The use of ulnar head prosthesis for salvage of failed distal ulnar resections has been reported. Results of ulnar head prosthetics for salvage or primary indications has been promising. For example, Schecker and Severo12 reported on 23 patients, but with a mean follow-up of only 15 months. All 23 patients were reported to be free of pain with a normal pronation/supination arc. Eight of the 13 patients who were out of work because of DRUJ disability returned to work. Implant longevity, given the short follow-up of most of these case series on prosthetic options, continues to be a concern.
Persistent pain or stump instability continues to plague most proposed treatments for DRUJ arthritis. If the newer generation of ulnar head prosthetic replacements demonstrates durable results with time, they may be a preferred solution for some patients. The data to support any of these prosthetics in general or to support the preferential use of one prosthesis over another certainly does not exist yet. Table 12-1 provides a summary of recommendations.
| CONDITION | GRADE | RECOMMENDATION |
|---|---|---|
| STT arthritis | I | Insufficient evidence exists to allow a recommendation for or against STT arthrodesis versus distal scaphoid excision for the treatment of primary STT arthritis. |
| SLAC/SNAC | I | Insufficient evidence exist to suggest a PRC or a four-corner arthrodesis as the preferable treatment for stage II arthritic changes in a SLAC or SNAC wrist. |
| DRUJ arthritis | I | Insufficient evidence exists to suggest a preferred treatment for osteoarthritis of the DRUJ. |
DRUJ, distal radioulnar joint; PRC, proximal row carpectomy; SLAC, scapholunate advanced collapse; SNAC, scaphoid nonunion advanced collapse; STT, scaphotrapeziotrapezoid.
1 Watson KH, Wollstein R, Joseph E, et al. Scaphotrapeziotrapezoid arthrodesis: A follow-up study. J Hand Surg [Am]. 2003;28:397-404.
2 Srinivasan VB, Matthews JP. Results of scaphotrapeziotrapeziod fusion for isolated idiopathic arthritis. J Hand Surg [Br]. 1996;21:378-380.
3 Garcia-Elias M, Lluch AL, Farreres A, et al. Resection of the distal scaphoid for scaphotrapeziotrapezoid osteoarthritis. J Hand Surg [Br]. 1999;24:448-452.
4 Cohen MS, Kozin SH. Degenerative arthritis of the wrist: Proximal row carpectomy versus scaphoid excision and four-corner arthrodesis. J Hand Surg [Am]. 2001;26:94-104.
5 Wyrick JD, Stern PJ, Kiefhaber TR. Motion-preserving procedures in the treatment of scapholunate advanced collapse wrist: Proximal row carpectomy versus four-corner arthrodesis. J Hand Surg [Am]. 1995;20:965-970.
6 Tomaino MW, Miller RJ, Cole I, Burton R: Scapholunate advanced collapse wrist: Proximal row carpectomy or limited wrist arthrodesis with scaphoid excision. J Hand Surg [Am] 19:134–142, 199.
7 Krakauer JD, Bishop AT, Cooney WP. Surgical treatment of scapholunate advanced collapse. J Hand Surg [Am]. 1994;19:751-759.
8 Minami A, Iwasaki N, Ishikawa J, et al. Treatments of osteoarthritis of the distal radioulnar joint: Long-term results of three procedures. Hand Surg. 2005;10:243-248.
9 Watson KW, Gabuzda GM. Matched distal ulna resection for posttraumatic disorders of the distal radioulnar joint. J Hand Surg [Am]. 1992;17:724-730.
10 Van Schoonhoven J, Kall S, Schober F, et al. The Hemiresection-interposition arthroplasty as a salvage procedure for the arthrotically destroyed distal radioulnar joint. Handchir. 2003;35:175-180.
11 Lamey DM, Fernandez DL. Results of the modified Sauve-Kapandji procedure in the treatment of chronic posttraumatic derangement of the distal radioulnar joint. J Bone Joint Surg Am. 1998;80:1758-1769.
12 Schecker LR, Severo A. Ulnar shortening for the treatment of early post-traumatic osteoarthritis at the distal radioulnar joint. J Hand Surg. 2001;26:41-44.