Chapter 26 Warts and molluscum contagiosum
Barley-corn, barley-corn, injun-meal shorts,
Spunk-water, spunk-water, swaller these warts,
—Tom Sawyer to Huck Finn on curing warts in The Adventures of Tom Sawyer by Mark Twain
2. Name the common types of warts.
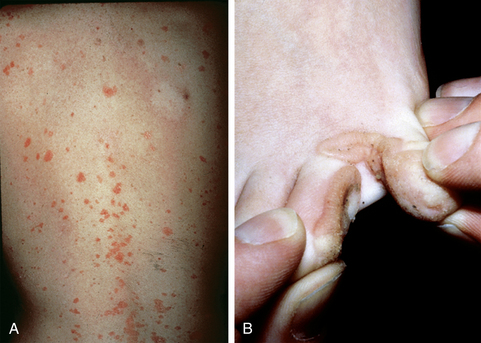
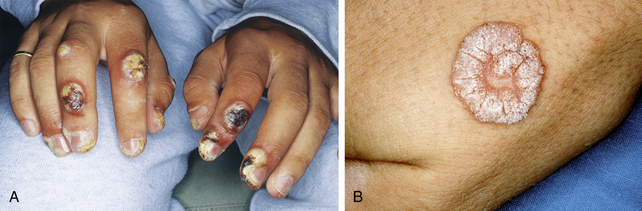
HPV infection is highly specific for epidermis, especially extremities, palms, and soles, but also the scalp and mucosal surfaces such as the mouth, larynx, genital areas, and rectal mucosa. Some types of HPV have a predilection for infection in certain locations in the body (Table 26-1). For example, flat warts are seen mostly on the face and hands of children and are often caused by HPV types 3 and 10 (Fig. 26-1A). Common warts occur most often on the fingers and periungual skin and are commonly due to HPV types 2, 4, and 29 (Fig. 26-1B). Warts in immunosuppressed patients are caused by HPV type 8 and others (Fig. 26-1C).
3. How frequently are the different cutaneous warts seen?
The three types of cutaneous HPV infections are widespread throughout the general population. Common warts, which represent up to 71% of cutaneous warts, occur frequently among school-aged children, with a prevalence of 4% to 20%. Plantar warts are most common among adolescents and young adults and represent about 34% of cutaneous warts. Flat warts are least common (4%) and affect mostly children. Other groups at high risk for cutaneous warts are butchers, meat packers, and fish handlers.
4. Can warts cause cancer?
Certain types of HPV infection have been associated with the development of malignancy. Although bowenoid papulosis is not considered a premalignancy, it may be associated with an increased risk of cervical cancer. Carcinomas of the conjunctiva, cornea, nasal cavities, oral cavity, esophagus, and plantar surface of the foot also have been reported in association with various types of HPV.
Carcinogenic wart types include the following: 16, 18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, and 69.
5. What is epidermodysplasia verruciformis (EV)?
EV is a rare, inherited disorder in which cutaneous HPV infection is generalized and persistent. Most cases are autosomal recessive, but autosomal dominant and X-linked dominant forms are also reported. It is caused by mutations in either the EVER1 or EVER2 genes. The lesions are either flat warts or reddish-brown plaques, often developing in sun-exposed areas (Fig. 26-2A). Malignant change occurs in about 10% of cases, but metastasis is uncommon. HPV types 5 and 8 are most commonly seen in EV patients, although several other HPV types may also been seen.
7. How does a person become infected with warts?
HPV infection occurs after exposure to humans or animals with HPV infection. The most common mode of transmission is through touch or contact from an individual infected with HPV, although HPV may also survive on inanimate objects for unknown amounts of time. Small abrasions or cracks in the skin of exposed persons allow the virus to penetrate. Such infection may commonly occur at a swimming pool, where chlorinated water and rough concrete surfaces may abrade the skin, or at other public places. Genital warts may be transmitted through sexual intercourse. People who work with meat, fish, and poultry also commonly have warts in the hand and forearm area, which are thought to be promoted through microinjuries sustained during processing of animals or fish, as well as from prolonged immersion of the skin in water.
8. Do warts spread?
Yes, especially if they are injured. Such injury may happen if the warts are in a location traumatized by shaving or scratching. This reaction is known as the Koebner phenomenon. (The Koebner reaction is also present in skin conditions that have no known viral cause, such as psoriasis and lichen planus.) Close approximation of two surfaces, where one surface is affected and the opposing surface is unaffected, is also associated with an increased likelihood of spreading (e.g., adjacent toe surfaces; Fig. 26-2B).
11. What is the difference between the Gardasil® and Cervarix® HPV vaccines?
Gardasil® is a quadrivalent vaccine with activity against HPV 16 and HPV 18, which are responsible for approximately 70% of all cervical carcinomas. It is also protective against infection with HPV types 6 and 11, which are nononcogenic HPV strains that produce genital warts in both men and women. In contrast, Cervarix® is a bivalent vaccine with proven protection against the oncogenic strains HPV 16 and 18. There is also some evidence that it produces some protection against other oncogenic HPV types, including HPV 31, 33, and 45.
13. Are plantar warts caused by a special kind of virus? Are they more difficult to treat?
15. Can HPV infection have a hereditary basis?
Except in the case of epidermodysplasia verruciformis, warts are not inherited. However, our immune systems are inherited, and some people seem to have inherited an immune system that places them at risk for acquiring HPV infection. For example, women with HPV involving the cervical and/or vaginal areas have given birth to babies with laryngeal warts.
16. Are some people more susceptible to warts than others?
Immunocompromised individuals, such as those with HIV infection or cancer, or transplant patients on immunosuppressive drugs are more susceptible to warts than others. Sexual intercourse at an early age is a known risk factor for acquiring genital warts. Children with atopic dermatitis may have warts that are more extensive and more difficult to eradicate.
18. How should external genital warts (EGWs) be treated?
Clinical examination is sufficient for evaluation. Treatment goals should be to eliminate symptomatic warts. Sexual partners of patients with EGWs should be evaluated for warts or other sexually transmitted diseases. Women with EGWs should have cervical cytologic screening. HPV detection and EGW typing are not currently required for diagnosis or management. In minors, the presence of EGWs should prompt a consideration of sexual abuse.
Lacey CJ: Therapy for genital human papillomavirus-related disease, J Clin Virol 32:S82–S90, 2005.
19. What methods are available for the treatment of warts?
Over-the-counter methods for eliminating warts include topical applications of acids such as salicylic or lactic acid. These may be in a liquid form or may be incorporated into plasters (Table 26-2). When choosing a treatment plan for warts, the physician’s primary concern should be to not make the treatment worse than the warts. For example, a treatment worse than the disease would be to excise and suture a wart on the weight-bearing surface of the foot and then have the wart recur in the middle of a painful scar. Sometimes, the best treatment is benign neglect. Resistance and recurrence are common with all treatments.
22. Should any treatments be avoided?
• During pregnancy, chemotherapeutic agents, interferon, and retinoids should be avoided, and careful consideration should be given to use of acids and cantharidin. Liquid nitrogen and laser are safe for use during pregnancy.
23. Is there a best way to treat warts?
No single treatment method may be relied upon to eliminate warts permanently. Treatment choice must depend on the age of the patient, location, appearance, and symptoms of the wart:
• Facial: These warts are usually flat and can respond to treatment with topical tretinoin cream or imiquimod. Liquid nitrogen or pulsed dye laser may be used cautiously, but persistent hypopigmentation is an undesired side effect.
• Weight-bearing (plantar): These warts are treated with combinations of acid plaster or liquid acid preparations and/or pulsed dye laser. Glutaraldehyde or intralesional bleomycin may be used in refractory cases.
• Nails: Periungual warts may be treated with topical acids or cantharidin. Liquid nitrogen, often helpful in the treatment of common warts, should be used cautiously here because of the intense pain it causes, as well as risk of persistent nail deformity.
• Genital: Genital warts may be treated with liquid nitrogen, podophyllin or derivatives, topical acids, 5-fluorouracil, imiquimod, or cidofovir. Refractory warts may be treated with interferon. Carbon dioxide laser may also be indicated in some cases.
• Children: Salicylic acid plasters and liquids, cantharidin, liquid nitrogen, and pulsed dye laser have been used successfully. There are recent reports of success using oral cimetidine in prepubertal children with extensive common warts. Many warts regress without treatment. It is speculated that such warts are identified as foreign by the owner’s immune system, which then rejects the wart.
| TREATMENT | WART TYPE | COMMENTS |
|---|---|---|
| Destructive Methods | ||
| Cryotherapy | All | Dyschromia, pain |
| Electrosurgery | Resistant | Scar, recurrence |
| Surgery | Resistant | Scar, recurrence |
| Carbon dioxide laser | Resistant | Scar, recurrence |
| Pulsed dye laser | Resistant | Not readily available |
| Caustic Acids | ||
| Monochloroacetic, dichloroacetic, and trichloroacetic acid | Common | Irritation, blisters, scar |
| Cantharidin | Small, common | Irritation, blisters, hyperpigmentation, fairy ring warts |
| Chemotherapeutic Agents | ||
| Podophyllotoxin* | External genital | Erythema, erosions, ulcers, pain |
| Imiquimod* | External genital | Erythema, burning, erosion |
| Bleomycin (intralesional)* | Common | Pain, nail loss, nail dystrophy, Raynaud’s phenomenon |
| 5-Fluorouracil (topical)* | Flat | Irritation |
| Miscellaneous | ||
| Interferon* | Anogenital | Inject intralesional or intramuscular |
| Contact hypersensitivity | Resistant | Squaric acid |
| Tretinoin (topical)* | Flat | Irritation |
| Glutaraldehyde | Plantar | Brown discoloration, allergy |
| Cimetidine (oral)* | Resistant | Best in children |
| Salicylic acid | Common, plantar | Available over the counter |
| Retinoids* | Immunosuppression | Relapse when drug is discontinued |
| Formalin* | Plantar | Contact sensitivity |
26. Do any warts come from toads?
No. There is no supportive scientific evidence—histologic, viral, or other—that the bumps on the skin of a toad are at all related to warts.
Key Points: Human Papillomavirus Infection
2. Most HPV infections are not carcinogenic, but persistent infections with some genotypes, especially HPV-16 and HPV-18, are associated with a high risk of epithelial neoplasia.
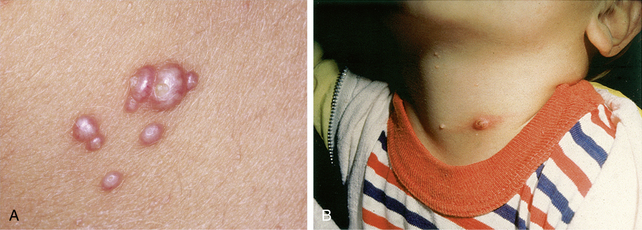
27. Are molluscum contagiosum a type of wart?
No. Molluscum contagiosum is a viral infection of the skin produced by a poxvirus that is more closely related to the virus that produces smallpox. Like warts, they are more common in children and immunocompromised individuals, and can be sexually acquired. They may occur anywhere on the skin surface and present as firm, skin-colored umbilicated papules with a central core of keratin (Fig. 26-4A). Some lesions may demonstrate an intense host response (Fig. 26-4B). Many of the same treatments effective in treating warts are effective in treating molluscum contagiosum.