86. Wegener’s Granulomatosis
Definition
Wegener’s granulomatosis (WG) is the systemic vasculitis of small and medium arteries, venules, and arterioles. Large arteries may also be affected.
Incidence
WG is rare; the exact frequency is not known. Recent estimates of incidence put the occurrence at 1:30,000 to 1:50,000 individuals. The age of onset peaks at 40 to 50 years, and it appears equally in males and females, with a strong predilection for Caucasians (>97% of cases).
Etiology
The exact cause of WG is still unknown. Antineutrophilic cytoplasmic antibody (ANCA) has been detected in most cases, and the concentration seems to correlate with the severity of the disease.
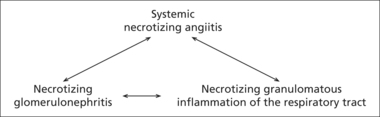 |
| Triad of physiologic features of Wegener’s granulomatosis. |
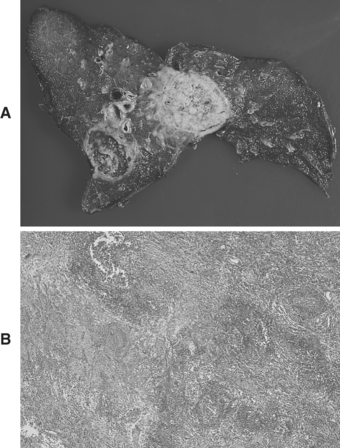 |
| Wegener’s Granulomatosis. The lung parenchyma contains two nodulesshowing central necrosis. |
Signs and Symptoms
• Acute nephritis
• Acute renal failure
• Anorexia
• Arthralgia
• Atelectasis
• Conjunctivitis
• Corneal ulceration
• Cough
• Episcleritis
• Fatigue
• Fever
• Hemoptysis
• Malaise
• Night sweats
• Otitis media
• Pleural effusion
• Pleuritis
• Rapidly progressing glomerulonephritis
• Rhinorrhea
• Sinusitis
• Urine color change
• Weakness
• Weight loss
Medical Management
WG is treated with a combination of prednisone and cyclophosphamide. After control of WG is established, the prednisone is tapered off over a 2-month period; cyclophosphamide is continued for another 6 to 12 months. The patient who does not tolerate the cyclophosphamide may respond more favorably to azathioprine, chlorambucil, or methotrexate. Methotrexate is not given to the patient with pulmonary hemorrhage or fulminate renal failure. Remission may be followed by reappearance of the disease. Relapses usually respond favorably to another regimen of prednisone and cyclophosphamide.
The patient with WG may suffer damage to the nose, subglottic region, trachea, and bronchial tree that may require surgical correction. The patient who progresses to renal failure should be qualified and considered for renal transplant.
Complications
• Acute renal failure
• Acute respiratory failure
• Blindness
• Chronic renal failure
• Deafness
• Massive hemoptysis
• Nasal septum perforation
• Neuropathy
• Saddle nose
• Tracheal stenosis
Anesthesia Implications
Pulmonary and renal effects of this disease must be assessed before any proposed surgical intervention. Blood urea nitrogen (BUN) and creatinine are hallmark preliminary indicators of renal dysfunction.
Tracheal stenosis may be detected using pulmonary flow-volume loop, which detects changes in tracheal caliber. Pulmonary function tests plus spirometry will help indicate whether WG has produced a restrictive pulmonary disorder or an obstructive pulmonary disease.
The patient with WG may have an unexpectedly difficult airway. By outward appearance and cursory physical examination, the patient may appear to have normal airway anatomy. However, there may be a great amount of granulation tissue within the nasal cavity. This highly vascular tissue may impede the insertion of either a nasal airway or passage of a nasotracheal tube. Even if either of these airway devices is able to be inserted, the granulation tissue may be significantly traumatized, resulting in considerable blood loss. Unless absolutely required by the proposed surgical procedure, use of nasal airway devices should be avoided. The epiglottis and oropharynx may be covered with a significant amount of granulation tissue or lesions that may significantly impede placement of an oral endotracheal tube. Even when the glottis is easily visualized, passage of the tube may not be possible because of unforeseen tracheal stenosis. When preparing to anesthetize a patient with WG, the anesthetist should have a variety of sizes of endotracheal tubes within immediate reach along with a difficult airway cart containing numerous airway devices, particularly the laryngeal mask airway (LMA), intubating LMA, and fiberoptic bronchoscope. Use of any of these devices to secure the patient’s airway may traumatize the granulation tissue and produce significant bleeding, further obscuring an already cloudy scene. Finally, all these possibilities may conspire to render the airway unsecurable, at which time emergent surgical intervention may be required to establish the patient’s airway.
The patient with WG is typically treated with relatively long-term administration of corticosteroids. As a result, this patient is likely to require perioperative coverage with corticosteroids.
Because WG can produce significant pulmonary sequelae, either as a restrictive or an obstructive disease, the patient is more prone to air trapping and barotrauma. During positive pressure ventilation, particularly mechanical ventilation, the inspiratory:expiratory ratio (I:E) should be prolonged to levels such as 1:2.5 or 1:3 to allow for better excursion, reduce or prevent air trapping and, thus, reduce or prevent barotrauma.
Regional anesthesia is a possibility for the patient with WG. However, before finalizing such a decision, a neurologic examination should be completed.
The medication and dosage of the neuromuscular blocking agent selected must be adjusted to account for the degree of renal dysfunction present as a result of the WG. Also, the degree of skeletal muscle wasting resulting from associated neuritis calls into question the use of succinylcholine; the prudent course would be to avoid administering succinylcholine.
If there is significant WG-related myocardial muscle and/or cardiac valve involvement, a “normal” concentration of the volatile anesthetics can give rise to an inordinate degree of myocardial depression. The concentration may thus need to be reduced. Other agents known to produce significant myocardial depression, such as propofol, are best avoided in favor of potentially less depressing drugs, such as ketamine or etomidate. The ECG should be closely observed for signs of significant myocardial depression. Direct monitoring of arterial blood pressure may be difficult, depending on the extent of arteritis present.
Chronic Symptoms of Wegener’s Granulomatosis after Remission
• Chronic renal disease
• Cosmetic nasal deformity
• Hearing loss
• Hoarseness
• Tracheal stenosis
• Visual loss
The patient with WG may be leukopenic and anemic as a result of taking the immunosuppressant cyclophosphamide. Cyclophosamide also tends to reduce the available concentration of plasma cholinesterases, which may result in prolonged response to succinylcholine and/or other plasma cholinesterase–dependent drugs.







