Chapter 45 What Is the Appropriate Timing of Prophylactic Stabilization of Osseous Metastases?
Metastatic bone disease continues to challenge even the most experienced orthopedic surgeon. The increased survival rate of patients with carcinoma has led to an increasing population of patients with osseous metastases. Bone is the third most common site of metastasis after lung and liver.1 In up to 25% of patients, metastatic bone disease is the first presentation of carcinoma. Metastasis to bone is common, with 50% of newly diagnosed cancers eventually spreading to bone.2 The most common primary tumors that metastasize to bone are prostate (36%), breast (32%), and lung (14%).2 The most common sites for metastasis to bone are vertebrae, pelvis, ribs, femur, and skull. In as many as 10% of patients with metastases, the primary site is never found. Survival after diagnosis of bone metastasis is related to the primary bone tumor: breast, 34 months; prostate, 24 months; cervix, 18 months; colorectal, 13 months; lung, less than 12 months; and melanoma, 3 months.2 A variation exists in survival related to types and grades of primary tumor.
Plain radiographs of the involved limb in at least two planes form the initial investigation. The metastatic lesion must destroy 30% to 50% of bone and reach a size of 1 cm to be seen on plain radiographs. The characteristic features seen include radiolucent (osteolytic) lesion, although the lesion can be osteoblastic, radiodense, or mixed; minimal periosteal reaction; epicenter in the intramedullary canal; and intracortical/juxtacortical locations are rare. A bone scan demonstrates metastatic lesions on average 3 months before plain radiographs, and it can detect a lesion as small as 2 mm. McNeil3 reviewed 273 patients with known primaries and a positive bone scan. He found that 55% had actual metastases, whereas the other 45% had other reasons: trauma in 25%, infection in 10%, and miscellaneous in 10% of patients. Overall, the diagnosis of metastatic bone disease can be made in 66% of patients with a careful history and physical examination, chest radiograph, and computed tomography (CT) of the chest. An additional 13% can be diagnosed with a CT scan of the abdomen. A biopsy of the skeletal lesion adds a further 8% and allows confirmation in 28% of patients.
EVIDENCE
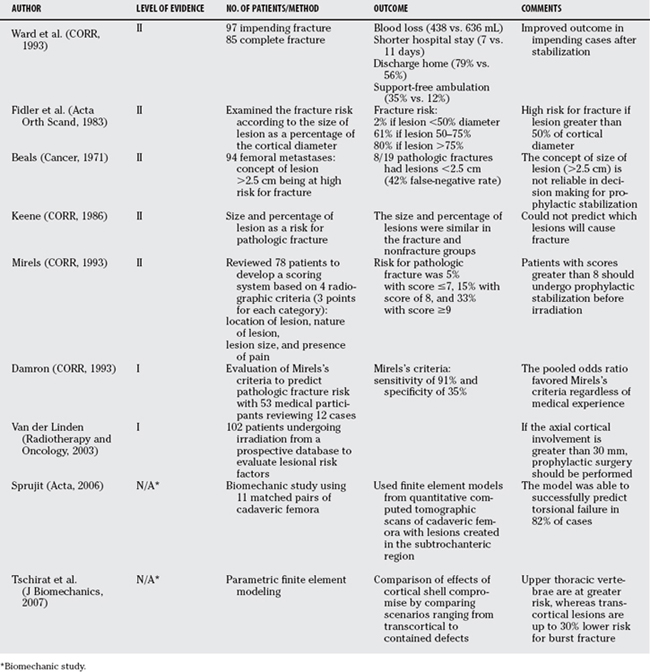
Ward and colleagues4 compared the results of 97 impending fractures compared with 85 complete fractures. In the impending group, there was less blood loss (438 vs. 636 mL), shorter hospital stays (7 vs. 11 days), greater likelihood of discharge home as opposed to an extended care facility (79% vs. 56%), and a greater likelihood of resuming support-free ambulation (35% vs. 12%).4
It has been recommended that femoral metastases can be treated without surgery if they are small (<2.5 cm), less than 50% of the diameter of the cortex, and are in a low-risk location (i.e., not in the pertrochanteric region of the femur)5,6 (Level V). Often, a CT scan of the affected area is valuable in determining the exact size and location of the lesion. These recommendations are controversial, serving only as guidelines, and treatment should be individualized.
Fidler7 examined the concept of greater than 50% cortical diameter as a criterion for operative intervention (Level II). The fracture risk was low (2%) when the lesion size was less than 50% of the diameter. The fracture risk was high (80%) when the lesion was greater than 75% of the diameter. Finally, when the lesion was 50% to 75% of the diameter, there was a 61% incidence rate of fracture.
Beals and coauthors8 reviewed 338 patients with 94 femoral metastases; 8 of 19 with a pathologic fracture had a lesion smaller than 2.5 cm on radiographs (Level II). This was a false-negative rate of 42% for the concept of 2.5 cm being a guideline.
Finally, Keene and coworkers9 could not use the criteria to predict which pathologic fractures would occur in patients with metastatic breast carcinoma to the proximal femur (Level II). The ranges of sizes and percentages of the cortical involvement on plain radiographs were the same for patients with and without fractures.
Several biomechanical studies have been completed to resolve the issue of pathologic fracture risk. Sprujit and researchers10 used finite element models from quantitative CT scans of cadaveric femora with lesions created in the subtrochanteric region. The model was able to successfully predict torsional failure in 82% of cases. Lee also developed a model using quantitative CT combined with engineering beam analysis to predict the load-carrying capacity of femurs with metastatic defects.10a
Roth and colleagues11 used biomechanically based models to predict metastatic burst fracture risk. They examined 92 vertebrae with osteolytic spinal metastases. Specific burst fracture risk was calculated incorporating load-bearing capacity (tumor volume, trabecular bone density, disc quality, and pedicle involvement) and load-bearing requirement (pressure load, loading rate). The models were able to predict fracture in patients at high risk and predict stability in patients at low risk.
Tschirhart and investigators12 were able to use parametric finite element modeling to determine the effects of vertebral level, geometry, and metastatic compromise to the cortical shell on the risk for burst fracture in the thoracic spine. Their findings demonstrate that upper thoracic vertebrae are at greater risk whereas kyphotic motion segments are at a lower risk for burst fracture. In addition, transcortical lesions are at up to 30% less likely to lead to burst fracture.
Mirels13 has proposed a scoring system for diagnosing the risk for impending pathologic fracture. This system objectively analyzes and combines four radiographic and clinical risk factors (that score is 1–3 independently, then added) into a single score. The variables include location (upper, lower extremity, and pertrochanteric); nature of the lesion (blastic, mixed, osteolytic); size of the lesion (<1/3, 1/3 2/3, >2/3 of the diameter of the bone); and pain (mild, moderate, functional). Using the system in a retrospective review of 78 patients (Level II), Mirels13 found that as the score increased to greater than 7, so did the risk for fracture. The actual occurrence of pathologic fracture was 5% with a score of 7 or less, 15% with a score of 8, and 33% with a score of 9 or greater. However, this means that two thirds of the patients will undergo stabilization that will not eventually sustain a pathologic fracture. Mirels13 recommends that patients with scores of 8 or higher should be treated with prophylactic stabilization before irradiation.
Damron performed a critical evaluation of Mirels’s13 criteria for impending pathologic fractures, which involved 53 medical participants of varying degrees of specialty and experience14 (Level II). The participants reviewed 12 actual clinical cases. The pooled odds ratio favored Mirels’ criteria over clinical judgment regardless of experience level. Overall sensitivity was 91%, but the specificity was only 35%.
Van der Linden and coworkers,15 using the randomized Dutch bone metastasis study, followed 102 patients to identify lesional risk factors for fracture who were undergoing irradiation of femoral metastases. The authors conclude that if the axial cortical involvement is greater than 30 mm, prophylactic surgery should be performed (Level I).
PREOPERATIVE EMBOLIZATION OF BONE METASTASES
Once the diagnosis of osseous metastasis is made, any suspicion of hypervascularity should be investigated and treated. Most commonly, the primary tumor renal cell carcinoma, but other primaries such as bronchogenic carcinoma can be associated with neovascularization. Preoperative embolization (POE), used 48 to 72 hours before peripheral or spinal surgery, is a method of reducing potential blood loss at the time of stabilization and can result in dramatic reduction of neovascularization16 (Level IV).
Sun and Lang17 found that blood loss was significantly less when POE resulted in obliteration of more than 70% of the tumor stain (blush on angiogram). Roscoe and researchers,18 as well as Manke and coworkers,19 found that POE was an effective way of significantly reducing blood loss before spinal stabilization for metastatic renal cell carcinoma18 (Level IV).
VENTING BEFORE PROPHYLACTIC STABILIZATION OF FEMORAL METASTASES WITH AN INTRAMEDULLARY NAIL
Most of the research regarding techniques to reduce marrow embolization during femoral manipulation is based on total hip arthroplasty. Heinrich and coauthors,20 in 26 patients undergoing total hip arthroplasty, used a 4.5-mm lateral cortical drill hole (“vent”) distal to the tip of the prosthesis. A significant reduction in air and fat embolism, as well as no change in end-expiratory carbon dioxide, were observed in the vented group20 (Level III). Martin and investigators21 found that proximal and distal vents reduced intramedullary pressure by up to 90% in a cadaveric model. Roth and colleagues11 used a cadaveric model to show a greater than 50% reduction in intramedullary pressure with distal venting in a cadaveric model with proximal metastatic defects. The creation of a distal vent before prophylactic stabilization for femoral metastases is a safe, easy method of reducing marrow embolization22 (Table 45-1).
AREAS OF UNCERTAINTY/CONTROVERSY
General guidelines are difficult in this patient population as a result of many variables including the primary tumor, the location and size of the metastatic lesion, the current medical status of the patient, and the life expectancy of the patient. Determination of the optimal surgical candidate and the method of stabilization remain controversial, especially in the setting of an impending pathologic fracture.23
A low threshold exists for operative intervention of impending pathologic fractures or lesions of the proximal femur. This is related to the high stresses to which the proximal femur is subjected and, therefore, the high risk for fracture.24 The exact method of stabilization is controversial. Lesions or fractures of the femoral neck or head or intertrochanteric fractures are usually managed with hemiarthroplasty. If any pathologic involvement of the acetabulum occurs, then a total hip arthroplasty is indicated. Rarely, lesions in the pertrochanteric region can be stabilized with a hip screw and side-plate device augmented with polymethylmethacrylate (PMMA) cement.
No studies have compared the use of intramedullary nail to plate for stabilization. However, Yazawa and coworkers25 report a 23% failure rate in cases treated with compression screw and plate25 (Level IV). The potential complication of plate fixation is a stress riser at the end of the plate. For this reason, intramedullary nail fixation should be considered when possible to span the entire length of the femur. Most often a nail is utilized that allows screw fixation into the femoral head.24
Preoperative embolization should be undertaken 24 to 72 hours before stabilization of metastases associated with renal cell carcinoma or other hypervascular tumors to reduce the risk for blood loss. Table 45-2 provides a summary of recommendations.
| RECOMMENDATION | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
1 Aaron AD. Treatment of metastatic adenocarcinoma of the pelvis and extremities. J Bone Joint Surg Am. 1997;79-A:917-932.
2 Campanacci M. Bone and soft tissue tumors. New York: Springer-Verlag, 1999.
3 McNeil BJ. Value of bone scanning in neoplastic disease. Semin Nucl Med. 1984;14:277-286.
4 Ward WG, Holsenbeck S, Dorey FJ, et al. Metastatic disease of the femur: Surgical treatment. Clin Orthop. 2003;415(suppl):230-244.
5 Harrington KD. New trends in the management of lower extremity metastases. Clin Orthop.; 169; 1982; 53-61.
6 Harrington KD. Impending pathologic fractures from metastatic malignancy: Evaluation and management. Instr Course Lect. 1986;35:357-381.
7 Fidler M. Incidence of fracture through metastases in long bones. Acta Orthop Scand. 1981;52:623-627.
8 Beals RK, Lawton GD, Snell WE. Prophylactic internal fixation of the femur in metastatic breast cancer. Cancer. 1971;28:1350-1354.
9 Keene JS, Sellinger DS, McBeath AA, et al. Metastatic breast cancer in the femur. A search for the lesion at risk of fracture. Clin Orthop.; 203; 1986; 282-288.
10 Sprujit S, van der Linden JC, Dijkstra PD, et al. Prediction of torsional failure in 22 cadaver femora with and without simulated subtrochanteric metastatic defects: A CT scan based finite element analysis. Acta Orthop. 2006;77:474-481.
10a Lee T. Predicting failure load of the femur with simulated osteolytic defects using noninvasive imaging technique in a simplified load case. Ann Biomed Eng. 2007;35(4):642-650. Epub 2007 Feb 8.
11 Roth SE, Mousavi P, Finkelstein J, et al. Metastatic burst fracture risk prediction using biomechanically based equations. Clin Orthop.; 419; 2004; 83-90.
12 Tschirhart CE, Finkelstein JA, Whyne CM. Biomechanics of vertebral, geometry, and transcortical tumours in the metastatic spine. J Biomech. 2007;40:46-54.
13 Mirels H. Metastatic disease in long bones: A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop. 2003;415(suppl):S4-S13.
14 Damron TA, Ward WG. Risk of pathologic fracture: Assessment. Clin Orthop. 2003;415S:S201-S207.
15 Van der Linden YM, Kroon HM, Dijkstra PD, et al. Simple radiographic parameter predicts fracturing in metastatic femoral bone lesions: Results from a randomized trial. Radiother Oncol. 2003;69:21-31.
16 Stephen DJG. Preoperative embolization of bone metastases. Tech Orthop. 2004;19:49-52.
17 Sun S, Lang EV. Bone metastases from renal cell carcinoma: Preoperative embolization. J Vasc Interv Radiol. 1998;9:263-269.
18 Roscoe MW, McBroom RJ, St. Louis, et al. Preoperative embolization in the treatment of osseous metastases from renal cell carcinoma. Clin Orthop. 1989;238:302-307.
19 Manke C, Bretschneifer T, Lenhart M, et al. Spinal metastases from renal cell carcinoma: Effect of preoperative particle embolization on intraoperative blood loss. AJNR Am J Neuroradiol. 2001;22:997-1003.
20 Heinrich H, Kremer P, Winter H, et al. Transesophageal 2-dimensional echocardiography in hip endoprostheses. Anaesthesist. 1985;34:118-123.
21 Martin R, Leighton RK, Petrie D, et al. Effect of proximal and distal venting during intramedullary nailing. Clin Orthop. 1996;332:80-89.
22 Stephen DJG. Venting the femoral canal. Tech Orthop. 2004;19:49-52.
23 Jacofsky DJ, Papagelopoulos PJ, Sim FH. Advances and challenges in the surgical treatment of metastatic bone disease. Clin Orthop. 2003;415(suppl):S14-S18.
24 Edwards SA, Pandit HG, Clarke HJ. The treatment of impending and existing pathological femoral fractures using the long gamma nail. Injury. 2001;32:229-306.
25 Yazawa Y, Frassica FJ, Chao EY, et al. Metastatic bone disease. A study of the surgical treatment of 166 pathologic humeral and femoral fractures. Clin Orthop Relat Res.; 251; 1990; 213-219.
26 Jung ST, Ghert MA, Harrelson JM, et al. Treatment of osseous metastases in patients with renal cell carcinoma. Clin Orthop.; 409; 2003; 223-231.
27 Roth SE, Rebello MM, Kreder HJ, et al. Pressurization of the metastatic femur during prophylactic intramedullary nail fixation. J Trauma. 2004;57:333-339.