Chapter 90 What Is Role of Computer Navigation in Hip and Knee Arthroplasty?
Achieving the correct rotation and alignment of the implant components is critical for the short- and long-term survival of hip and knee arthroplasty. In total hip arthroplasty (THA), wear,1,2 range of motion,3 and stability4 are all affected by component orientation. In total knee arthroplasty (TKA), authors have shown that knee implants malpositioned by more than 3 degrees had a 24% loosening rate by 3 years after surgery as compared with 3% for correctly aligned implants.5,6
The correct placement of implants is guided by preoperative radiographs and templating, intraoperative anatomic landmarks, and mechanical alignment guides on the instrumentation sets. However, patient positioning on the table is variable, anatomic landmarks are often difficult to reliably identify in arthritic joints, and mechanical alignment guides have not improved accuracy of acetabular positioning.7,8
BACKGROUND
Picard and colleagues9 have classified CAS into active robotic systems, semiactive robotic systems, and passive systems. Active robotic systems are those in which a robot performs some surgical tasks such as drilling and reaming without the direct intervention of the surgeon. Many systems use a preoperative computed tomographic (CT) scan to plan the surgery. These systems are costly and involve complex equipment in the operating room, and thus have not been widely used.
CLINICAL RESULTS
Total Hip Arthroplasty
Achieving the correct abduction and anteversion of the acetabular component could potentially improve the longevity of a THR, improve the range of motion,3 and decrease the dislocation rate.10–12 Lewinnek and coauthors13 recommend an abduction angle of 40 ± 10 degrees and an anteversion angle of 15 ± 10 degrees as the safe zone for cup orientation. Many studies have investigated whether CAS can help improve accuracy in cup placement.
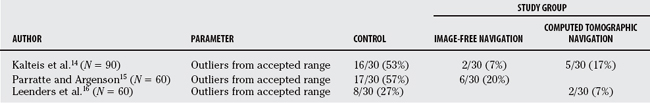
Kalteis and investigators,14 in a prospective, randomized trial, examined CT-based navigation versus imageless navigation versus conventional techniques for positioning of the acetabulum. The data showed that the incidence of component malposition was 53% in the freehand group, 17% in the CT-based group, and 7% with imageless navigation. The authors conclude that navigation significantly improved component alignment (P = 0.003), and there was no difference between CT-based and imageless navigation (P = 0.23). In comparing the mean abduction and anteversion angles between the groups, navigation was significantly better than conventional techniques with no difference between the CT-based versus imageless navigation. Surgical time was increased 8 minutes with imageless navigation and 17 minutes with CT-based navigation with no difference in blood loss among the three groups.
Parratte and Argenson15 compared image-free navigation and freehand techniques for cup placement in a prospective randomized study of 60 patients. They found that 57% of the cups in the freehand group were malpositioned outside the acceptable range as compared with 20% in the navigation group (P = 0.002). When they compared the mean cup angles for both abduction and anteversion between the two groups, there was no significant difference. The mean surgical time was 12 minutes greater for the navigation group.
Leenders and researchers16 undertook a prospective, randomized trial comparing CT-based navigation and freehand techniques for positioning of the acetabular component. CAS surgery led to a significantly improved accuracy for placing the cup within the safe zone of 45 to 55 degrees as compared with traditional methods (P < 0.001). The authors found that only 2 of the 50 patients in the CAS group had abduction angles of cup outside the safe zone.
Other authors have concluded similar findings that navigation helped improve alignment in cup position and reduce the number of outliers from the acceptable range.17,18 Many of these studies are short-term follow-up, and it would be prudent to follow these patients long term to see whether the improved component alignment leads to an improved outcome and survival of the implant. Overall, there is no reported increase in complication rate associated with CAS.
A prospective, randomized study from Germany by Schwieger and colleagues19 compared robotic insertion (ROBODOC) and conventional techniques for total hip replacement. After 24 months of follow-up, the authors conclude that limb-length equality and varus/valgus alignment of the femoral component was improved with the robot (P < 0.001). Recurrent dislocations and subsequently the revision rate was greater in the robotic group (P < 0.001), and the duration of surgery was increased in the robotic group (P < 0.001). No difference was found at 2 years in the Harris hip, Merle d’Aubigné, and the Mayo clinical scores between the two groups. The authors conclude that the 18% dislocation rate in the robot group was due to the abductor muscle deficiencies either from the wide surgical approach needed for the robot or the damage it caused to the tendon during the reaming process, but not from malposition of the components. Furthermore, the authors suggest this technology needs some further development before it can be considered for routine use in THA.
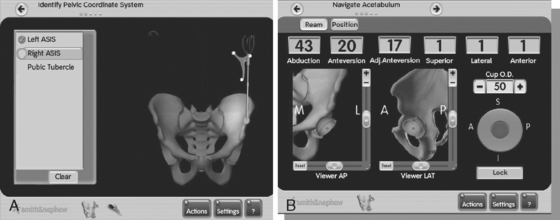
The stability of the femoral implant inserted with ROBODOC was evaluated by Nogler and researchers20 in a prospective, randomized cadaveric study. The authors conclude that there was no difference in femoral component micromotion at the time of insertion; therefore, the robot system did not enhance stability as compared with manual insertion techniques (Table 90-1 and Fig. 90-1).
Total Knee Arthroplasty
Minor implant malpositioning can lead to early wear and loosening, and poorer clinical results. Ritter and coworkers21 have proposed that implants should be aligned in a neutral mechanical axis ±3 degrees varus or valgus for better survivorship. Ten percent of knees lie outside of this range using standard instrumentation. Rotational malpositioning can affect patellar tracking and cause subluxation.22 Traditional techniques for determining femoral component alignment include the epicondylar axis, posterior femoral condyles, and Whiteside’s line.23 Studies have shown that the intraobserver and interobserver reproducibility of these techniques in arthritic knees is poor24–26 Computer navigation has the potential to improve component alignment and also to record information on intraoperative knee kinematics, joint range of motion, and soft-tissue balance.27
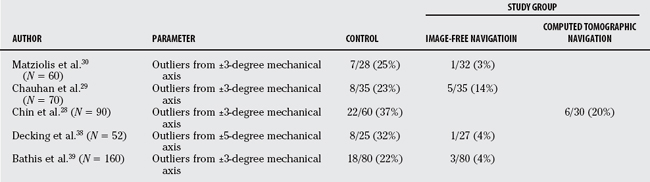
Chin and investigators28 performed a prospective, randomized trial to compare postoperative radiographic alignment of TKA using standard alignment techniques, both intramedullary (IM) and extramedullary, with CAS. The authors found that CAS was more accurate and consistent with placement of the components in both the sagittal and coronal planes as compared with conventional techniques (P < 0.05). When the overall mechanical axes of the limbs were compared, there was no difference among the three groups (P = 0.274). The authors conclude that there are fewer outliers from the acceptable alignment of ±3 degrees with computer navigation. Operative time was significantly greater in the CAS group by 30 minutes (P < 0.001). The volume of drainage in the drains was less in the computer navigation group (P = 0.046); however, the decline in hemoglobin was no different (P = 0.176).
In a randomized prospective trial by Chauhan and coworkers,29 70 patients were randomized to jig-based TKA versus. computer-assisted TKA. They found that computer-navigated knees scored significantly better in terms of femoral coronal plane alignment (P = 0.032), femoral rotation (P = 0.001), and tibial alignment (P = 0.047). Overall, blood loss was less with CAS (P = 0.0001), and the duration of surgery was greater by an average of 13 minutes (P = 0.0001).
Matziolis and investigators30 performed a prospective, randomized study comparing CAS and conventional techniques in TKA. They conclude that computer guidance led to a smaller range of deviation from a neutral mechanical axis as compared with conventional techniques (P < 0.004). Rotational alignment of the tibial and femoral components showed no difference between the two groups. Other authors have reported similar results whereby computer navigation decreases the number of outliers from the acceptable range of alignment.31,32
Another potential benefit to CAS is avoid having to cannulate the IM canals of the femur and tibia, which can potentially lead to decreased blood loss and less systemic fat embolus load. Kalairajah and colleagues33 investigated the incidence of cranial emboli in a prospective, randomized study of 24 patients undergoing either CAS or traditional TKA using intramedullary femoral and tibial guides. In the computer-assisted group, there were, on average, 0.64 emboli detected versus 10.7 in the conventional total knee group (P = 0.003). However, this study did not determine the size of these emboli or the nature of the emboli being fat, air, platelets, or bone. No difference was reported in mean mental scores conducted on the patients on postoperative days 1 or 3.
The issue of blood loss was addressed by Kalairajah and colleagues34 in a prospective, randomized study of 60 patients undergoing TKA with either computer-based navigation or by conventional methods. The mean blood loss in the CAS group was 1183 versus 1747 mL in the conventional group. This difference was statistically significant (P = 0.001). The authors conclude that despite an increase in mean surgical time in the CAS group, 89 versus 74 minutes (P = 0.002), CAS surgery can potentially lead to a decrease in need for blood transfusions.
Keene and investigators35 randomized patients undergoing bilateral medial unicompartmental arthroplasty into two groups, one side with computer navigation and the other with traditional techniques. Preoperative valgus stress view radiographs and clinical assessments were used to determine the desired postoperative coronal alignment. The results demonstrated that the mean variation between the desired alignment and the achieved correction was significantly improved in the navigation group, 0.9 versus 2.8 degrees (P < 0.001). The mean tourniquet time for the navigated knees was 70 minutes as compared with 53 minutes in the non-navigated knees.
A meta-analysis taking restoration of the mechanical axis as an end point was reported by Bauwens and coauthors.36 They included 33 studies, 11 of which were randomized studies for a total of 3423 patients. They conclude that mean values for alignment were no different between the computer navigation group of patients and the conventional technique group. Computer navigation did, however, decrease the risk for malalignment beyond the critical threshold of 3 degrees. Mean surgical time was 23% greater in the navigation group.
The benefits of computer navigation in revision surgery have not been well described in the literature. Sikorski37 reported on 14 knees revised for aseptic failure and concluded that no component was perfectly aligned after surgery and the most difficulty came in femoral rotation. Overall, the author believes that the alignment obtained in computer-assisted revision knee surgery is not as accurate as computer-assisted primary knee arthroplasty (Table 90-2 and Fig. 90-2).
STUDY LIMITATIONS
Computer navigation is an emerging technology whereby the software and hardware components are all continuing to evolve. There is a significant learning curve with computer navigation.17 Potential improvements may be a pinless system to avoid stress risers in the tibia and femur, as well as a computer base with a sterile handle such that it can be adjusted by the surgeon. New systems are using electromagnetic pulses rather than line-of-sight infrared determination of implant position, which may help reduce some of the clutter of the crowded operating room.
The role of computer navigation may be limited to difficult cases with altered anatomy or in association with small incision techniques to improve component alignment. Its consistent use in every primary total joint replacement would likely require a reduction in costs to the hospital, a decrease in added surgical time to the case, and an alternate funding model for the surgeon. Table 90-3 provides a summary of recommendations.
| RECOMMENDATIONS | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION | REFERENCES |
|---|---|---|
CAS, computer-assisted surgery; THA, total hip arthroplasty; TKA, total knee arthroplasty.
1 Schmalzried TP, Guttman D, Grecula M, Amstutz HC. The relationship between design, position and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994;76:677-688.
2 Kennedy JG, Rogers WB, Soffe KE, et al. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530-534.
3 Kummer FJ, Shah S, Iyer S, DiCesare PE. The effect of acetabular cup orientations on limiting hip rotation. J Arthroplasty. 1999;14:509-513.
4 Jolles BM, Zangger P, Leyvraz PF. Factors predisposing to dislocation after primary total hip arthroplasty. J Arthroplasty. 2002;17:282.
5 Fehring TK, Odum S, Griffin WL, et al. Early failures in total knee arthroplasty. Clin Orthop Relat Res. 2001;392:315-318.
6 Jeffery RS, Morris RW, Denham RA. Coronal alignment after total knee replacement. J Bone Joint Surg Br. 1995;73:709-714.
7 Siston RA, Patel JJ, Goodman SB, et al. The variability of femoral rotational alignment in total knee arthroplasty. J Bone Joint Surg Am. 2005;87:2276-2280.
8 DiGioia AM, Jaramaz B, Plakseychuk Ay, et al. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J Arthroplasty. 2002;17:359-364.
9 Picard F, Moody J, DiGioia AMIII, et al, editors. Computer and Robotic Assisted Hip and Knee Surgery. 2004; Oxford University Press: New York; 43-48.
10 Del Schutte HJr, Lipman AJ, Bannar SM, et al. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J Arthroplasty. 1998;13:621-626.
11 Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202-1210.
12 Kennedy JG, Rogers WB, Soffe KE, et al. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear, and component migration. J Arthroplasty. 1998;13:530-534.
13 Lewinnek GE, Lewis JL, Tarr R, et al. Dislocations after total hip-replacement arthroplasties. J Bone Joint Surg Am. 1978;60:217-220.
14 Kalteis T, Handel M, Bathis H, et al. Grifka imageless navigation for the insertion of the acetabular component in total hip arthroplasty: Is it as accurate as CT based navigation? J Bone Joint Surg Br. 2006;88:163-168.
15 Parratte S, Argenson JN. Validation and usefulness of a computer-assisted cup-positioning controlled study system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Joint Surg Am. 2007;89:494-499.
16 Leenders T, Vandevelde D, Mahieu G, Nuyts R. Reduction in variability of acetabular cup abduction using computer assisted surgery: A prospective and randomized study. Comput Aided Surg. 2002;7:99-106.
17 Wixson RL, MacDonald MA. Total hip arthroplasty through a minimal posterior approach using imageless computer-assisted hip navigation. J Arthroplasty. 2005;20(7 suppl 3):51-56.
18 Haaker RG, Tiedjen K, Ottersbach A, et al. Comparison of conventional versus computer-navigated acetabular component insertion. J Arthroplasty. 2007;22:151-159.
19 Schwieger K, Hille E, Morlock MM, et al. Comparison of robotic-assisted and manual implantation of a primary total hip replacement: A prospective study. J Bone Joint Surg Am. 2003;85:1470-1478.
20 Nogler M, Polikeit A, Wimmer C, et al. Primary stability of a robodoc implanted anatomical stem versus manual implantation. Clin Biomech (Bristol, Avon). 2004;19:123-129.
21 Ritter MA, Faris PM, Keating EM, Meding JB. Postoperative alignment of total knee replacement. Its effect on survival. Clin Orthop Relat Res.; 299; 1994; 153-156.
22 Merkow RL, Soudry M, Insall JN. Patellar dislocation following total knee replacement. J Bone Joint Surg Am. 1985;67:1321.
23 Whiteside LA, Arima J. The anteroposterior axis for femoral rotational alignment in valgus total knee arthroplasty. Clin Orthop Relat Res.; 321; 1995; 168-172.
24 Kinzel V, Ledger M, Shakespeare D. Can the epicondylar axis be defined accurately in total knee arthroplasty? Knee. 2005;12:293-296.
25 Jerosch J, Peuker E, Philipps B, Filler T. Interindividual reproducibility in perioperative rotational alignment of femoral components in knee prosthetic surgery using the trans-epicondylar axis. Knee Surg Sports Traumatol Arthrosc. 2002;10:194-197.
26 Jenny JY, Boeri C. Low reproducibility of the intra-operative measurement of the transepicondylar axis during total knee replacement. Acta Orthop Scand. 2004;75:74-77.
27 Siston RA, Gioric NJ, Goodman SB, Delp SL. Surgical navigation for total knee arthroplasty: A perspective. J Biomech. 2007;40:728-735.
28 Chin PL, Yang KY, Yeo SJ, Lo NN. Randomized control trial comparing radiographic total knee arthroplasty implant placement using computer navigation versus conventional technique. J Arthroplasty. 2005;20:618-626.
29 Chauhan SK, Scott RG, Breidahl W, Beaver RJ. Computer-assisted knee arthroplasty versus a conventional jig-based technique. A randomised, prospective trial. J Bone Joint Surg Br. 2004;86:372-377.
30 Matziolis G, Krocker D, Weiss U, et al. A prospective, randomized study of computer-assisted and of implant alignment and rotation conventional total knee arthroplasty. Three-dimensional evaluation. J Bone Joint Surg Am. 2007;89:236-243.
31 Stockl B, Nogler M, Rosiek R, et al. Navigation improves accuracy of rotational alignment in total knee arthroplasty. Clin Orthop Relat Res.; 426; 2004; 180-186.
32 Victor J, Hoste D. Image-based computer-assisted total knee arthroplasty leads to lower variability in coronal alignment. Clin Orthop Relat Res.; 428; 2004; 131-139.
33 Kalairajah Y, Cossey AJ, Verrall GM, et al. Are systemic emboli reduced in computer-assisted knee surgery? A prospective, randomised, clinical trial. J Bone Joint Surg Br. 2006;88:198-202.
34 Kalairajah Y, Simpson D, Cossey AJ, et al. Blood loss after total knee replacement: Effects of computer-assisted surgery. J Bone Joint Surg Br. 2005;87:1480-1482.
35 Keene G, Simpson D, Kalairajah Y. Limb alignment in computer-assisted minimally-invasive unicompartmental knee replacement. J Bone Joint Surg Br. 2006;88:44-48.
36 Bauwens K, Matthes G, Wich M, et al. Navigated total knee replacement. A meta-analysis. J Bone Joint Surg Am. 2007;89:261-269.
37 Sikorski JM. Computer-assisted revision total knee replacement. J Bone Joint Surg Br. 2004;86:510.
38 Decking R, Markmann Y, Fuchs J, et al. Leg axis after computer-navigated total knee arthroplasty: A prospective randomized trial comparing computer-navigated and manual implantation. J Arthroplasty. 2005;20:282-288.
39 Bathis H, Perlick L, Tingart M, et al. Alignment in total knee arthroplasty: A comparison of computer-assisted surgery with the conventional technique. J Bone Joint Surg Br. 2004;86-B:683-687.
40 Widmer KH, Grutzner PA. Joint replacement-total hip replacement with CT based navigation. Injury. 2004;35(suppl 1):S-A84-A89.
41 Nabeyama R, Matsuda S, Miura H, et al. The accuracy of image-guided knee replacement based on computed tomography. J Bone Joint Surg Br. 2004;86:366-371.
42 Kalteis T, Handel M, Herold T, et al. Greater accuracy in positioning of the acetabular cup by using an image-free navigation system. Int Orthop. 2005;29:272-276.