Chapter 10 What Is the Best Surgical Procedure for Cubital Tunnel Syndrome?
The second most common site of nerve compression in the upper extremity is the ulnar nerve in the region of the cubital tunnel. Until recently, the surgical management of cubital tunnel syndrome was represented in the literature by numerous case series with the authors reporting experience with a specific surgical procedure. Clinical research related to cubital tunnel syndrome answered many important questions about this disorder and its care; however, until recently, there has been only low-quality evidence supporting one type of surgical procedure over others.
In 1989, Dellon1 advocated a staging system for ulnar nerve compression at the elbow. He reviewed the literature and concluded that severity of compression, a characteristic he used to divide the syndrome into three stages, was an important prognostic factor and should be used to guide surgical management. Parallel to the staging of carpal tunnel syndrome, he divided cubital tunnel syndrome into “mild,” “moderate,” and “severe” stages. Although it remains unknown whether the stage of compression is an important guide for choice of surgery, if the prognosis of surgical care is related to the severity of compression, then this information would be useful in randomized trials to define the population and ensure balance of treatment groups.
For measurement of the results of cubital tunnel surgery, Kleinman and Bishop2 have devised a grading system. The domains include “satisfaction,” “improvement,” “severity of residual symptoms,” “work status,” “leisure activity,” “strength,” and “sensibility.”
This has been used widely since its introduction, and although it requires some measurement by a trained person, it is recommended for anyone performing clinical research in cubital tunnel syndrome. As a disorder causing symptoms and functional problems in the hand, in clinical research, some patient-oriented method of evaluation of the results of treatment should be used. The use of electrodiagnostic testing to measure the outcome of cubital tunnel surgery may be misleading. It has been reported that electrodiagnostic testing may not be accurate after anterior transposition.3 In addition, in other forms of nerve compression, electrodiagnostic tests may not return to normal despite good clinical results after surgery. The importance of these measurement issues in the use of electrical testing to evaluate the results of cubital tunnel surgery has not been explored. These concerns add to the importance of patient-oriented measures in outcomes research in cubital tunnel syndrome.
OPTIONS
Simple Release
The value of simple release of the ulnar nerve is that it is technically simple to perform and, if successful, causes the least morbidity for the patient. The surgery is of short duration and the postoperative care is simplified requiring no prolonged immobilization. This procedure leaves the nerve in its anatomic position, and therefore reduces the chance of inducing secondary compression by changing the anatomic course of the nerve. The concern with the procedure is that the nerve is left in a position behind the elbow where it can continue to undergo traction with full elbow flexion. Another potential problem is created because the nerve is released from its tethers within its anatomic bed. Theoretically, this increases the potential for subluxation of the nerve with flexion of the elbow. A variation of simple release is to use minimal incisions and some type of “endoscopic” visualization of the procedure. Nathan and colleagues4 report 89% good or excellent immediate postoperative relief of symptoms using simple decompression of the nerve in 164 nerves in 131 patients. At an average follow-up period of 4.3 years, 79% of patients still reported good or excellent relief.
Epicondylectomy
The nerve is released as in a simple release and a portion of the medial epicondyle is removed to perform medial epicondylectomy. This procedure also leaves the nerve in its anatomic position. By combining a simple release with epicondylectomy, theoretically, when the elbow flexes, the nerve will not snap over the medial epicondyle. A minimal degree of epicondylar excision appears to be as effective as a partial epicondylectomy.5
Intramuscular and Submuscular Transposition
For intramuscular and submuscular transposition, the nerve is removed from its anatomic location and placed within2 or deep to the flexor pronator muscle origin. In this procedure, the nerve is placed anterior to the elbow and is placed within a protective environment. The surgeon may introduce additional sites of compression, and the patient must have a period of postoperative immobilization to allow the flexor origin to heal. One variation is to perform lengthening of the flexor pronator origin to loosen this structure over the nerve. In Dellon’s6 report of submuscular transposition on 121 patients and 161 extremities using the musculofascial lengthening technique, 88% of patients had an excellent or good result with a 7.5% failure rate. In Pasque and Rayan’s7 study, 84% of patients had good or excellent grades after submuscular transposition with a Z lengthening.
EVIDENCE
In an attempt to compare all these procedures, Dellon1 compiled the literature on each procedure. In his article, he reviewed the previous 90 years of literature and concluded, “This study demonstrates that despite more than 50 reported series of patients treated for ulnar nerve compression at the elbow, a collective experience with more than 2000 patients, there are at present no statistically significant guidelines based on prospective randomized studies for choosing one operative technique over another.”1
Dellon1 found that in mild compression, the literature supported nonsurgical management with an expectation of 50% of patients achieving excellent results and almost 100% of patients achieving excellent results with any of the five common surgical procedures. For moderate compression, he noted that the literature suggested the anterior submuscular technique yielded the most excellent results with the least recurrence, and for severe compression, the intramuscular technique yielded the fewest excellent results and the most recurrence.
A meta-analysis of 30 clinical studies from 1945 to 1995 compared patients having nonsurgical management, simple decompression, medial epicondylectomy, subcutaneous, submuscular transposition. Although it appears that none of the studies was a randomized trial, the authors tried to collect information from each patient in each study where possible. The report provides a list of publications evaluating each procedure and is useful to provide historical context to the surgery for cubital tunnel syndrome. Patients were categorized by preoperative staging of severity. Outcomes were scored as “total relief,” “improvement,” “no change,” and “worse.” In minimum stage compression, total relief was experienced by 92% having medial epicondylectomy. The remaining groups were small; however, it was noted only 9% of 22 patients had complete relief after subcutaneous transfer. In moderate stage compression, submuscular transposition yielded 80% complete relief, and in severe stage compression, all the procedures faired poorly with simple decompression providing 26% complete relief and no significant differences except medial epicondylectomy, which had the lowest satisfaction rate at 38% and had no patients with complete relief. In this systematic review, more than 450 patients were analyzed with severe compression.8
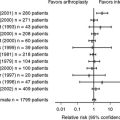
Recently, randomized trials have been used to compare some of the surgical procedures used for cubital tunnel syndrome. In 2005, Bartels and coworkers9 used a randomized trial to compare the outcome of simple decompression versus anterior subcutaneous transposition.
First, the authors used a survey of neurosurgeons in the Netherlands to determine the most commonly performed procedures. From a single center, 152 patients were randomized by a computer-generated randomization list to simple release or anterior subcutaneous transposition. Inclusion criteria included duration of symptoms greater than 3 months, clinical and electrical criteria, and failure of nonsurgical management. Exclusion criteria included diabetes, arthritis of the elbow, and previous surgery on the symptomatic side, among other factors listed in the article. The exact surgical methods used were not detailed in the article; however, the tendency of the ulnar nerve to sublux was noted and found to have no influence on the result. Preoperative severity of compression was recorded. The authors found no influence of the preoperative grade, the extent of muscle weakness, or the duration of symptoms on the probability of improvement, although the analysis of this was not presented. In addition to neurologic grade noted earlier, outcomes were measured using the SF-36 and a Dutch version of the McGill Pain Questionnaire. The authors state the results of both instruments improve with time with no statistical difference at any follow-up interval. No further statistical detail or data from either instrument are reported. A total of 147 participants were included in the analysis. The results were reported as excellent and good in 65% of simple decompression and 70% of anterior subcutaneous transposition. The complication rate was lower in the simple decompression patients at 9.6% compared with 31.1% in anterior subcutaneous transposition. Eighteen of 152 patients were deemed to have unsuccessful surgical results.
In another study, Nabhan and coauthors10 report on a randomized trial of simple decompression compared with subcutaneous transposition of the ulnar nerve. Sixty-six patients were included and randomized using a sealed envelope method. Patients with previous elbow trauma were excluded. Outcomes were measured by a sensory scale, intrinsic motor strength, pain, and nerve conduction velocity. The surgical procedures are described. After a 6- to 9-month follow-up, there were no significant differences between the two groups. The article does not report how many patients experienced complete relief of symptoms and how many failures occurred in each group (Level II).
Both of these randomized trials failed to show any benefit of transposition of the nerve over simple release. In Bartels and coworkers’9 report, neither the preoperative severity of compression nor the tendency of the nerve to sublux over the epicondyle had an effect on the outcome. The Nabhan and coauthors’10 findings are consistent with those of Bartels and coworkers,9 putting into question the need for transposition of the nerve in patients without trauma or elbow pathology.
Biggs and Curtis11 compared “ulnar neurolysis” with submuscular transposition in a randomized, controlled trial. In this study, 44 patients were stratified and randomized. Inclusion and exclusion criteria were documented, and the procedures are described in the article. Using the Louisiana State University Medical Center system, the authors note neurologic improvement in 61% of the neurolysis group and 67% of the transposition group. In medium- and high-grade compression, there was no statistically significant difference in the groups, with 82% improving in the neurolysis group and 68% in the transposition group. Although the numbers are small, the simple decompression group had better results in this more severe degree of compression. Three of 21 patients experienced development of wound infection after transposition, and 0 of 23 after neurolysis. The surgery and the postsurgical evaluations were performed by the lead author, so the study could not be considered blinded with regard to measurement of the results of surgery (Level II).
Gervasio and coworkers12 compared simple decompression versus anterior submuscular decompression in severe cubital tunnel syndrome. Patients were “randomized” based on their hospital reservation number, and one of two surgeons was assigned depending on the procedure. All patients had severe cubital tunnel syndrome, termed Dellon 3, or severe compression. Exclusion criteria are presented in the article. Surgical procedures are described. The postoperative evaluations were performed by a blinded neurologist using the Bishop rating system (see earlier). The results showed that both groups improved to a similar degree with no significant differences in electrical or clinical improvement. Eighty percent of patients had a good to excellent outcome with simple decompression, and 82.9% has a good or excellent outcome with submuscular transposition. Simple decompression yielded 54.3% excellent, 25.7% good, and 20% fair results, whereas anterior submuscular transposition gave 51.4% excellent, 31.4% good, and 17.1% fair results (Level II).
Once again, the two trials failed to show any improvement afforded by transposition of the nerve into the submuscular location over simple decompression of the nerve. This was specifically found in severe compression in the trial that Gervasio and coworkers12 reported. Although that study was not truly randomized, a large proportion of patients with severe compression had good or excellent results after simple decompression.
In a randomized trial of medial epicondylectomy versus anterior transposition in a population of 47 patients, Geutjens and investigators13 found no difference in the results with regard to two-point discrimination recovery or muscle power. A larger proportion of patients was the same or worse after anterior transposition, and fewer transposition patients would have the procedure again. Patients were randomized using sealed envelopes and had one of the two procedures performed by one of two surgeons. Both surgeons performed both procedures. Postoperative evaluation was blinded. The statistical methods are not elaborated in the article (Level II).
A nonrandomized comparative study of 56 patients comparing minimal medial epicondylectomy and anterior subcutaneous transposition similarly found that the two procedures produced similar results.14 The medial epicondylectomy yielded 41% excellent, 45% good, 9% fair, and 5% poor results, whereas the subcutaneous transfer had 41% excellent, 38% good, 18% fair, and 3% poor.
Areas of Uncertainty
Efficacy and Complication Rates of the Procedures.
Do the results of these trials suggest these procedures, the efficacy, and the complication rates would be typical for other surgeons? Our attention is drawn to the cure rate that may be lower and the complication rate including infections that may be higher in these randomized trials than reported in large cohorts performed by other surgeons. For example, the importance of cutaneous nerves crossing the incision in cubital tunnel surgery has been pointed out in the literature.15 The complications of subcutaneous transfer reported by Bartels and coworkers9 could have been reduced by increased attention to this detail.
Similarly, the proportion of patients achieving complete relief of symptoms reported by Bartels and coworkers9 seems low, and in contrast with the systematic review of previous studies, the degree of compression did not appear to influence the results.
Size of Studies
All studies reviewed were small trials, increasing the possibility that chance could play a role in the results. The largest study with Level I evidence9 comparing simple release with subcutaneous transfer had enough power to detect a 25% or greater difference in the results. Those authors found a 13% difference in those patients “cured,” favoring transposition. Biggs and Curtis’s11 study, when evaluating the more severe cases, found the reverse, favoring simple decompression, although the numbers are small. With small studies, the impact of methodologic problems or chance can sway the results of a trial. For example, in at least two of the trials, the measurement of the results was not blinded; in one trial, the allocation was not truly randomized; and in all the trials, the surgery was performed by a limited number of surgeons.
CONCLUSIONS
Based on this review, I believe good to fair evidence exists (grade B, that is, consistent Level I and II evidence) to support simple decompression for cubital tunnel syndrome over transposition of the nerve. This evidence is limited to patients in whom the cubital tunnel syndrome is not secondary to trauma or an anatomic cause at the elbow. The evidence is strongest for use by neurosurgeons to guide their decision making. I believe evidence exists against transposition of the ulnar nerve, during cubital tunnel surgery. Also, I believe no evidence is available to differentiate between simple decompression and medial epicondylectomy in cubital tunnel surgery.
| Summary of Recommendations | |
|---|---|
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATIONS |
| Simple decompression is as efficacious as transposition of the ulnar nerve in cubital tunnel syndrome | B |
1 Dellon AL. Review of treatment results for ulnar nerve entrapment at the elbow. J Hand Surg [Am]. 1989;14:688-700.
2 Kleinman WB, Bishop AT. Anterior intramuscular transposition of the ulnar nerve. J Hand Surg [Am]. 1989;14:972-979.
3 Dellon AL, Schlegel RW, Mackinnon SE. Validity of nerve conduction velocity studies after anterior transposition of the ulnar nerve. J Hand Surg [Am]. 1987;12:700-703.
4 Nathan PA, Keniston RC, Meadows KD: Outcome study of ulnar nerve compression at the elbow treated with simple decompression and an early programme of physical therapy. J Hand Surg [Br] 20;5:628–637.
5 Amako M, Nemoto K, Kawaguchi M, et al. Comparison between partial and minimal medial epicondylectomy combined with decompression for the treatment of cubital tunnel syndrome. J Hand Surg [Am]. 2000;25:1043-1050.
6 Dellon AL, Coert JH. Results of the musculofascial lengthening technique for submuscular transposition of the ulnar nerve at the elbow. J Bone Joint Surg Am. 2004;86-A(suppl 1):169-179.
7 Pasque CB, Rayan GM. Anterior submuscular transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg [Br]. 1995;20:447-453.
8 Mowlavi A, Andrews K, Lille S, et al. The management of cubital tunnel syndrome: A meta-analysis of clinical studies. Plast Reconstr Surg. 2000;106:327-334.
9 Bartels RHMA, Verhagen WIM, van der Wilt GJ, et al. Prospective randomized controlled study comparing simple decompression versus anterior subcutaneous transposition for idiopathic neuropathy of the ulnar nerve at the elbow: Part 1. Neurosurgery. 2005;56:522-530.
10 Nabhan A, Ahlhelm F, Kelm J, et al. Simple decompression or subcutaneous anterior transposition of the ulnar nerve for cubital tunnel syndrome. J Hand Surg [Br]. 2005;30:521-524.
11 Biggs M, Curtis JA. Randomized, prospective study comparing ulnar neurolysis in situ with submuscular transposition. Neurosurgery. 2006;58:296-304.
12 Gervasio O, Gambardella G, Zaccone C, Branca D. Simple decompression versus anterior submuscular transposition of the ulnar nerve in severe cubital tunnel syndrome: A prospective randomized study. Neurosurgery. 2005;56:108-117.
13 Geutjens GG, Langstaff RJ, Smith NJ, et al. Medial epicondylectomy or ulnar-nerve transposition for ulnar neuropathy at the elbow? J Bone Joint Surg Br. 1996;78:777-779.
14 Baek GH, Kwon BC, Chung MS. Comparative study between minimal medial epicondylectomy and anterior subcutaneous transposition of the ulnar nerve for cubital tunnel syndrome. J Shoulder Elbow Surg. 2006;15:609-613.
15 Lowe JB3rd, Maggi SP, Mackinnon SE. The position of crossing branches of the medial antebrachial cutaneous nerve during cubital tunnel surgery in humans. Plast Reconstr Surg. 2004;114:692-696.